Kamal Niaz, Faheem Maqbool, Mohammad Abdollahi*
Department of Toxicology and Pharmacology, Faculty of Pharmacy and Pharmaceutical Sciences Research Center, Tehran University of Medical Sciences, International Campus (TUMS-IC), Tehran 1417614411, Iran
- *Corresponding Author:
- Mohammad Abdollahi
Department of Toxicology and Pharmacology
Faculty of Pharmacy and Pharmaceutical Sciences
Research Center, Tehran University of Medical Sciences
Tehran 1417614411, Iran
Tel: +98-21-66959104
E-mail: Mohammad.Abdollahi@utoronto.ca or Mohammad@tums.ac.ir
Received Date: 18.03.2016; Accepted Date: 10.04.2016; Published Date: 20.04.2016
Introduction
Over the past decade, extensive use of antibiotics in veterinary and humans contributed to bacterial resistance in the environment. The contribution of resistant bacterial strains in the environment occurred through feces, excreta of animals and humans. The enormous intake of antibiotics have resulted resistance in the normal microbiota of gastrointestinal tract (GIT) among healthy humans [1]. Furthermore, veterinarians used broad spectrum antibiotics for pets’ safety [2]. In the present editorial, we tried to document the resistance of E. coli to various antibiotics with special reference to animals and humans.
Investigative exposure to drug-resistant extraintestinal pathogenic E. coli
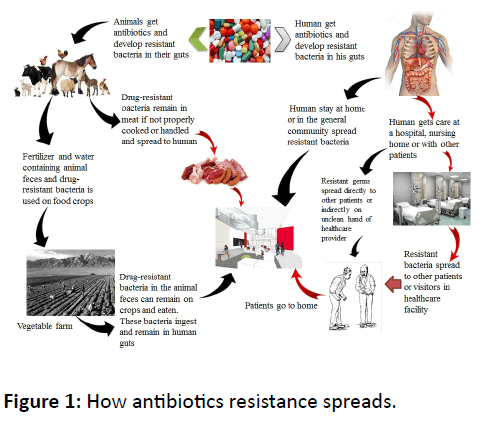
The massive practice of antibiotics in pets such as in dog lead to the existence of antibiotics resistant bacteria in feces, which have the possibility to infect public space, like parks and may contributed to public acquired infectious diseases [3]. Dogs and other domestic animals might be the important contributors in spreading of antibiotic resistance against E. coli. Furthermore, individuals returning from parks and other areas that contain canine feces unintentionally spread the resistant bacteria via shoe (Figure 1) [3]. For instance 9% of extraintestinal pathogenic E. coli multiple drug-resistant was calculated from the total quantity of E. coli identified in the shoe samples. Therefore, in order to draw attention to these sites, as potential point of exposure is important; dissemination of antibiotic resistant E. coli bacteria can put large population in urinary tract infection [4]. Canines and humans isolation of multi-drug resistant E. coli clonal groups found to be closely related, suggesting possible cross-hosts species transfer infections [5,6]. Ultimately, extensive uses of antimicrobial agents lead to resistance in animals as well as in humans. Furthermore, in animals 50% of antimicrobial and chemotherapeutic agents are given each year to increase productivity [7].
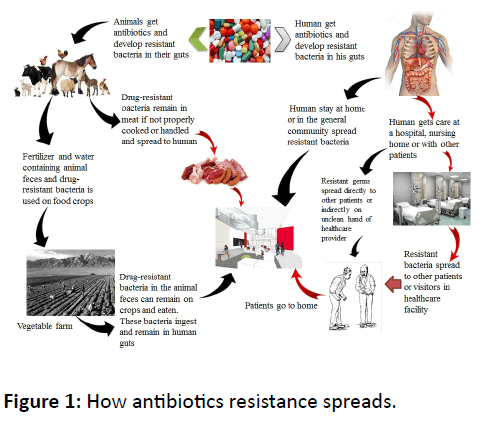
Figure 1: How antibiotics resistance spreads.
Incidence of extended-spectrum β-lactamaseproducing E. coli (ESBL-EC)
The occurrence of ESBL-EC infection has improved in community hospital. Researchers and microbiologists should draw attention to the maternity centers, community hospitals and healthcare related ESBL-EC infection [8].
Approximately, 20 hospitals in the Southeast of United State patients’ record were reviewed. By investigative analysis, it was found that admittance time, history, examinations and demographic evidence the scientists also pledge increased infections occurred due to antibiotics amongst public adherents who had inadequate contact to health maintenance facility. However, these infections developed due to other environmental risk factors such as unhygienic condition, genetics and malnutrition. In the study they have measured antibiotic-resistant pathogenesis a challenging situation in the large hospitals. This extended study confirmed that resistance to antibiotics of normal micro-flora happened in entirely health maintenance system. They also investigated that infection burden increasing in health facilities of the rural areas due to unavailability of health care units [8]. As aforementioned people living with domestic animals could possibly be at high risk to develop different species-cross infections.
Antibiotics are tremendously essential in health care settings. The statistical figures indicated that E. coli collapsed from 5.28 to 10.5 infections rate per 100,000 patients in 2009-2014 in which mostly there was drugs-resistant ESBL-EC. In these aforementioned patients average age of E. coli infected patients was 72 years [8].
It has been noticed that mostly in large health care setups, E. coli contamination chances as well spread chances are very high due to nosocomial infection. So it’s noteworthy that poor health facilities and contamination in the hospital colonized drug-resistant bacteria on the patient skin can trigger other hospital acquired infections. Health care providers and suppliers are not following standard practicing guidelines during patient’s care. So researchers should focus for E. coli and its source of resistance where it develops and struggles to vigorously monitored patients who get nosocomial infection. This pathogen is a common and predominant cause of hematological abnormalities and linked with higher morbidity and mortality among individuals especially in infants. It is notable that prevalence of disease in individual and when last hospitalized in health facility unit is very important. Individuals occasionally admitted in hospital have been found to have more chances of pathogens attack than the patients who have association with health care system or nursing homes. The information presented three time faster rise in communityassociated infection in population during 2009 and 2015 [8].
It is concluded that specialized pathogenic strains of E. coli that cause most extra-intestinal infections, represent a major but little-appreciated health threat. Although, the reasons for their evolution remain mysterious, extra-intestinal pathogenic E. coli (ExPEC) clearly possess a unique ability to cause disease outside the host in public. Broader, appreciation of the existence and importance of pathogenic E. coli and better understandings of their distinctive virulence mechanisms, reservoirs and transmission pathways may lead to effective preventive interventions. However, the other environmental risk factors like feces and food item from animal sources lead to cross-hosts species infection and multi-drug resistant E. coli found to be closely related to possible transfer and need further study.
Contributors
MA came up with the idea and KN wrote the first draft of the editorial and organized subsequent inputs. FM supported the data collection, cleaning and editing.
Competing Interests
The authors declare no competing financial interests.
9504
References
- Johnson JR, Russo TA (2002) Extraintestinal pathogenic Escherichia coli:“the other bad E coli”. J Lab Clin Med 139: 155-162.
- Al-Dabbagh M, Dobson S (2011) Infectious hazards from pets and domestic animals. AdvExp Med Biol 697: 261-272.
- Ahmed LN, Price LB, Graham JP (2015) An exploratory study of dog park visits as a risk factor for exposure to drug-resistant extra-intestinal pathogenic E. coli (ExPEC). BMC Res Notes 8: 137.
- Nordstrom L, Liu CM, Price LB (2013) Foodborne urinary tract infections: a new paradigm for antimicrobial-resistant foodborne illness. Front Microbiol 4: 29.
- Platell JL, Cobbold RN, Johnson JR, Clabots CR, Trott DJ (2012) Fluoroquinolone-resistant extraintestinal Escherichia coli clinical isolates representing the O15: K52: H1 clonal group from humans and dogs in Australia. Comp Immunol Microbiol Infect Dis 35: 319-324.
- Platell JL, Trott DJ, Johnson JR, Heisig P, Heisig A, et al. (2012) Prominence of an O75 clonal group (clonal complex 14) among non-ST131 fluoroquinolone-resistant Escherichia coli causing extraintestinal infections in humans and dogs in Australia. Antimicrol Agents Chemother 56: 3898-3904.
- Teillant A, Brower CH, Laxminarayan R (2015) Economics of Antibiotic Growth Promoters in Livestock. Annu Rev Resource Economics 7: 349-374.
- Thaden JT, Fowler VG, Sexton DJ, Anderson DJ (2016) Increasing Incidence of Extended-Spectrum ß-Lactamase-Producing Escherichia coli in Community Hospitals throughout the Southeastern United States. Infect Control HospEpidemiol 37: 49-54.