Keywords
Carotid intima-media thickness; Flowmediated vasodilation; Cardiac systolic function; Diastolic function; Nasal polyps; Rhinitis
Introduction
Many diseases characterized by chronic inflammation and by an immunological activation are associated with an increased risk of atherosclerosis.
Diseases such as lupus erythematosus, rheumatoid arthritis, chronic infections accelerate the development of atherosclerosis and allergic disorders such as allergic rhinitis or asthma can help increasing the risk.
The nature of the association observed between allergies and atherosclerosis remains speculative. Apart from the unlikely possibility that this association is due to chance, there are at least two plausible interpretations [1-4].
First, allergic disorders may constitute a real risk factor. It is well established that localized allergic diseases can cause a systemic inflammatory response mediated by the release of vasoactive peptides and cytokines in the circulation. The endothelial cells in several points from exposure to allergens site increase the expression of adhesion molecules, facilitating the trafficking of leukocytes into the vessel wall and potentially promoting atherosclerosis. Furthermore, the allergic disorders are commonly associated with respiratory infections [5], another potential vascular risk.
Second, allergic rhinitis, asthma and the atherosclerosis can share central paths and some variants of the predisposing genes. Mast cells and leukotriene’s, which are characteristic of allergy, are increasingly recognized as key factors for atherosclerosis. The functional variants of the 5-lipoxygenase and of the 5- lipoxygenase activating protein that increase the synthesis of leukotriene’s or promotes inflammation confer a high risk of atherosclerotic vascular disease in humans [6], while mice deficient of 5-lipoxygenase show excellent protection against atherosclerosis [7].
Support for this hypothesis is given by previous studies that show that the increased level of IgE [8-10] and eosinophils in the blood [11], the prick test positive results are associated with an increased risk of cardiovascular disease and death.
The Bruneck and Army studies have confirmed this hypothesis. The study ARMY, performed in Innsbruck in 2001, has recruited adults with allergic disease; intima media thickness (IMT) was measured resulted higher than controls. The Bruneck study is a prospective study carried out in Brunico on a sample of 1000 subjects. In these patients it studied the progression of carotid disease from 1990 to 1995 and confirmed the progression of plaque formation [12].
In inflammatory diseases of the airways, inflammation can also be seen at the systemic level, thus determining extra nasal clinical manifestations, including muscle weakness, diseases of the cardiovascular system, high blood pressure [13], depression, worsening cognitive function, sleep disorders.
Pi-Chieh et al. [1] in an epidemiological study showed that patients with rhino sinusitis have a higher risk of acute myocardial infarction.
Rhinitis also involves intracranial vessels and can lead to increased frequency of stroke. Ferrari et al. [3] instead have shown that patients with rhinitis, regardless of the presence of atopy, have a higher risk of suffering from intermittent claudication [2].
Despite being very different disease entities, rhinitis, nasal polyposis and vascular dysfunction, they have some common elements. In both cases the primary pathogenic noxious factor that triggers the degenerative process is inflammation.
Aim
The aim of the study is to verify if the rhinitis and nasal polyposis can induce early cardiovascular structural abnormalities and endothelial dysfunction.
Materials and Methods
For the present study a sample of 44 adults was enrolled, aged between 18 and 60 years, of both sexes, belonging to the Otolaryngology Unit of Policlinico of Bari for rhinitis or nasal polyposis, and 42 subjects in the control group.
We divided patients into 5 groups, depending on the type of rhinological diagnosis:
• Group 1, patients with allergic rhinitis
• Group 2, patients with nasal polyposis
• Group 3, patients with overlap (allergic rhinitis and nonallergic rhinitis, as NARES, NARESMA, etc.)
• Group 4, patients with not allergic rhinitis
• Group 5, patients suffering from polyposis in the context of an allergic rhinitis.
These classifications were made on the basis of the 2014 ARIA guidelines. The distribution of patients according to the rhinological diagnosis was the following:
• Group 1, 13 patients (30%) with allergic rhinitis
• Group 2, 4 patients (9%) patients with polyposis
• Group 3, 6 patients (14%) patients with overlap of allergic rhinitis and not allergic rhinitis
• Group 4, 5 patients (11%) suffering from non-allergic rhinitis
• Group 5, 16 patients (36%) patients with polyposis and allergic rhinitis.
During enrollment consent and assent to the study was obtained; demographic data were collected and the following program was made:
• Family and medical history
• Nasal cytology
• Prick test
• Nasal endoscopy
During the second visit, vascular ultrasound and Echocardiography assessment was carried out:
• Intima-media thickness (IMT) of the right and left common carotid arteries
• Flow-mediated dilation (FMD)
• Echocardiogram
• Left and right diastolic and systolic ventricular function
Vascular Ultrasound Studies
All patients underwent high definition vascular and cardiac echography according to the following protocols to identify early atherosclerotic changes.
FMD of Brachial Artery
The ultrasound technique is called FMD (flow mediated dilation, dilation induced by the flow) and measures the degree of brachial artery dilation [14] (but can be also used the radial artery) in response to an increase of the "shear stress". We must consider that the endothelial function of the brachial artery is closely related to that one found at the same time in the coronary artery [15].
In peripheral arteries, a temporary increase in shear stress can be induced by increasing the flow of blood, the so-called "reactive hyperemia." Reactive hyperemia can be obtained by inflating a sleeve around the forearm for a few minutes and then by deflating it. This causes an abrupt decrease in vascular resistance. After deflation, the postiperemia arterial diameter increases.
The method involves the use of Philips Sonos 5500 with linear probe from 7.5 MHz to 10 MHz. After a rest period of about 10 minutes with ECG monitoring in an air conditioned room, the brachial artery of the right arm is studied in different longitudinal scans with the probe placed over the elbow crease. Subsequently, obtained an optimal longitudinal scan, the diameter of the vessel must be measured on ECG R-wave four times to calculate the average value. Once that has been measured the average diameter of the brachial artery at rest, a sleeve sphygmomanometer is positioned 3 cm to 5 cm below the bend of the elbow, than it is inflated to a pressure of 50 mmHg higher than the systolic blood pressure for 5 min [16]. Afterwards the sleeve is deflated, which involves the phenomenon of reactive hyperemia.
Brachial artery diameter is measured several times, every 20 s to about three minutes, taking into account that the maximum expansion is obtained on average between 60 s and 90 s.
The flow-mediated dilatation (FMD) is calculated as the percentage difference between the maximum post-ischemic diameter reached and the average basal diameter [14].
Values of FMD higher than 7% are considered normal [17].
The FMD is not an invasive method and it allows the recognition of a population of subjects with impaired endothelial function [18], but it presents a certain variability intra and inter-operator [19].
Ultrasound Measurement of CIMT
Using the same ultrasound scanner and the same probe used for the brachial artery, doppler of left and right common carotid arteries were performed.
With the patient supine and the head rotated 45 degrees to the examiner, the physician positions the probe perpendicular to the carotid artery.
To assess the carotid stiffness, the operator should use the Bmode and insert the cursor M-mode along the common carotid artery one centimeter proximal to the bulb. IMT is defined as a low-level echo gray band that does not project into the arterial lumen and it is measured during end-diastole. It calculates the average of three maximum values of IMT.
In adults, increased intima media thickness is in direct correlation with cardiovascular risk factors [20-22] and the degree of severity is associated to coronary artery disease [23]; IMT is considered as a predictor of cardiovascular events [24-28].
Echocardiographic Evaluation of Systolic and Diastolic Ventricular Function
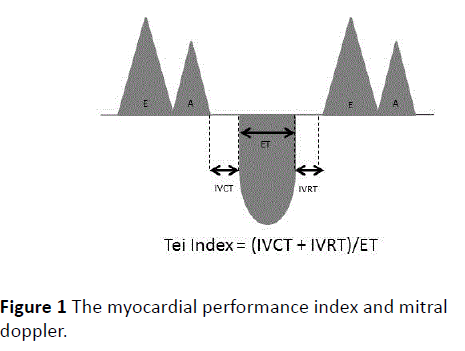
To evaluate the right and left systolic and diastolic ventricular function was performed an echocardiogram to each patient (Figure 1). Fraction of shortening, the Doppler study of transmittal flow, the tissue doppler have been examined and the Tei index was calculated. The myocardial performance index (Tei or index) is calculated as the sum of the duration of isovolumic relaxation (IVRT) and the duration of the contraction (IVCT), divided by the systolic ejection period ET. It has been proposed as a measure of global function, systolic and diastolic, and it can be applied to both ventricles. The normal left myocardial performance index is about 0.4; typically higher values of 0.6 to >1.0 may indicate a systolic ventricular dysfunction (with a prolonged isovolumic contraction) or diastolic (with prolonged isovolumic relaxation), or both of them. The value is normal when <0.55 in the right ventricle. The index increases if it increases the duration of the contraction and isovolumic relaxation which are respectively the expression of left ventricular diastolic and systolic dysfunction.
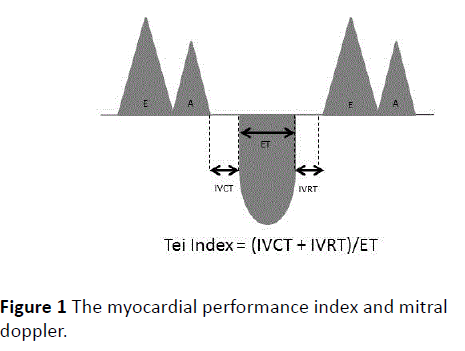
Figure 1: The myocardial performance index and mitral doppler.
Although the myocardial performance index is not influenced by abnormal ventricular geometry or changes in heart rate, it can be changed instead to preload and afterload changes. The index can be calculated using intervals of time measured by Doppler tissue [29].
Statistical Analysis
Data were analyzed with Statsoft software. The continuous variables were expressed as mean and standard deviation. For the considered data these tests were used: t-student for independent samples (or unpaired/independent test) and chi square test.
A p<0.05 was considered statistically significant.
Results
Out of 44 patients, 35 had an allergic component. The first significant data regarded the assessment of flow-mediated dilatation in patients suffering from rhinitis and in the control group. In particular average values were significantly lower in patients with rhinitis (Table 1).
| |
Rhinitis |
Control |
p |
| |
N=35 |
N=42 |
|
| FMD % |
6.92 |
17.47 |
0.000 |
| IMT DX(mm) |
0.68 |
0.61 |
0.0429 |
| IMT SX (mm) |
0.65 |
0.59 |
0.0498 |
| E/A mitral |
1.34 |
1.63 |
0.0004 |
| E'/A' mitral |
1.48 |
2.37 |
0.0004 |
| E/E' |
18.57 |
6.08 |
0.0032 |
| IVRT mitral |
92.28 |
79.42 |
0.008 |
| E/A tricuspid |
2.05 |
1.48 |
0.0165 |
| TeiIndex tricuspid |
1.28 |
0.44 |
0.0002 |
| TAM |
20.74 |
22.5 |
0.0489 |
| S tricuspid (cm/s) |
21.16 |
14.85 |
0.0139 |
Table 1 Endothelial function and echocardiographic parameters of the patients studied expressed as mean, with associated statistical significance; the p<0.05 were related to statistically significant values.
Intima-media thickness was normal in both groups, although patients with rhinitis had higher values than control group with statistical significance.
The Tei index tricuspid appeared significantly higher in patients with rhinitis than in the control group.
The comparison was made between the patients with polyposis and the patients of the control group. The FMD of the group of patients suffering from the disease was significantly lower than control patients (Table 2). Furthermore patients without polyposis (Group A, including 1-3-4 Group according to ARIA Classification) were compared with patients with polyposis and allergic rhinitis with polyposis (Group B, including Group 2-5 of the ARIA classification) (Table 3). The IMT appeared normal in all subjects tested but there was a significant difference comparing the two diseases together: patients with polyps tended to have higher IMT than patients in Group A. The Tei index was higher than normal in both groups, but the patients in Group B had higher values of right dysfunction compared with Group A.
| |
Polyposis |
Control |
p |
| |
n=20 |
n=42 |
|
| FMD % |
6.98 |
19.41 |
0.0017 |
| E/E' mitral |
26.37 |
8.29 |
0.0025 |
| E/E' tricuspid |
184.17 |
18.15 |
0.0165 |
| S tricuspid (cm/s) |
24.65 |
14.85 |
0.0019 |
Table 2 Echocardiographic parameters of endothelial function of patients with nasal polyposis and in control group, with associated statistical significance; the p <0.05 is related to statistically significant values.
| |
GROUP A |
GROUP B |
P |
| |
N=24 |
N=20 |
|
| IMT sx |
0.62 |
0.73 |
0,0224 |
| EA' mitral |
9.92 |
26.37 |
22 |
| IVRT mitral |
78.5 |
102.5 |
0 |
| EVA' tricuspid |
1.35 |
0.74 |
27 |
| E/E' tricuspid |
49.85 |
184.17 |
0,0443 |
| Tei Index Tricuspid |
0.74 |
1.68 |
15 |
Table 3 Echocardiographic parameters of endothelial function of patients without polyps and parameters of patients with nasal polyposis, with associated statistical significance; the p<0.05 were related to statistically significant values.
Discussion
Rheumatoid arthritis, systemic lupus erythematosus, seronegative spondyloarthropathies, psoriasis and inflammatory bowel disease are diseases already studied in their association with cardiovascular risk.
The idea of looking for a relationship between nasal disease and endothelial dysfunction has already been considered in a recent study by Elcioglu et al. [30]. Indeed, they have investigated the relationship between chronic rhino sinusitis, carotid intima-media thickness, flow-mediated dilation (FMD) of the brachial artery and micro albuminuria.
In this study, 38 patients with chronic rhino sinusitis were compared with 29 patients in a control group. Patients with chronic rhino sinusitis had lower scores of FMD (p=0.031), higher values of IMT (p=0.005) and a higher ratio Albumin-urine creatinine (p=0.036) compared with healthy controls.
The links between inflammatory diseases and cardiovascular disease have not been fully elucidated. It seems likely that chronic inflammation, a common feature of these diseases, is involved in the pathogenesis of accelerated endothelial dysfunction. There are several potential mechanisms.
It is well known that TNF-α plays a critical role in inflammation. The vascular endothelium is a target of TNF-α. At the cellular level, TNF-α induces the expression of genes associated with inflammation, coagulation, and the proliferation and reduces the expression of the protein e-NOS and [31]. In addition, TNF-α induces the CAM expression on the surface of vascular endothelial cells in contrast to NO, also known to be an inhibitor of CAM expression [32].
The inflammatory cytokines and TNF spread from specific primary site of pathology in the circulation, spreading a systemic inflammatory response.
The products of inflammation such as ROS, dyslipidemias feed endothelial dysfunction, increasing the expression of adhesion molecules (VCAM, ICAM), the diapedesis of leukocytes, and the production of ROS and reduced response NO dependent vasodilation and relaxation of the smooth muscle [33].
These mechanisms therefore explain the reason for which FMD was lower both in patients considered in our study and in patients suffering from systemic inflammatory diseases already studied previously.
Endothelial dysfunction could lead to subclinical organ damage as the increase in carotid IMT. In patients in our study, with a mean age of 39.64 years, IMT appeared normal, but significantly higher than the control group. This could mean that with increasing age, with the onset of additional risk factors, such as hypertension, smoking, diabetes these individuals are at risk of developing a vascular disease at an earlier age than the normal population. Patients seen in our study, in fact, have been carefully selected, eliminating all those who had any cardiovascular risk factor.
The correlation with right ventricular systolic and diastolic dysfunction is instead less studied and investigated. Studies have shown a higher incidence of cardiovascular events such as stroke, intermittent claudication and acute myocardial infarction [14,15] in patients with polyposis and/or rhinitis, but meager are the studies that have focused attention on myocardial damage.
Nasal polyposis and rhinitis are chronic diseases that can lead to chronic hypoxia and hypercapnia. The latter can cause arterial vasoconstriction and in severe cases pulmonary hypertension.
If left untreated, this condition can lead to overload, hypertrophy and dilatation of the right ventricle, due to an increase in pulmonary resistance and pulmonary artery pressure, which over time can lead to a condition of right ventricular failure and death [34].
Therefore, early recognition of the right dysfunction can prevent cardiopulmonary complications.
The TDI is a technique, based on the demonstration of the movement of the myocardial tissue with the low frequency and high amplitude filtering the movements of blood components with high frequency [35].
Studies have confirmed that the TDI technique is very practical and it has a potential value in assessing the diastolic and systolic function of the right ventricle [36], even with its limitations.
In our study, in fact, the TDI at the level of the right ventricular showed that the speed of E', A', S, and the ratio E'/A' were similar to the control group. The increased tricuspid Tei index is an extremely interesting correlation emerged in the group studied both in patients with nasal polyps and in patients with rhinitis, even if with lesser extent. The Tei index is an extremely complex as sensitive index of myocardial performance, which attests to the presence of ventricular dysfunction. This parameter is advantageous and it can express an initial cardiac dysfunction.
In the present study the TDI showed no further correlations with other parameters of subclinical diastolic and systolic right ventricular dysfunction.
The speed S of the tricuspid that helps to assess the right ventricular systolic function was in fact in the standard and same thing applies to the TAPSE. It would be interesting investigating subclinical dysfunction with the strain (S technology) and strain rate (SR). In 2013 a study [4] was performed, in which echocardiography S and SR showed a subclinical deficiency of the longitudinal right functions in patients with nasal polyposis, where a simple echocardiogram showed no alterations of the right sections [4].
We think that due to hypoxia, hypoventilation and hypercapnia, right ventricular function in patients with nasal disorders, particularly nasal polyposis, can be compromised in the myocardial tissue level.
The results of our study suggest that patients suffering from nasal polyps and rhinitis, that are clinically asymptomatic and have a normal right ventricular function in conventional echocardiography, have a subclinical dysfunction, demonstrated by the significantly higher value of tricuspid Tei index. The same result was obtained in a previous study performed at the clinic of Cardiology of Bari in asthmatic children.
Other studies should be performed to demonstrate that the tricuspid Tei index is a decisive parameter of RV function and that would indicate a subclinical dysfunction.
The data suggest the importance of performing in subjects with rhinitis and nasal polyposis not only an endoscopic and cytological monitoring, but also of atherosclerotic risk and cardiac contractile function.
The study still has limitations related to the small number of patients enrolled and the critical issues will be resolved by expanding the number of the sample. However in the sample considered it has already been possible to demonstrate endothelial dysfunction and premature right ventricular echocardiographic alteration.
Conclusions
There is strong evidence that the mechanisms responsible for accelerated atherosclerosis in patients with inflammatory diseases of the nasal cavity are related to the high degree of local inflammation which then becomes systemic inflammation. This leads to endothelial dysfunction through multiple mechanisms and still under study and results in a subclinical endothelial damage, as evidenced from increasing values of IMT in patients with rhinitis and polyposis, although they are normal values, and by the lower values of FMD. Endothelial dysfunction with predominance of vasoconstriction, proliferation, and remodeling of the vascular wall can lead to a progressive increase in pulmonary pressure, which leads to right ventricular overload, even in the early subclinical disease states. This overload is expressed by a higher value of tricuspid Tei index to TDI.
17924
References
- Pi-Chieh W, Herng-Ching L, Jiunn-Horng K (2013) Chronic rhinosinusitis confers an increased risk of acute myocardial infarction. Am J Rhinol Allergy 27: e178-e182.
- Jiunn-Horng K, Chuan-Song W, Keller JJ, Herng-Ching L (2013) Chronic rhinosinusitis increased the risk of stroke: A 5-year follow-up study. Laryngoscope 123: 835-840.
- Ferrari M, Pesce G, Marcon A, Vallerio P, Pasini F, et al. (2014) Rhinitis is associated with a greater risk of intermittent claudication in adults. Allergy 69: 472-478.
- Simsek E, Simsek Z, Tas MH, Kucur C, Gunay E, et al. (2013) Evaluation of right ventricular functions in patients with nasal polyposis: an observational study.
- Egger KS, Mayr MG (2001) Chronic infections and the risk of carotid atherosclerosis: prospective results from a large population study.
- Dwyer JH, Allayee H, Dwyer KM, Fan J, Wu H, et al. (2004) Arachidonate 5-lipoxygenase promoter genotype, dietary arachidonic acid, and atherosclerosis.N Engl J Med 350: 29-37.
- Mehrabian M, Allayee H, Wong J, Shi W, Wang XP, et al. (2002) Identification of 5-lipoxygenase as a major gene contributing to atherosclerosis susceptibility in mice.Circ Res 91: 120-126.
- Criqui MH, Lee ER, Hamburger RN, Klauber MR, Coughlin SS (1987) IgE and cardiovascular disease. Results from a population-based study.Am J Med 82: 964-968.
- Langer RD, Criqui MH, Feigelson HS, McCann TJ, Hamburger RN (1996) IgE predicts future nonfatal myocardial infarction in men.J ClinEpidemiol 49: 203-209.
- Korkmaz ME, Oto A, Saraçlar Y, Oram E, Oram A, et al. (1991) Levels of IgE in the serum of patients with coronary arterial disease.Int J Cardiol 31: 199-204.
- Hospers JJ, Schouten RB, Postma JP, Weiss ST (1999) Eosinophilia and positive skin tests predict cardiovascular mortality in a general population sample followed for 30 years. Am J Epidemiol 150: 482- 49
- Knoflach M, Kiechl S, Mayr A, Willeit J, Poewe W, et al. (2005) Allergic rhinitis, asthma, and atherosclerosis in the Bruneck and ARMY studies.Arch Intern Med 165: 2521-2526.
- Heinrich J, Döring A (2004) Blood pressure and rhinitis in adults: results of the MONICA/KORA-study.J Hypertens 22: 889-892.
- Corretti MC, Anderson TJ, Benjamin EJ (2002) Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am CollCardol 39: 257-265.
- Verma S, Buchanan MR, Anderson TJ (2003) Endothelial function testing as a biomarker of vascular disease.Circulation 108: 2054-2059.
- Pyke KE, Tschakovsky ME (2005) The relationship between shear stress and flow-mediated dilatation: implications for the assessment of endothelial function. J Physiol 568: 357-369.
- Moens AL, Goovaerts I, Claeys MJ, Vrints CJ (2005) Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool?Chest 127: 2254-2263.
- Sonka M, Liang W, Lauer RM (2002) Automated analysis of brachial ultrasound image sequences: early detection of cardiovascular disease via surrogates of endothelial function. IEEE Trans Med Imaging 21: 1271- 1279.
- González AS, Kostine A, Gómez-Flores JR, Márquez MF, Hermosillo AG, et al. (2006) Non-invasive assessment of endothelial function. Intra and inter-observer variability.Arch CardiolMex 76: 397-400.
- Poli A, Tremoli E, Colombo A, Sirtori M, Pignoli P, et al. (1988) Ultrasonographic measurement of the common carotid artery wall thickness in hypercholesterolemic patients: a new model for the quantitation and follow-up of preclinical atherosclerosis in living human subjects. Atherosclerosis 70: 253-261.
- Haapanen A, Koskenvuo M, Kaprio J, Kesäniemi YA, Heikkilä K (1989) Carotid arteriosclerosis in identical twins discordant for cigarette smoking.Circulation 80: 10-16.
- Ciccone M, Vettor R, De Pergola G, Pannacciulli N (2001) Plasma leptin is independently associated with the intima-media thickness of the common carotid artery. Int J ObesRelatMetabDisord 25: 805-810.
- Burke GL, Evans GW, Riley WA, Sharrett AR, Howard G, et al. (1995) Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) Study.Stroke 26: 386-391.
- Salonen JT, Salonen R (1991) Ultrasonographically assessed carotid morphology and the risk of coronary heart disease.ArteriosclerThromb 11: 1245-1249.
- Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M (2007) Prediction of clinical cardiovascular events with carotid intima-media Thickness: a systematic revew and meta-analysis. Circulation 115: 459-467.
- Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, et al. (1997) Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993.Am J Epidemiol 146: 483-494.
- Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE (1997) Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study.Circulation 96: 1432-1437.
- O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, et al. (1999) Cardiovascular Health Study Collaborative Research Group. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med 340: 14-22.
- Mishra RK, Kizer JR, Palmieri V, Roman MJ, Galloway JM, et al. (2007) Utility of the myocardial performance index in a population with high prevalences of obesity, diabetes, and hypertension: the strong heart study. Echocardiography 24: 340-347.
- Elcioglu OC, Afsar B, Bakan A, Takir M, OzkokAet al. (2016) Chronic rhinosinusitis, endothelial dysfunction, and atherosclerosis. Am J Rhinol Allergy30: 58-61.
- Neumann P, Gertzberg N, Johnson A (2004) TNF-alpha induces a decrease in eNOS promoter activity. Am. J. Physiol. Lung Cell. Mol. Physiol 286: L452-L459.
- Bergh N, Ulfhammer E, Glise K, Jern S, Karlsson L (2009) Influence of TNF-alpha and biomechanical stress on endothelial anti- and prothrombotic genes.BiochemBiophys Res Commun 385: 314-318.
- Curtis M, Miller FJ Jr (2014) Endothelial Dysfunction in Chronic Inflammatory Diseases. Int J MolSci 25: 11324-11349.
- Naiboglu B, Deveci S, Duman D, Kaya KS, Toros S, et al. (2008) Effect of upper airway obstruction on pulmonary arterial pressure in children. Int J PediatrOtorhinolaryngol 72: 1425-1429.
- Nikitin NP, Witte KK (2004) Application of tissue Doppler imaging in cardiology.Cardiology 101: 170-184.
- Moustapha A, Lim M, Saikia S, Kaushik V, Kang SH, et al. (2001) Interrogation of the tricuspid annulus by Doppler tissue imaging in patients with chronic pulmonary hypertension: implications for the assessment of right ventricular systolic and diastolic function. Cardiol 95: 101-104.