David J Anschel*
Department of Neurology, St Charles Hospital, 200 Belle Terre Rd, Port Jefferson, NY, USA
*Corresponding Author:
David J Anschel
Department of Neurology
St Charles Hospital, 200 Belle Terre Rd Port Jefferson, NY11777, USA
Tel:(631) 474-6279
E-mail: danschel@amneuro.com
Received date: December 09, 2016; Accepted date: March 29, 2017; Published date: April 03, 2017
Citation: Anschel DJ. Effective Stimulators for Intraoperative Visual Evoked Potentials. J Neurology and Neuroscience 2017, 8:2. doi:10.21767/2171-6625.1000181
Dear Editor,
The review by Rajan et al. [1] provides an excellent introduction to and overview of intraoperative visual evoked potentials. The authors point out many of the shortcomings of certain types of visual stimulators when employed intraoperatively. Generally, these devices consist of reusable goggles with embedded light emitting diodes.
In my experience problems include:
1. A reusable device must be cleaned in between patients.
2. Tightly fitting goggles pose a risk of damaging the eyes.
3. Goggles may fall off the eyes or move intraoperatively and be difficult to reposition once the procedure is underway.
4. The light emitting diodes utilized, tend to be too weak to produce an adequate stimulus.
5. Straps or bands interfere with other aspects of patient care
Rajan et al. speculate that better stimulus methods may be useful to more reliably record intraoperative VEPs.
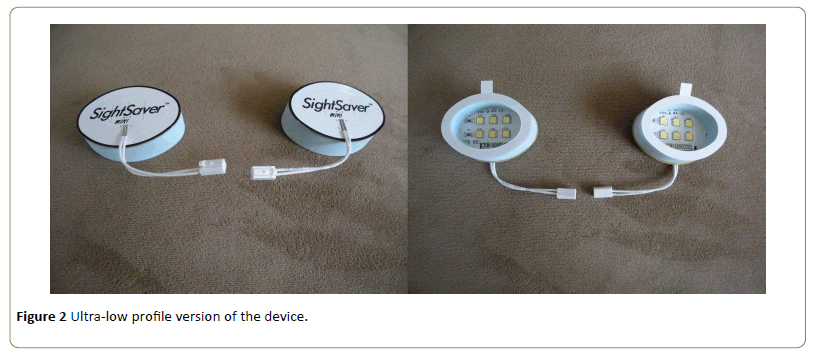
There is an FDA approved visual stimulator, designed for superior performance in the operating room presently available commercially. The SightSaverTM is a novel visual stimulator consisting of: Adhesive foam padding shaped to the contours of the periocular region attached to a printed circuit board with specially selected high intensity light emitting diodes; and a cable interface compatible with standard intraoperative neurophysiology systems (Figure 1).

Figure 1: FDA approved visual stimulator.
This design has several key advantages over standard goggle stimulators:
1. Hygienic advantages - being disposable it eliminates the necessity of cleaning and sterilization in between patients. Reusable stimulating goggles must be carefully cleaned and preferably sterilized after each use in the operating room. Additionally, some bodily fluids are extremely difficult to remove without damaging the reusable stimulating goggles. Using a disposable selfadhesive visual stimulator eliminates such problems.
2. Ocular safety - Reusable stimulating goggles, may damage the eye, especially during procedures where the patient is placed face down. It has even been specifically recommended that any type of goggles be avoided during prone spine surgery as the risk is excessive [2]. SightSaverTM consists primarily of foam padding and actually physically protects the eyes rather than increasing the risk of damage caused by goggles.
3. The form fitting and self-adhesive characteristics of the SightSaverTM result in more effective acquisition of data.Reusable stimulating goggles are fastened to the patient’s head with rubber straps. These straps may interfere with the surgical approach or other monitoring equipment. Additionally, stimulating goggles may be accidentally moved from their original position during the operation, as the head is manipulated. It is often impossible to replace the goggles once the surgery has begun. SightSaverTM does not have a strap and the adhesive properties of the SightSaverTM nearly eliminate any chance of the stimulator moving as the head is manipulated.
4. The specifically chosen high intensity light emitting diodes provide a stronger stimulus than goggles.
An ultra-low profile version of the device is also available (Figure 2). The SightSaverMiniTM does not provide the same level of physical protection to the orbit, but allows for additional intracranial surgical approaches or other situations where less bulk is desirable [3-5].
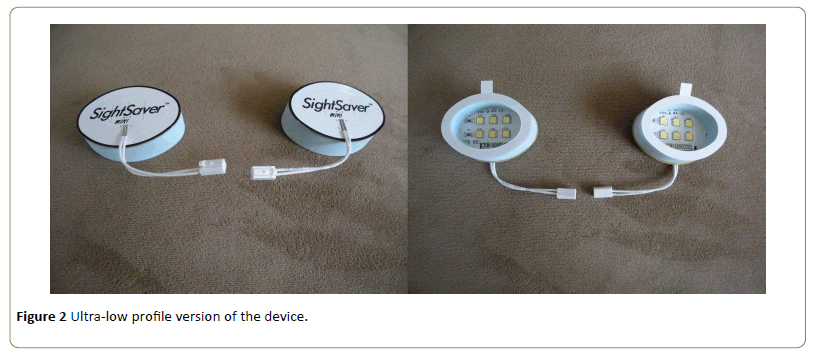
Figure 2: Median and ulnar nerves sensory territories in the palmar surface of the hand. (Please note that TCL is both the roof of the carpal tunnel and the floor of Guyon's canal).
18907
References
- Rajan S, Simon MV, Nair DG (2016) Intraoperative visual evoked potentials: There is more to it than meets the eye. J NeurolNeurosc 7: 1-11.
- Roth S(2007) Visual loss in a prone-positioned spine surgery patient with the head on a foam headrest and goggles covering the eyes: An old complication with a new mechanism. Anesthesia & Analgesia 104: 1185-1187
- Uribe (2016) Comparison of utility and safety of visual evoked potential monitoring using sightSaver™ during spine surgeries. American Society of Anesthesiologists Annual Meeting, October 22-26, Chicago, IL.
- Uribe (2015) Efficacy and safety of detecting subtle visual evoked potential (VEP) changes Using SightSaver™ visual stimulator during spine prone surgery: A pilot study. American Association of Neurological Surgeons, 83rd Annual Scientific Meeting, May 2-6, Washington, DC.
- Uribe (2015) A pilot study to assess the efficacy and safety using SightSaver™ to monitor visual evoked potential (VEP) during spine prone surgery. American Society of Anesthesiologists Annual Meeting, October 24-28, San Diego, CA.