Research Article - (2023) Volume 17, Issue 11
Elastography as a Method for the Detection of Breast Cancer
Juan Farak Gomez1*,
Andres Felipe Diaz Munoz2,
Heyman Bravo Dominguez3,
Maria Carolina Causil Galvis4,
Sarly Katiana Serrano Medina5,
Lilian Paola Navarro Mercado6,
Diana Carolina Gonzalez Sotelo7,
David Alejandro Guzman Sanchez8,
Irina Alejandra Vallejos Diaz8 and
Juan Abraham Gonzales Albarracin9
1Department of Medicine, Rafael Nunez University, Cartagena de Indias, Colombia
2Department of Radiology, Pontifical Catholic University, Rio de Janeiro, Brazil
3Department of Oncology, Belgorod State University, Belgorod, Russia
4Department of Medicine, University of Sinu, Monteria, Colombia
5Department of Medicine, University of Magdalena, Magdalena, Colombia
6Department of Medicine, San Martin University Foundation, Atlantico, Colombia
7Department of Medicine, Bogota University Foundation of Health Sciences, Bogota, Colombia
8Department of Medicine, UTE University, Quito, South America
9Department of Medicine, Peruvian University of Applied Sciences, Peru, South America
*Correspondence:
Juan Farak Gomez, Department of Medicine, Rafael Nunez University, Cartagena de Indias,
Colombia,
Email:
Received: 21-Apr-2022, Manuscript No. IPHSJ-23-12742;
Editor assigned: 26-Apr-2022, Pre QC No. IPHSJ-23-12742 (PQ);
Reviewed: 10-May-2022, QC No. IPHSJ-23-12742;
Revised: 01-Sep-2023, Manuscript No. IPHSJ-23-12742 (R);
Published:
29-Sep-2023
Abstract
Breast cancer is a disease characterized by the increase and lack of control in the growth of mammary epithelial cells. In recent years, research has been carried out on new technologies with the aim of being more precise and less radical in the methods used for the diagnosis of breast cancer, where a new use of ultrasound based on the properties of elastic tissues emerged, a technology that uses the name of elastography, which greatly improves the accuracy of diagnosis, the development and application of elastography in the breast, it has made it possible to characterize the elasticity of lesions detected by B-mode (fundamentally nodules) and in certain cases to raise or lower the degree of suspicion of lesions initially assessed by B-mode and color doppler, for breast cancer, has been shown that elastic ultrasound provides information on prognosis and response to neo adjuvant therapy, considering that cancer breast is a heterogeneous disease. Prognostic factors are represented by histological type, tumor size, histological grade, axillary lymph node metastasis and lymphatic vascular invasion, considering the above, when using this technique for early diagnosis, assess prognosis and grade of malignancy of the patients, thus achieving timely treatment which will allow a decrease in the morbidity and mortality of these patients.
Keywords
Elastography; Breast cancer detection; Breast
cancer; Mammary epithelial cells
Introduction
Breast cancer is a disease characterized by an increase and
lack of control in the growth of mammary epithelial cells, it
represents one of the main causes of death in women, many of
these cancers are discovered by tumors found incidentally by
the patient or on routine physical examination and in more
advanced cases with manifestations such as fixation of the mass
to the chest wall or overlying skin, satellite nodules or skin
ulcers, skin edema caused by intrusion of cutaneous lymphatics
(skin of orange), the usually exaggerated skin marks, the fixed or
hard axillary lymph nodes indicate the spread of the tumor and
the presence of inflammation of the superior or subclavian
lymph nodes, associated with risk factors such as age,
gynecological, family history, diet, radiotherapy and genetic
changes associated with the appearance of breast cancer,
according to statistics it is established that one every ten women
will develop breast cancer at some point in her life, however,
with the current increase in the use of mammography and
ultrasound, it has allowed an increase in breast cancer diagnoses
in less serious stages [1].
In recent years, research has been carried out on new
technologies with the aim of being more precise and less radical
in the methods used for the diagnosis of breast cancer, where a
new use of ultrasound based on the properties of elastic tissues
emerged. A technology that uses the name of elastography,
which greatly improves the accuracy of diagnosis, first described
in 1987 by Krouskop, based on the theory that soft tissues in the presence of malignancy present alterations and morphological
changes leading to a deformation process.
The development and application of elastography in the
breast has made it possible to characterize the elasticity of
lesions detected by B-mode (fundamentally nodules) and in
certain cases raise or lower the degree of suspicion of lesions
initially assessed by B-mode and color doppler [2].
This method has proven to be useful by adding information
on the structure of the breast cancer property to morphological
data provided by grayscale ultrasound, it is a method used to
evaluate the level of hardness or elasticity of a section of an
organ or nodule, through the tension and compressibility
produced by the ultrasound waves in the body's tissues in real
time.
Elastography features of breast nodules provide additional
tools for morphologic features, which can improve diagnostic
specificity and efficiency. The greatest utility of elastography has
been shown in lesions classified as Bi-Rads 3 (possibly benign
lesions), elastography is also more useful in circumscribed
cancers and are categorized as possibly benign B-mode lesions.
These localized cancers can be identified as suspicious by 2DSWE,
thus subsequently recommending a biopsy, considering
the breast to be suspicious. These lesions found by this
technique are classified using a scale, the most used elasticity
scale is the UENO, which defines a score or score between 1 and
5, which has greater elasticity when there is no elasticity.
Lesions with a score between 1 and 3 are considered benign, if
the score is 4 or 5, it is considered malignant [3].
There are two main types of elastography, quantitative (shearwave)
and qualitative (strain). Quantitative elastography sends
micropulses to measure tissue displacement independent of
applied acoustic pressure with minimal energy levels for
different tissues. So, it creates an organization chart of
displacement relative to adjacent structures. Qualitative
techniques indicate the existence of hardness in the area of
interest. These qualitative parameters focus on showing relative
hardness between different areas, that is, they separate the
hard from the soft tissues and can distinguish the presence of a
lump. The information obtained is presented by means of
contrast images on a scale of colors that indicate hardness and
softness. This diagnostic alternative is 100% effective when
there is no cancer, which avoids unnecessary biopsies and it is
92% effective when the cells are malignant. In the latter three, a
biopsy is recommended [4].
Elastography should not be used to avoid biopsy of nodules
classified as BI-RADS 4B or C or BI-RADS 5 (highly indicative of
malignancy), nor should it be recommended for nodules
classified as BI-RADS 2 (usually benign). For breast cancer, elastic
ultrasound has been shown to provide information on prognosis
and response to neoadjuvant therapy, considering that breast
cancer is a heterogeneous disease. Prognostic factors are
represented by histological type, tumor size, histological grade,
axillary lymph node metastasis and lymphatic vascular invasion,
considering the above, when using this technique for early
diagnosis, assess prognosis and grade of malignancy of the patients, thus achieving timely treatment which will allow a
decrease in the morbidity and mortality of these patients [5].
Materials and Methods
To carry out this article, a bibliographic search was carried out
in various databases such as Elsevier, Scielo, Medline, PubMed,
ScienceDirect and Ovid, thus selecting original articles, case
reports and bibliographic reviews from 2008 to 2021, but more
extensive bibliographies were used. Old 2000-2007 due to its
weight and information necessary to carry out this work, in
Spanish and English using MeSH terms: Elastography, breast
cancer detection, breast cancer. Thus including all the
documents that will deal with elatography as a method for the
detection of breast cancer and information related to it, the data
found were between 15-40 records, thus using 30 articles for the
preparation of this document [6].
Results
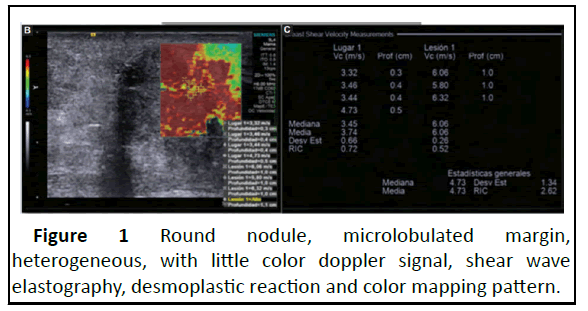
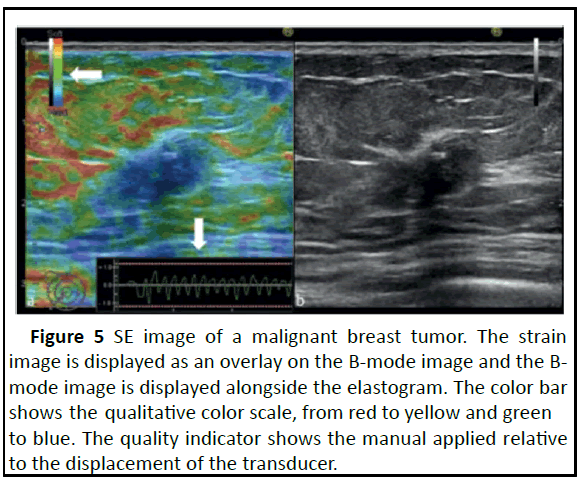
Santos Aragon, et al., have compared the use of conventional
ultrasound versus elastography in the mammary gland with
respect to a benign solid nodule and a malignant nodule. Where
it was observed that, in a benign nodule, such as fibroadenoma,
with elastography, it is observed as an area of greater rigidity
typically smaller than the limits of the lesion. In elastography it is
visualized with a bull's-eye appearance, bright posterior
enhancement or with an aliasing effect. In addition, a
complicated cyst can be differentiated from a solid mass, the
propagation of shear waves does not occur in cysts, in which it
provides values of zero (Figure 1) [7].
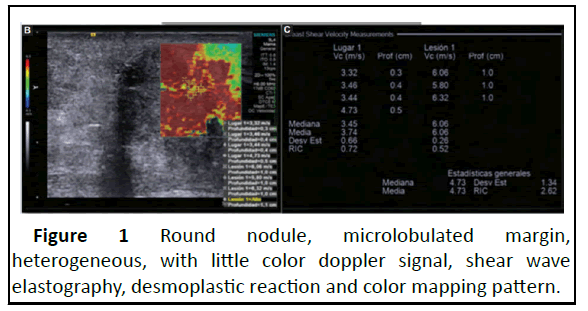
Figure 1: Round nodule, microlobulated margin,
heterogeneous, with little color doppler signal, shear wave
elastography, desmoplastic reaction and color mapping pattern.
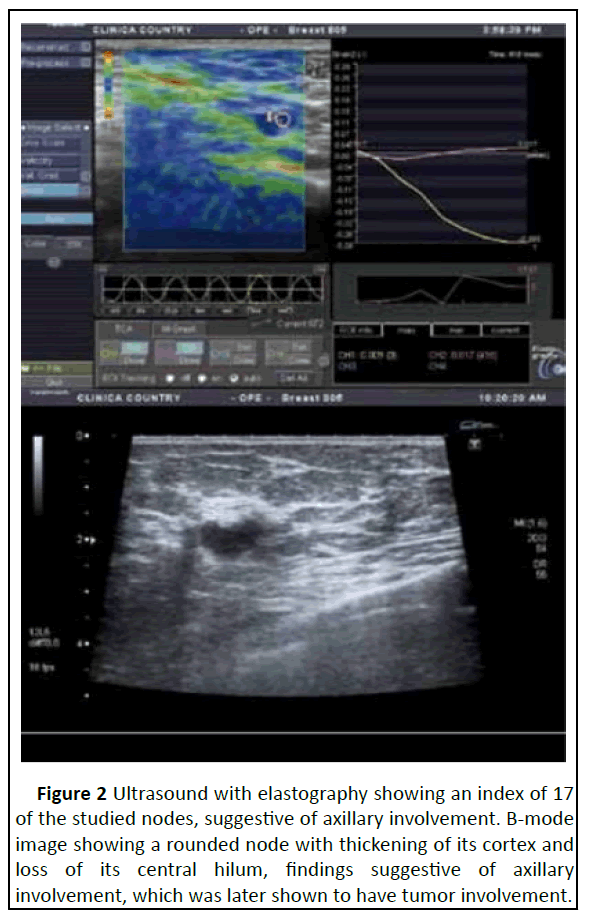
In a study of 101 confirmed invasive breast cancers, Evans, et
al. They showed that high mean stiffness on shear wave
elastography was significantly correlated with high histologic
grade, large invasive size, nodal involvement and vascular
invasion (Figure 2).
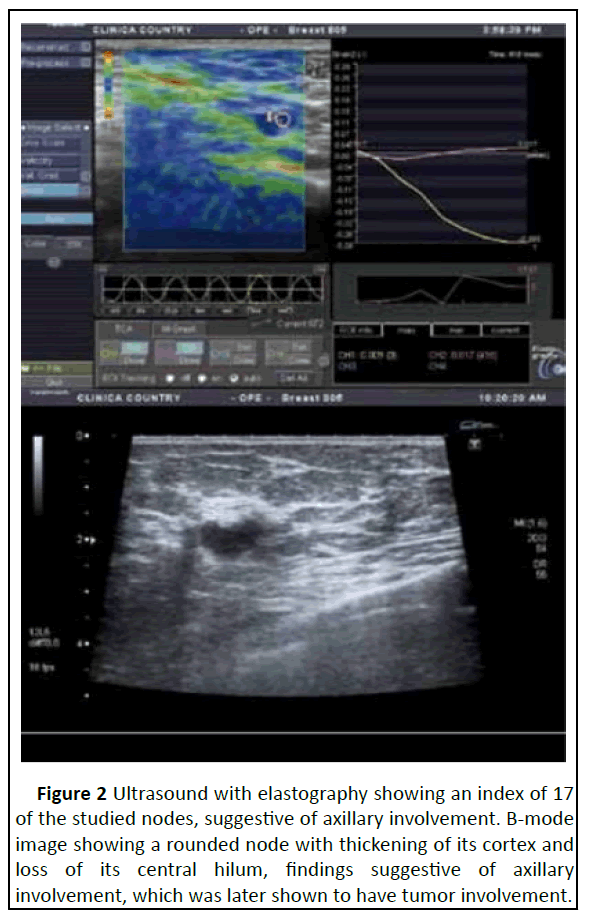
Figure 2: Ultrasound with elastography showing an index of 17
of the studied nodes, suggestive of axillary involvement. B-mode
image showing a rounded node with thickening of its cortex and
loss of its central hilum, findings suggestive of axillary
involvement, which was later shown to have tumor involvement.
In a study carried out in 2013 with 24 women, it was found
that the frequency of axillary metastatic disease was 50%,
finding 17 patients with positive elastography and 12 with
confirmed histopathological involvement. The sensitivity of
elastography in this study was 100% with a specificity of 58%
and the combined use of elastography and ultrasound
demonstrated a sensitivity and specificity of 100% [8].
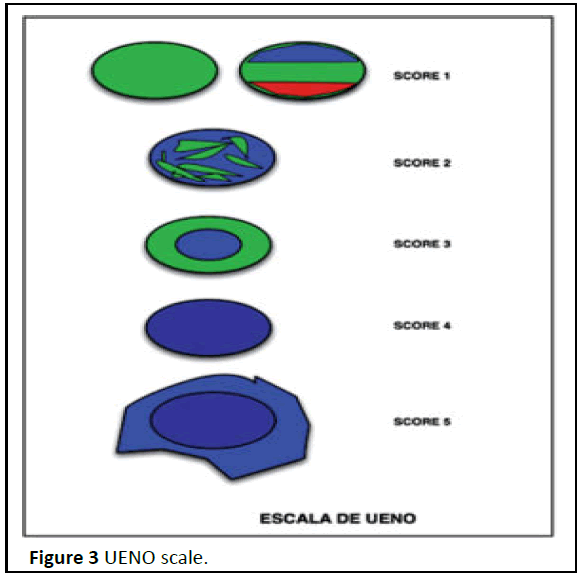
Equivalence between the BIRADS classification and the UENO
classification has been established in different studies,
considering the cut-off point between benign/malignant lesions
between elastographic scores 3 and 4. The results of the mean
scores of benign and malignant lesions in the different published
series are similar (they range between 4.2 and 3.9 for malignant
cases, between 2.1 and 1.8 for benign cases and between 3.7
and 3.3 for ductal carcinoma in situ) and in all cases it is stated
that these differences in elasticity between benign and
malignant lesions are significant. Equivalence with the BI-RADS
classification is made considering that BI-RADS 2 lesions
correspond to elastography scores 1 and 2 and the rest of the
lesions correspond unequivocally to elastography scores (Figure
3).
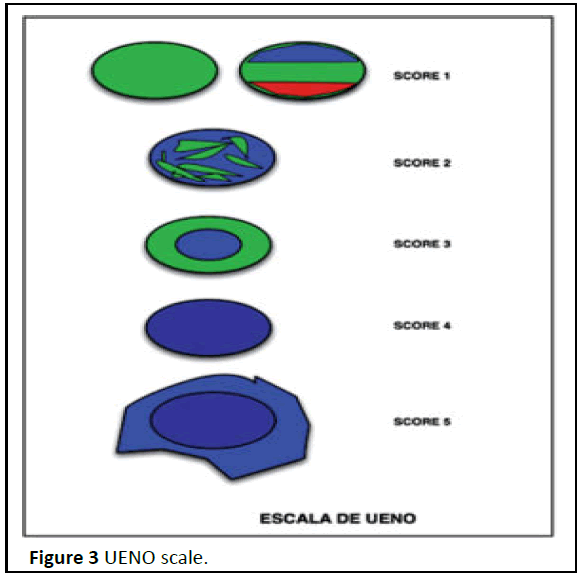
Figure 3: UENO scale.
Diagnostic validity analyzes of elastosonography compared to
ultrasound indicate that the technique shows equal or better
results than B-mode ultrasound. The specificity values of
elastography are usually better than those of B-mode
ultrasound, which is why many authors propose that
elastography improves the rates of false positive results of Bmode
ultrasound. The comparison of the diagnostic
performance of both techniques is limited by the fact that the
elastographic image is always superimposed on the B-mode
image, introducing an interpretation bias [9].
In a meta-analysis carried out in 2018, it was found that the
main use of introducing elastography in clinical practice could be
to reduce the number of unnecessary biopsies. These pose a
problem for the patient, even from an emotional point of view,
in addition to an economic cost for health systems. Other
indications for elastography in breast cancer described in the
literature could be the evaluation of the intraductal component
of the cancer because it does not present as a mass, the
evaluation of the response to neoadjuvant chemotherapy and
the study of axillary lymphadenopathies for which elastography
in real time it seems more sensitive than palpation and
ultrasound. In this meta-analysis, 8 meta-analyses published
between 2011 and 2017 were included. They have studied
different forms of elastography, from compression elastography
and real-time elastography to various quantitative modalities.
The number of patients included in the studies ranged between
1,245 and 5,397 and the number of breast lesions between
1,408 and 5,838. In all of them, the presence of great
heterogeneity between studies was detected. The diagnostic
parameters were calculated for the different qualitative and
quantitative techniques and depending on the way of
interpreting the test (color pattern, SR, length ratio) and have
ranged from 0.83 to 0.94 for the added sensitivity, for the
aggregate specificity between 0.81 and 0.93 and the area under
the SROC curve between 0.84 and 0.96. In general, no significant differences were found between the diagnostic capacity of the
different elastographic techniques [10].
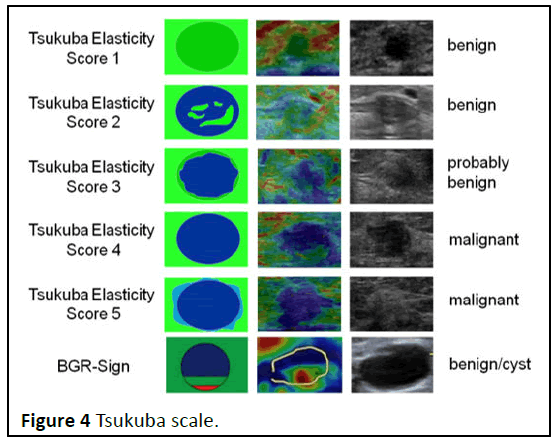
Elastography can be seen as a method used to make
diagnoses, based on ultrasound, it allows evaluating the
elasticity or rigidity of a fragment of an organ or nodule that is
subjected to study, focusing on the tension and compressibility
produced by pressure with the transducer and changes of the
ultrasonic waves of the tissues of the evaluated organ. This
technique can be considered as innovative in ultrasonography, it
allows studying the hardening of a tumor, using quantitative
values expressed in numerical units called kilopascal (kPa).
Establishing an estimate of stiffness in the examined nodule,
depending on the number of kPa, which increases the
specificity; elastography can be applied to any type of body
structure that can be compressed, five degrees of elasticity are
estimated on the tsukuba scale, qualitative elastography of
mammary masses (Figure 4).
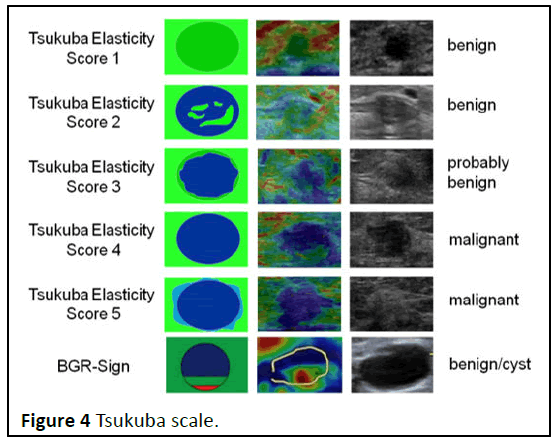
Figure 4: Tsukuba scale.
Elastography has higher specificity but lower sensitivity than
B-mode images when evaluated separately. A meta-analysis of
the Tsukuba score of 29 studies using a cutoff between three
and four in 5,511 breast tumors found a mean sensitivity and
specificity of 79% and 88%, respectively. In another metaanalysis
of nine SR studies in 2087 tumors, the mean sensitivity
and specificity were 88% and 83%, respectively. SWE and pSWE
have shown good sensitivity and specificity in differentiating
benign from malignant breast lesions in a recent meta-analysis
[11].
Several studies have reported the diagnostic benefits of
combining B-mode imaging with SE or SWE, but the
combinations have not been performed consistently. Therefore,
a recommendation or guideline on how to combine
elastography and BI-RADS scores is not yet available. By
combining elastographic evaluations with B-mode BI-RADS
scoring, either sensitivity or specificity can be improved
compared to B-mode imaging alone, depending on the method
of combining the two diagnostic tests. When elastographic
evaluations are used to alter the initial BI-RADS classifications, primarily class 3 and class 4 are considered for re-evaluation, as
these are the BI-RADS classes with the highest number of false
negatives and false positives, respectively. Combining B-mode
imaging with elastography can improve the specificity of breast
tumor evaluation, which is low on the BI-RADS score, without
significantly lowering sensitivity (Figure 5).
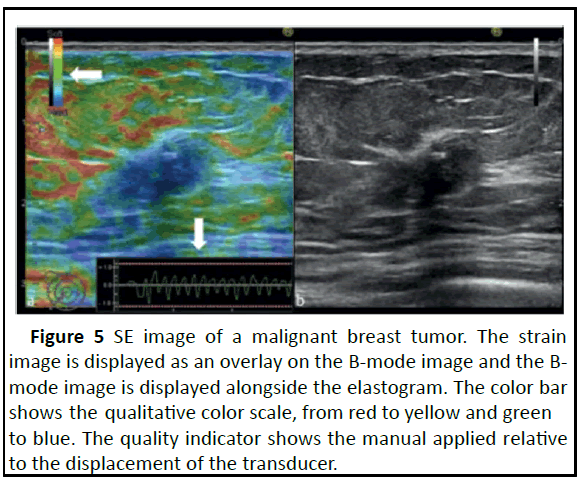
Figure 5: SE image of a malignant breast tumor. The strain
image is displayed as an overlay on the B-mode image and the Bmode
image is displayed alongside the elastogram. The color bar
shows the qualitative color scale, from red to yellow and green
to blue. The quality indicator shows the manual applied relative
to the displacement of the transducer.
It should ideally be between the two red dots. The rate of
compressions can be seen on the x-axis, where the distance
between the two white markers is one second. The tumor is
blue on the elastogram, while the surrounding tissue is red,
yellow and green (mild and intermediate stiffness). On B-mode
image, a 17 mm, nearly oval, hypoechoic tumor with irregular
borders, calcifications, mild shadowing and invasion of
surrounding adipose tissue and Coope’s ligament is seen. The
tumor was classified as BI-RADS 5. Histopathology showed
invasive ductal carcinoma.
In a 2019 study where a total of 373 were included, 196 had
benign lesions and 177 had malignant lesions based on
pathology results. Detailed demographic and pathologic types of
lesions. When the TS and SR values of malignant and benign
breast lesions were analyzed, we found that malignant lesions
usually had higher TS (p<0.001) and RS (p<0.001) than benign
lesions. SR demonstrated signi icantly better performance
than TS in distinguishing malignant from benign lesions. The
AUCs for TS and SR were 0.902 and 0.995,
respectively. Strain elastography achieved a sensitivity of
96.0%, a speci icity of 98.5%, a positive predictive value of
98.3% and a negative predictive value of 96.5% in
differentiation. Meanwhile, with the best cutoff value at 2.5,
the TS yielded a sensitivity of 93.8%, a speci icity of 80.6%, a
positive predictive value of 81.4% and a negative predictive
value of 93. 5% in the differentiation between benign and
malignant tumors (Table 1).
| Characteristcs |
Benign (n=196) |
Malignant (n=177) |
P value |
| Age (years) |
49.9 ± 11.5 |
50.6 ± 10.9 |
0.54 |
| Final diagnosis; n (%) |
|
|
|
| Fibrocystic changes |
9 (4.6) |
- |
- |
| Plasma cell mastitis |
39 (19.9) |
- |
- |
| Introductal papilloma |
23 (11.7) |
- |
|
| Fibroadenoma |
57 (33.3) |
- |
|
| Mastopathy |
48 (25.1) |
- |
|
| Sclerosing mastopathy |
20 (10.0) |
- |
|
| Infiltrating ductal carcinoma |
- |
76 (42.9) |
|
| Malignant phyllodes tumor |
- |
20 (11.3) |
|
| Mucinous carcinoma |
- |
16 (9.0) |
|
| Invasive lobular carcinoma |
- |
65 (36.7) |
|
| TS |
1.86 ± 0.98 |
3.63 ± 0.77 |
<0.001** |
| SR |
1.67 ± 0.51 |
4.8 ± 2.55 |
<0.001** |
Table 1. Patient demographics, histopathologic diagnosis and imaging biomarkers for patients with benign breast and malignant lesions (n=373).
Discussion
Technological advances have been developed in the three
methods mentioned, which has allowed an improvement in the
detection, characterization, management of injuries and followup
of patients. Breast ultrasound is widely used as a diagnostic
tool to characterize nodules detected on mammography,
evaluation of palpable areas, suspicious discharge through the
nipple and guidance for invasive procedures. At the same time,
we can observe that, in addition to ultrasound, the development
and application of elastography in the breast has made it
possible to characterize the elasticity of the lesions detected by
means of B mode, where we mainly look for nodules and in
certain cases, raise or lower the degree of suspicion of lesions
initially. Assessed by B-mode and color doppler.
Physical examination of the breast by palpation can guide
towards benign and malignant pathology, since breast cancer is
harder and more fixed than the adjacent normal breast
parenchyma, unlike benign lesions that are soft and mobile.
Although breast palpation can guide, it is sometimes difficult to
reproduce and its main limitation is based on its low sensitivity
and diagnostic accuracy.
Elastography is a useful, fast and non-invasive method in the
diagnosis of breast lesions. The primary use of elastography in
the breast is as an adjunct to conventional ultrasound to
improve differentiation between benign and malignant lesions
and several studies attest to the value of EUS in refining breast
imaging reporting data system scoring. US breast to avoid unnecessary biopsies. The technique is easy to learn,
reproducibility is better than with B-mode ultrasound and fits
well into standard examination protocol. It is also useful to
confirm that a lesion is a cyst when the content is echogenic. We
proposed a practical examination protocol for strain
elastography and ARFI to avoid sonographer dependency, while
providing images, which are useful in differentiating benign from
malignant breast lesions [12].
Breast elastography is a modality that helps in the diagnosis
after the identification of changes in the mammography, it is
also used as mammographic screening in symptomatic patients
under 40 years of age and also as a complementary method to
mammography, especially in young patients or with dense
breasts. This breast study has the advantages of being a widely
available method that does not require radiation or contrast and
is well tolerated by patients. A meta-analysis carried out by Xue
et al., showed high sensitivity and specificity values for this type
of evaluation, 85% and 89%, respectively. Despite this, there is
great heterogeneity regarding the ideal cutting bridges to
differentiate between benign and malignant breast masses. In
addition, breast cancer is a heterogeneous disease, with several
differences depending on the histological type found. These
findings demonstrate the need to investigate the effectiveness
of elastography in patients with breast nodules. Taking this into
account, the objective of the present study is to evaluate the
effectiveness of elastography to differentiate the histological
types of nodules and to compare its effectiveness with the BIRADS
classification.
In a study Letman, et al., they evaluated 82,980 routine
mammograms and compared category 3 cases that progressed
to malignancy with those that were truly benign after 3 years of
radiological follow-up. Of the 1,711 cases classified as BIRADS 3,
2.1% of the total and the 82,898 routine mammograms, 150
were malignant, with a predictive value of malignancy (PPV) of
8.8%. However, after careful review of the 150 cases that were
initially classified as B3 and progressed to malignancy, only 20%
of the lesions actually met the clearly defined morphologic
criteria for this category. Graf, et al., in a study with 450 solid
nodules and morphological characteristics of category 3,
observed a PPV of only 0.2%. Early diagnosis of breast cancer has
been shown to reduce the risk of death by providing a better
chance of identifying a treatment. In general, palpation,
ultrasound and mammograms are the most common forms of
diagnosis.
However, ultrasound elastography currently plays a vital role
in the process of diagnosing breast cancer. Computer-aided
diagnosis using a combination of ultrasound (B-mode) and
elastography images show a marked superiority over other
digital imaging techniques due to their accurate classification of
lesions. Machine learning makes use of mathematical and
statistical methods and thus establishes models to learn from
the data. This method finds an important role in biomedical
applications in which the precision of these algorithms help in
the early diagnosis and measurement of pre-malignant lesions
and in making an early approach [13].
Conclusion
Physical examination of the breast by palpation can guide
towards benign and malignant pathology, since breast cancer is
harder and more fixed than the adjacent normal breast
parenchyma, unlike benign lesions that are soft and mobile.
Although breast palpation can guide, it is sometimes difficult to
reproduce and its main limitation is based on its low sensitivity
and diagnostic accuracy. Elastography is a useful, fast and noninvasive
method in the diagnosis of breast lesions. The primary
use of elastography in the breast is as an adjunct to conventional
ultrasound to improve differentiation between benign and
malignant lesions and several studies attest to the value of EUS
in refining breast imaging reporting data system scoring. US
breast to avoid unnecessary biopsies. The technique is easy to
learn, reproducibility is better than with B-mode ultrasound and
fits well into standard examination protocol. It is also useful to
confirm that a lesion is a cyst when the content is echogenic.
There are two main types of elastography, quantitative (shearwave)
and qualitative (strain). Quantitative elastography sends
micro pulses to measure tissue displacement independent of
applied acoustic pressure with minimal energy levels for
different tissues. So, it creates an organization chart of
displacement relative to adjacent structures. Qualitative
techniques indicate the existence or absence of hardness in the
area of interest. These qualitative parameters focus on showing
relative hardness between different areas, that is, they separate
the hard tissues from the soft ones and can distinguish the
presence of a lump. The information obtained is presented by
means of contrast images on a scale of colors that indicate hardness and softness. This diagnostic alternative is 100%
effective when there is no cancer, which manages to avoid
unnecessary biopsies and it is 92% effective when the cells are
malignant. In the latter three, a biopsy is recommended. In
addition, the elastography in breast cancer described in the
literature could be the assessment of the intraductal component
of the cancer because it does not present as a mass, the
assessment of the response to neoadjuvant chemotherapy and
the study of axillary lymphadenopathies for which elastography
in time real seems more sensitive than palpation and ultrasound.
References
- Bucheli DA, Espinoza MA, Vargas EF, Regalado SA, Sanchez DB, et al. (2023) Artificial intelligence in medical education: Latin American Context. Metro Ciencia 31: 21-34.
[Google Scholar]
- Ruiz Cortes S, Gonzalez Lopez A, Elzaurdin Mora RA, Rabeiro Gonzalez D, Gonzalez Lugo Y, et al. (2016) Usefulness of elastography in breast cancer regarding two cases. Cuba J Military Med 45: 372-377.
[Google Scholar]
- You Y, Song Y, Li S, Ma Z, Bo H (2019) Quantitative and qualitative evaluation of breast cancer prognosis: A sonographic elastography study. Int Med J Expclin Res 25: 9272.
[Crossref] [Google Scholar] [PubMed]
- Sadigh G, Carlos RC, Neal CH, Dwamena BA (2012) Ultrasonographic differentiation of malignant from benign breast lesions: A meta-analytic comparison of elasticity and BIRADS scoring. Breast Cancer Res Tret 133: 23-35.
[Crossref] [Google Scholar] [PubMed]
- Berg WA, Cosgrove DO, Dore CJ, Schafer FK, Svensson WE, et al. (2012) Shear-wave elastography improves the specificity of breast US: The BE1 multinational study of 939 masses. Radiol 262: 435-449.
[Crossref] [Google Scholar] [PubMed]
- Carlsen J, Ewertsen C, Sletting S, Vejborg I, Schafer FK, et al. (2015) Ultrasound elastography in breast cancer diagnosis. Ultraschall Med-Eur J Ultrasound 14: 550-565.
[Crossref] [Google Scholar] [PubMed]
- Cho N, Lim J, Moon WK (2014) Usefulness of ultrasound elastography in reducing the number of breast imaging reporting and data system category 3 lesions on ultrasonography. Ultrasonography 33: 98.
[Crossref] [Google Scholar] [PubMed]
- Lehman CD, Lee CI, Loving VA, Portillo MS, Peacock S, et al. (2012) Accuracy and value of breast ultrasound for primary imaging evaluation of symptomatic women 30-39 years of age. Am J Roentgenol 199: 1169-1177.
[Crossref] [Google Scholar] [PubMed]
- Coughlin SS (2019) Epidemiology of breast cancer in women. Adv Exp Med Biol 1152: 9-29.
[Crossref] [Google Scholar] [PubMed]
- Duncan III JL, Cederbom GJ, Champaign JL, Smetherman DH, King TA, et al. (2000) Benign diagnosis by image-guided core-needle breast biopsy. Am Surg 66: 5-10.
[Google Scholar] [PubMed]
- Graziano L, Bitencourt AG, Cohen MP, Guatelli CS, Poli MR, et al. (2017) Elastographic evaluation of indeterminate breast masses on ultrasound. Rev Bras Ginecol Obst 39: 072-079.
[Crossref] [Google Scholar] [PubMed]
- Evans A, Trimboli RM, Athanasiou A, Balleyguier C, Baltzer PA, et al. (2018) Breast ultrasound: Recommendations for information to women and referring physicians by the European society of breast imaging. Insights Imag 9: 449-461.
[Crossref] [Google Scholar] [PubMed]
- Evans A, Whelehan P, Thomson K, McLean D, Brauer K, et al. (2012) Invasive breast cancer: Relationship between shear-wave elastographic findings and histologic prognostic factors. Radiology 263: 673-677.
[Crossref] [Google Scholar] [PubMed]
Citation: Gomez JF, Munoz AFD, Dominguez HB, Galvis MCC, Medina SKS, et al. (2023) Elastography as a Method for the Detection of Breast Cancer. Health Sci J. Vol. 17 No. 9: 1085.