Amin Kordi Yoosefinejad1, Azadeh Shadmehr2*, Ghloamreza Olyaei3, Saeed Talebian4, Hossein Bagheri5, Mohammad Reza Mohajeri -Tehrani6
1PhD student of Physical Therapy, Physical Therapy Department, Rehabilitation Faculty, Tehran University of Medical Sciences (TUMS), Pich-e- Shemiran, Tehran, IR. Iran
2Associate Professor, Physical Therapy Department, Rehabilitation Faculty, Tehran University of Medical Sciences (TUMS), Pich-e- Shemiran, Tehran, IR. Iran
3Professor, Physical Therapy Department, Rehabilitation Faculty, Tehran University of Medical Sciences (TUMS), Pich-e- Shemiran, Tehran, IR. Iran
4Associate Professor, Physical Therapy Department, Rehabilitation Faculty, Tehran University of Medical Sciences (TUMS), Pich-e- Shemiran, Tehran, IR. Iran
5Professor, Physical Therapy Department, Rehabilitation Faculty, Tehran University of Medical Sciences (TUMS), Pich-e- Shemiran, Tehran, IR. Iran
6Assistant Professor, Internal medicine, Endocrinology and Metabolic Research Institute ,5th floor, Shariati Hospital ,Karegar st.,Tehran ,IR. Iran
- *Corresponding Author:
- Azadeh Shadmer
Associate Professor
Physical Therapy Department, Rehabilitation Faculty
Tehran University of Medical Sciences (TUMS)
Pich-e- Shemiran, Tehran, IR. Iran
Email: shadmehr@tums.ac.ir
Keywords
Whole-Body Vibration, Diabetes, Muscle strength, Neuropathy, Michigan Diabetic Neuropathy Score.
Introduction
Type 2 diabetes mellitus (DM) is a prevalent metabolic disease all around the world that affects 1.3% to 14.5 % of Iranian population [1,2].
As the disease progresses over time, neuropathy becomes a common complication. Up to 36% of individuals with non-dependent diabetes mellitus are affected by this condition [3]. While some studies reported a more prevalence among people with type 2 diabetes, others suggest that symptoms are more severe in this population [4]. Muscle strength and balance can be impaired in patients with DM. Diabetic patients had a 17 and 14% reduction of strength of ankle flexors and ankle extensors, respectively [5]. Somatosensory and visual systems are often affected in the presence of DM. Signs and symptoms of peripheral nerve damage may occur in up to 25% of patients with DM after 10 years. The fact that several sensory systems are simultaneously affected in DM makes balance problems and the risk of falling. Yet, proprioceptive deficits of foot and ankle are considered to be the primary sources of balance impairment in DM [6]. In addition to gait and balance impairments, diabetic patients are known to suffer from high risk of injurious falls. Fall-related injuries are supposed to trigger a vicious cycle because of their potential detrimental effects on physical activity levels of the patients [7].
Pain is a common symptom of diabetic neuropathy occurs often symmetrically in the feet and ankles. Peripheral nerves are composed of small and large diameter nerve fibers. Symptoms associated with the large fiber dysfunction are: weakness, tingling, numbness and balance deficit, while those associated with small fiber damage include pin and temperature sensation loss, pain and autonomic dysfunction.
Small fiber involvement initially predominates in early stages of neuropathy [8].
Aerobic exercise is considered as the main strategy to treat type 2 diabetic patients [9]. Besides endurance training, segmental strength training of the major muscle groups is used in the management of diabetic type 2 patients [10]. However, majority of diabetic patients suffer from several problems as obesity, articular complications in addition to adverse effects of diabetes. Whole-Body Vibration training can be a good substitution.
WBV is a new somato-sensory stimulation (SSS) type of exercise that has been emerged in sport training and rehabilitation during the last decade [11,12]. Long term WBV increases muscular strength and balance [12-17]. Recently, a case report showed that WBV has an effect on pain level of a diabetic patient with neuropathy [1].
The purpose of this study was to describe a case of diabetic type 2 patient with peripheral neuropathy suffered from muscular weakness and sleep disturbances and also fear of falling during walking who treated by a six-week WBV training program.
Description of the Case
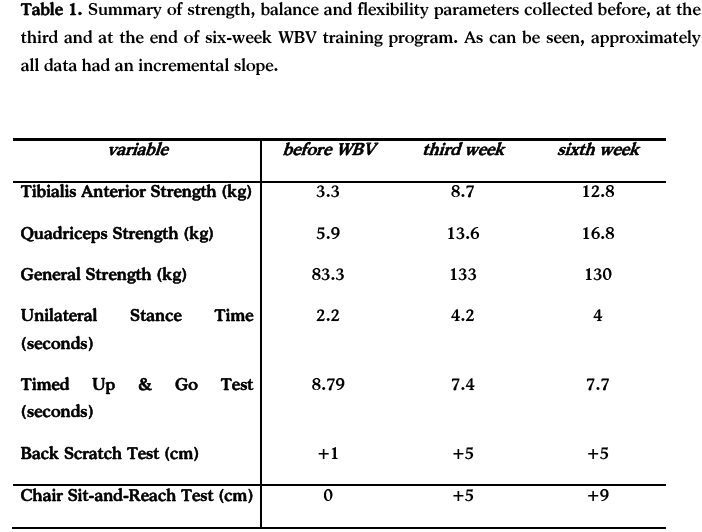
The patient was a 52-year old female with a 10-year history of type 2 diabetes mellitus and a sensation of tingling and numbness in feet from a year ago that awoke her from night sleep with a sense of pain obliged her to change her position continually. Her Body Mass Index (BMI) was 26.1 and Waist to Hip ratio was 0.97. She had moderate degree of neuropathy according to Michigan Diabetic Neuropathy Score (MDNS). When her pain was described by using Visual Analog Scale (VAS), both feet pain was 6 of ten. After her pain was described, muscle strength was assessed by a dynamometer (MIE, medical research ltd., England) locally from Tibialis Anterior and Quadriceps Femoris muscles and also generally by a Back-Leg-Chest dynamometer (BASELINE, USA). Balance was evaluated by Unilateral Stance Test (UST) and Timed Up and Go Test (TUGT). UST is a commonly-used measure of balance capabilities, and a significant predictor of falls [18] and peripheral neuropathy [19]. With the arms folded across the chest, the subject stood on the dominant leg and lifted the other limb approximately 5 centimeters from the medial malleolus of the stance leg. Three experimental trials of UST were recorded and then the average of three was calculated. TUGT is a valid test for mobility and dynamic balance [20]. The participant asked to rise from a chair, walk three meters to a point on the floor at her usual comfortable safe pace, turn around the point and return to her initial seated position. TUGT was scored as the mean time of three subsequent trials. Lower and upper limb flexibility were assessed using back scratch and chair sit-and-reach test. The back scratch test consists in reaching behind the head with one hand and behind the back with the other hand towards the middle finger of hands. The score expressed as the distance (in cm) between the middle fingers. During the chair sit-and-reach test the subject sat on the front edge of a chair and extended her dominant leg straight in front of hip, with ankle in dorsiflexion and heel resting on the floor and reached as far as possible toward the toes. The result of test expressed as the distance (in cm) between the fingers and foot. In both tests the scores were negative when the subject was unable to touch the foot or middle finger and positive when overlap with foot or middle finger was possible [21]. After recording the initial data, the subject exposed to a WBV program which followed overload principle. At the first week the WBV applied at the frequency of 30 Hz, amplitude of 2mm and five thirty-second bouts with one minute elapsed between bouts. For the following two weeks, frequency and amplitude kept the same but exposure duration changed to five 45-second bouts with one-minute interval between bouts and for the last three weeks, subject exposed to five one-minute bouts with one minute interval between bouts. Subject stood barefooted with an even distribution of weight over both feet on the plate with 30 degrees of knee flexion. She was told to contract the muscles of the lower limbs during exposure to vibration and bear weight more on their forefoot to dampen the vibration [22]. She was not allowed to touch the handle of vibrating plate. Data were collected three times; before exposure to WBV, at the end of 3rd week and at the end of 6th week. Data are summarized in Table 1.
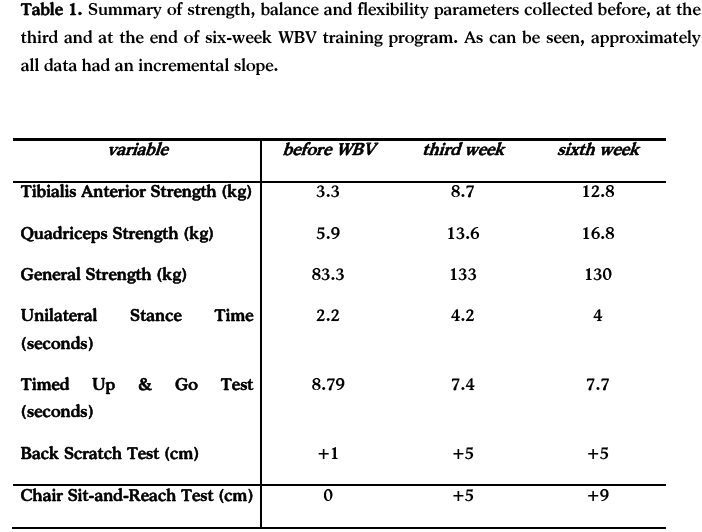
After 6 weeks of WBV training, the patient’s pain in her both feet reduced from 6 to one of ten in VAS and she reported to have a good sleep during night time without being awaken due to feet pain and Paraesthesia. The most interesting finding of our study is the alteration of MDNS score from 13 at baseline to 2 after WBV training. Also, BMI reduced from 26.1 initially to 25.3 and waist to hip ratio declined from 0.97 to 0.89 post training. When the study was about to completed, the patient asked if she could continue the training with WBV or she could purchase her own vibration plate. The patient is very happy with the response and satisfied with her daily activities.
Conclusion
This study demonstrated that WBV training reduces pain and improves muscle strength locally and generally and balance parameters and flexibility in a diabetic type 2 patient with peripheral neuropathy. The interesting finding was that although peripheral neuropathy is believed to be progressive and irreversible [3,23,24], MDNS score reduced significantly in our patient. Although, research on this topic is still in its infancy, the incorporation of WBV to other therapeutic treatment options may be promising. In this case report study, possible placebo and learning effects cannot be completely excluded. Our report is intended to further a discussion about the possible mechanisms of WBV effects on diabetic patients. WBV warrants further investigation over the course of longer, prospective study; in addition long term follow up is required to understand any possible side effects with application of WBV.
3184
References
- Hong J. Whole Body Vibration Therapy for Diabetic Peripheral Neuropathic Pain: A Case Report. Health Science Journal 2011;5(1):66-71.
- nLARIJANI B, ZAHEDI F. Epidemiology of diabetes mellitus in Iran. iranian journal of Diabetes and Lipid Disorders 2002;1(1).
- nPieber K, Herceg M, Paternostro-Sluga T. Electrotherapy for the treatment of painful diabetic peripheral neuropathy: a review. Journal of Rehabilitation Medicine 2010;42(4):289-95.
- nPolydefkis M, Griffin JW, McArthur J. New insights into diabetic polyneuropathy. JAMA: The Journal of the American Medical Association 2003;290(10):1371.
- nAndersen H, Nielsen S, Mogensen CE, Jakobsen J. Muscle strength in type 2 diabetes. Diabetes 2004;53(6):1543.
- nVan Deursen RW, Simoneau GG. Foot and ankle sensory neuropathy, proprioception, and postural stability. The Journal of orthopaedic and sports physical therapy 1999;29(12):718.
- nAllet L, Armand S, De Bie RA, Golay A, Monnin D, Aminian K, et al. The gait and balance of patients with diabetes can be improved: a randomised controlled trial. Diabetologia 2010;53(3):458-66.
- nFink E, Oaklander A. Diabetic Neuropathy. Pain Management Rounds 2005;2(3):309-14.
- nPraet SFE, van Loon LJC. Optimizing the therapeutic benefits of exercise in type 2 diabetes. Journal of Applied Physiology 2007;103(4):1113.
- nLambers S, Van Laethem C, Van Acker K, Calders P. Influence of combined exercise training on indices of obesity, diabetes and cardiovascular risk in type 2 diabetes patients. Clinical Rehabilitation 2008;22(6):483.
- nvan Nes IJW, Latour H, Schils F, Meijer R, van Kuijk A, Geurts ACH. Long-term effects of 6-week whole-body vibration on balance recovery and activities of daily living in the postacute phase of stroke: a randomized, controlled trial. Stroke 2006;37(9):2331.
- nGerodimos V, Zafeiridis A, Karatrantou K, Vasilopoulou T, Chanou K, Pispirikou E. The acute effects of different whole-body vibration amplitudes and frequencies on flexibility and vertical jumping performance. Journal of Science and Medicine in Sport . 2009. Ref Type: Magazine Article
- nRittweger J, Mutschelknauss M, Felsenberg D. Acute changes in neuromuscular excitability after exhaustive whole body vibration exercise as compared to exhaustion by squatting exercise. Clinical physiology and functional imaging 2003;23(2):81-6.
- nBogaerts A, Delecluse C, Claessens AL, Coudyzer W, Boonen S, Verschueren SMP. Impact of whole-body vibration training versus fitness training on muscle strength and muscle mass in older men: a 1-year randomized controlled trial. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2007;62(6):630.
- nBazett-Jones DM, Finch HW, Dugan EL. Comparing the Effects of Various Whole Body Vibration Accelerations on Counter Movement Jump Performance. Journal of Sports Science and Medicine 2008;7(1):144-50.
- nTorvinen S, Kannus P, SIEV NEN H. Effect of four-month vertical whole body vibration on performance and balance. Medicine & Science in Sports & Exercise 2002;34(9):1523.
- nPrisby RD, Lafage-Proust MH, Malaval L, Belli A, Vico L. Effects of whole body vibration on the skeleton and other organ systems in man and animal models: what we know and what we need to know. Ageing research reviews 2008;7(4):319-29.
- nHurvitz EA, Richardson JK, Werner RA, Ruhl AM, Dixon MR. Unipedal stance testing as an indicator of fall risk among older outpatients. Archives of physical medicine and rehabilitation 2000;81(5):587-91.
- nHurvitz EA, Richardson JK, Werner RA. Unipedal stance testing in the assessment of peripheral neuropathy. Archives of physical medicine and rehabilitation 2001 Feb;82(2):198-204.
- nPodsiadlo D, Richardson S. The timed" Up & Go": a test of basic functional mobility for frail elderly persons. Journal of the American geriatrics Society 1991;39(2):142.
- nBautmans I, Van Hees E, Lemper J, Mets T. The feasibility of whole body vibration in institutionalised elderly persons and its influence on muscle performance, balance and mobility: a randomised, controlled trial. Journal of Sports Science and Medicine 2008;7:144-50.
- nAbercromby AFJ, Amonette WE, Layne CS, MCFARLIN BK, HINMAN MR, PALOSKI WH. Vibration exposure and biodynamic responses during whole-body vibration training. Medicine & Science in Sports & Exercise 2007;39(10):1794.
- nEmam AA, Gad AM, Ahmed MM, Assal HS, Mousa SG. Quantitative assessment of posture stability using computerised dynamic posturography in type 2 diabetic patients with neuropathy and its relation to glycaemic control. Singapore Med J 2009;50(6):614-8.
- nHijmans JM, Geertzen JH, Zijlstra W, Hof AL, Postema K. Effects of vibrating insoles on standing balance in diabetic neuropathy. Orthotic Interventions to Improve Standing Balance in Somatosensory Loss 2008;45:1442-50.