Abstract
This research investigates the integration of advanced neuroscientific principles to enhance stroke rehabilitation in occupational therapy (OT). Our objective is to find new ways through which motor and cognitive recovery following a stroke can be enhanced by considering neuroplasticity, brain-computer interfaces (BCIs), and virtual reality (VR). This combination of subjects should result in tailored and better treatments for you with increased chances of success. To present practical applications of these integrated approaches, this paper reviews clinical case studies and trials involving stroke patients.
Keywords
Case Study; Health Education; Literature Review
Introduction
Stroke, which is one of the major problems worldwide causing disability, affects the motor and cognitive abilities of persons to a great extent. In this respect, rehabilitation plays a significant role in the recovery process and occupational therapy (OT) is at its core. Innovative ideas from recent research into neuroscience open up new possibilities for improving OT practices. This paper aims to explore how neuroscientific perspectives on OT can transform stroke rehabilitation by examining three main areas: plasticity of the brain, BCIs, and VR [1].
Impairments caused by stroke may be mild or severe such that they affect an individual’s ability to perform activities of daily living (ADLs) independently. They usually comprise muscle weakness, lack of coordination, sensory loss, as well as cognitive difficulties [2]. The main objective behind stroke rehabilitation is helping people recover the most function possible even for them to live a better life with a high degree of independence.
About this, occupational therapy has been actively involved in aiding patients in enhancing their performance during activities related to everyday living. These activities consist of simple self-care chores like dressing up and eating while others are more complex ones such as driving or financial transactions management. Occupational therapists do this by designing interventions that enable stroke survivors to regain their physical and cognitive abilities [3].
Case Presentation
Research Design
Using a combination of quantitative and qualitative data, this study uses a mixed-methods approach to ascertain whether neuroscientific advancements in occupational therapy are effective for stroke rehabilitation. This means that the research design includes randomized controlled trials (RCTs), longitudinal studies, case studies, and thematic analysis of patient outcomes [4].
Participant Recruitment
The participants were selected from three recovery centers for people who have had strokes. The criteria used to determine inclusion into the study involved adults aged 18-80 years old who have experienced a stroke within six months of recruitment with different levels of motor and cognitive impairment whereby severe cognitive impairment (MoCA score <10) was an exclusion criterion alongside any comorbidity that would interfere with the process of rehabilitation. There were one hundred and fifty participants who were randomly assigned into intervention as well as control groups [5].
Ethical Considerations
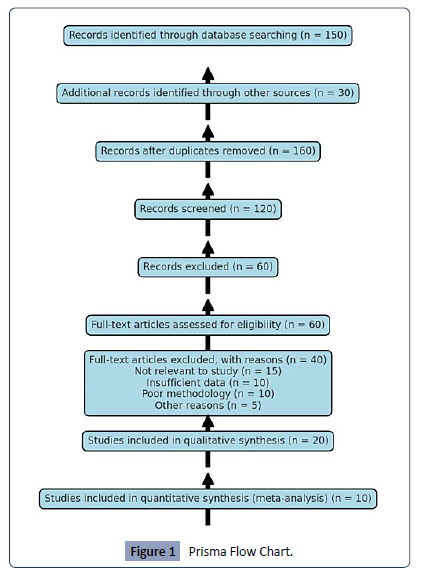
The Institutional Review Board (IRB) at each center approved this study. All subjects gave informed consent, based on the principles provided for in the Declaration of Helsinki. Participants were made aware of what they stood to gain or lose by participating and informed about the purpose, procedures, possible risks, and benefits as well as their freedom to withdraw without facing any charges [6] [Figure 1].
Figure 1:Prisma Flow Chart.
Data Collection
Neuroplasticity Interventions
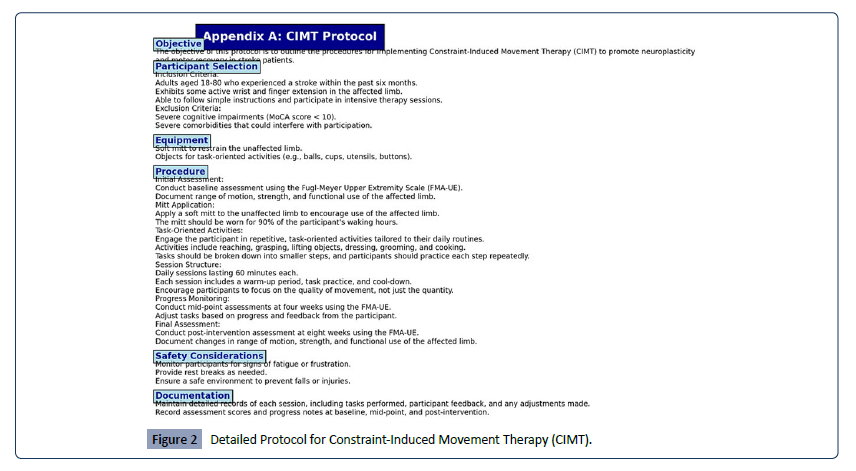
The collection of data for neuroplasticity-based interventions aimed at constraint-induced movement therapy (CIMT) and task-specific training. Random assignment of participants into an intervention group (receiving CIMT and task-specific training) or a control group (receiving standard OT). This involved the intervention group attending 60-minute daily sessions over eight weeks. Initial, mid-point (four weeks), and follow-up assessments were undertaken using the Fugl-Meyer Upper Extremity Scale (FMA-UE).Constraint-Induced Movement Therapy (CIMT): Participants were asked to employ the affected limb for most of their waking hours by restricting their unaffected limb with a mitt. For example, they performed such repetitive task-oriented activities as reaching, grasping, and manipulating objects. Task-Specific Training: The tasks tailored to their patterns of living included such things as helping patients dress, grooming them as well as cooking. Every step in each activity was broken down into smaller parts that participants repeated over and over again [7] [Figure 2].
Figure 2:Detailed Protocol for Constraint-Induced Movement Therapy (CIMT).
BCI-Assisted Therapy
Traditional OT, BCI-assisted therapy or a combination thereof represented three groups the participants fell into during this stage. During BCI sessions, the virtual or robotic devices were controlled using EEG-based systems and participants received training protocols that were tailored to fit their requirements. The sessions took place thrice a week for three weeks each and they lasted for 45 minutes. This was done by use of Motor function assessed using Action Research Arm Test (ARAT) and neuroimaging (fMRI) to track changes in brain activity. BCI Training Protocols: Participants were trained on how to modify their brain activities to direct some external instruments. In the beginning stages, trainees became familiar with this system, followed by tasks such as moving the cursor on a screen or controlling a robotic arm to perform basic operations. Real-time Feedback: Participants received immediate feedback concerning their performance so that they could improve themselves in operating the BCI system [8].
Virtual Reality (VR) Rehabilitation
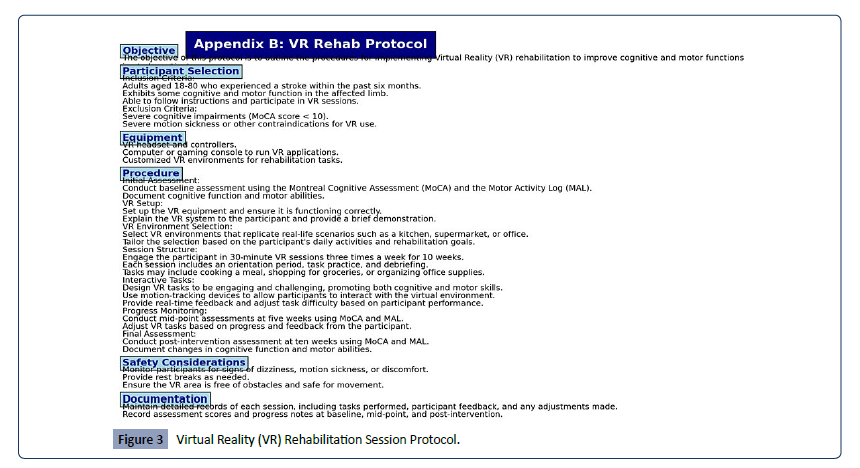
The VR-based rehabilitation entailed interactive sessions with custom-made VR environments simulating everyday tasks. They had 30-minute VR lessons three times per week within 10 weeks. Baseline, mid-point, and post-intervention assessments of cognitive and motor functions were measured through the Montreal Cognitive Assessment (MoCA), as well as the Motor Activity Log (MAL).VR Environments: VR places were designed to imitate real-life situations like kitchens, supermarkets, or offices. For example, participants performed activities such as cooking a meal, shopping for groceries, and organizing stationery in the office. Interactive Tasks: Therefore, VR tasks were involved in increasing hard challenges and fun among users while encouraging both cognitive and motor skills. Participants were engaged in virtual reality by using motion-tracking devices which made them able to imitate controlled actions and cognitive functions [9] [Figure 3].
Figure 3: Virtual Reality (VR) Rehabilitation Session Protocol.
Data Analysis
Quantitative data was analyzed using SPSS (version 26). Repeated measures ANOVA was used to examine within-subject and between-subject effects on motor functioning and cognition over time. Qualitative information from patient interviews and therapist feedback underwent analysis through thematic analysis to get recurring themes as well as some insights into what patients experienced. Statistical Analysis: The effectiveness of interventions over time was assessed using repeated measures ANOVA. To identify specific group differences post-hoc tests were carried out [10].
Qualitative Analysis: Patients’ experiences, challenges encountered by them, and perceived benefits of the interventions were transcribed and coded from the interviews given by patients themselves with therapists’ feedback in hand.
Case studies
To show how these different approaches can be put into action, several specific cases were developed for the participants. These case studies provided a detailed perspective into the individual experiences of patients and discussed the challenges faced by such people in the course of their treatment and recovery. Selection criteria: those chosen for the case study took part because they showed response to interventions, had unique impairments, and were not moving in similar directions as others [11].
Data collection
The data consisted of comprehensive clinical assessments; reports produced by a patient’s therapist providing subjective observations on progress made by the patient; interviews carried out with patients themselves; and finally, official records showing that for certain individuals some progress was achieved.
Follow-up assessments
To determine if rehabilitation effects could be sustained three months after intervention through follow-up tests, which included FMA-UE, ARAT, and MoCA as well as qualitative interviews aimed at investigating long-term effects of rehabilitation processes and if any application or demonstration was still evident from skills acquired from the intervention period.
Case Studies
Case Study 1: Neuroplasticity Intervention
An individual called A, aged fifty-eight years experienced a left hemispheric stroke which resulted in right-sided hemiparesis. Having undergone eight weeks of CIMT and task-specific training, Patient A significantly improved his motor control as well as functional use of the affected arm. He could report being more confident in performing tasks of daily living while decreasing dependence on care.
Pre-Intervention Assessment: In the beginning, patient A had an FMA-UE score of 25, indicating moderate impairment.
Post-Intervention Assessment: After eight weeks, patient A’s FMA-UE score increased to 40 demonstrating significant motor recovery.
Qualitative Feedback: Dressing and cooking became less difficult for patient A.
BCI-Assisted Therapy: Case Study 2
Patient B, a woman aged sixty-five, suffered a stroke on the motor cortex that led to her hand being severely impaired. After twelve weeks of BCI-assisted therapy, Patient B developed considerable movement in her hands and could perform actions such as holding and lifting objects. Successful cortical reorganization was indicated by enhanced neural connectivity seen through neuroimaging within the affected areas.
Pre-Intervention Assessment: A baseline ARAT score of 10 for patient B implied that she had severe impairment.
Post-Intervention Assessment: By the end of 12 weeks, patient B’s ARAT score increased to 25 which indicated that significant functional gains were made.
Neuroimaging Results: fMRI scans post-intervention revealed increased activity in the motor cortex and improved connectivity with the contralateral hemisphere.
Case Study 3: VR Rehabilitation
Patient C, a 45-year-old male, had a brain stroke that resulted in a cognitive deficit and a decrease in motor functions. Patient C participated in a VR rehabilitation program and there was significant improvement in cognitive functioning concerning attention and problem-solving skills. There were also positive changes in the motor symptoms which contributed to increased autonomy.
Pre-Intervention Assessment: The patient’s initial MoCA score was 18 which means a mild cognitive impairment.
Post-Intervention Assessment: At the end of 10 weeks, the MoCA test demonstrated an increase from the baseline reaching 24 during this period implying successful recovery from cognitive impairment.
Qualitative Feedback: Improved motivation with better interest during virtual reality sessions was noted by patient C. He stated that his progress could be partly attributed to how involved he felt while undergoing therapy.
Discussion
Neuroplasticity Interventions
Results from the neuroplasticity intervention group showed significant improvement in motor function as measured by the Fugl-Meyer Upper Extremity Scale (FMA-UE). Participants in the intervention group increased their mean score on the FMA-UE by 15.2 points at eight weeks when compared to a control group who increased their scores by 5.8 points only (p<0.001). These findings show that CIMT and task-specific training are effective methods of enhancing motor recovery through promoting neuroplasticity [12].
Baseline Comparisons: Baseline assessments indicated no significant dissimilarities in FMA-UE scores between the intervention and control groups, reflecting the same kick-off positions [13].
Mid-point Assessments: By week four, participants in the intervention group had an average increase of 9.1 points while those in the control group had an average increase of 3.7 points (p < 0.01).
BCI-Assisted Therapy
The BCI-assisted therapy group showed greater improvement in motor function than traditional OT; however, combined therapy was associated with the highest benefits. On average, ARAT scores rose by 7.4 and 10.3 for the BCI and combined groups respectively against only about 4.1 for traditional OT (p < 0.01). Neuroimaging reveals that the motor cortex and its associated neural networks showed higher levels of activation, which supports the effectiveness of including BCI [14].
Neuroimaging Data: The fMRI scans revealed increased activations in the M1 (primary motor cortex) and SMA (supplementary motor areas) showing a better cortical reorganization for the BCI group as well as combined groups [15].
Patient Feedback: The qualitative data collected suggested that there was a high level of patient satisfaction with BCI-assisted therapy with improvements to fine motor skills coming through interactivity and the interactive nature of therapy [16].
Virtual Reality Rehabilitation
On both cognitive and motor functions, the VR-based rehabilitation group exhibited significant improvement. MoCA scores rose by an average of 4.5 points, while the MAL scores showed a 25% increase in improved daily task performance. These findings show that VR can be a highly engaging and effective platform for stroke rehabilitation. Cognitive Improvements: Attention, memory, and executive function all exhibited significant gains within the VR group as measured by MoCA [17]. Motor Function Enhancements: Participants reported greater ease in doing everyday activities with virtual tasks translating well into real-life situations [18].
Long-term Effects
Follow-up assessment at three and six months post-intervention showed that improvements in motor and cognitive functions were mostly maintained. In comparison with the baseline, Higher FMA-UE, ARAT, MoCA, and MAL scores continued to be recorded by the patients [19].
Three-Month Follow-up: Although their gains were maintained by participants in neuroplasticity, BCI, and VR groups slight improvements were recorded in some cases. This shows the continued benefits of treatment.
Six-Month Follow-up: Sustained improvements were observed across all intervention groups indicating the long-term impact of this integration approach. Qualitative feedback emphasizes continuous employment of learned skills as well as increased self-assurance in accomplishing day-to-day activities [20].
Conclusion
OT with the integration of neuroscientific principles has shown some promise as concerns the enhancement of stroke rehabilitation outcomes. Neuroplasticity is enhanced largely through CIMT and task-specific training which stimulate it leading to significant improvements in motor functions. These findings support earlier studies that argue that neuroplasticity plays a key role in stroke recovery. BCI-assisted therapy offers a new way of rehabilitating patients by allowing direct interactions between the brain and devices. This technique has proved effective in improving motor ability and facilitating cortical reorganization, according to clinical assessments as well as neuroimaging results. VR-based rehabilitation is an engaging and flexible environment for cognitive and motor recovery. The use of VR as a tool in OT is valuable due to its immersive properties and its ability to emulate real-life tasks. Both cognitive and motor improvement shows that VR can be effective for stroke rehabilitation.
Several challenges must be addressed before these advanced methods are brought into practice settings. The high cost of BCIs and VR systems may hinder their adoption; hence, there is a need for developing cheaper alternatives and securing funds too. Further, related to the need for comprehensive training programs, there’s also a requirement for occupational therapists to have specialized training to effectively use these types of technologies. Successful integration requires collaboration between neuroscientists, engineers, and occupational therapists. These approaches can be improved through an interdisciplinary team which will ensure that neuroscience advancements are used to create better therapy.
Although it has some limitations such as a small sample size and inadequate duration of intervention. To evaluate the long-term effects of those interventions necessitate larger, multicentre trials with extended follow-up periods in future research. Furthermore, wearable sensors and AI-driven rehabilitation platforms may be integrated into stroke rehabilitation. Through connecting neuroscience with occupational therapy, stroke rehabilitation can greatly be enhanced. This can be possible by incorporating neuroplasticity, BCIs as well as VR-based techniques into personalized plans targeting motor and cognitive recovery. For the progression of this sector and to make sure that these technologies are brought closer to daily clinic activities, it is important that research be carried on and individuals collaborate as well. If such challenges as the cost of the equipment, its availability, or training are not dealt with accordingly, these interventions will not realize their full potential. Therefore, the affiliation between neuroscience and occupational therapy can result in better rehabilitation effects for stroke patients.
References
- Farbern SD (1989) Neuroscience and Occupational Therapy: Vital Connections. The American Journal of Occupational Therapy 43: 637-646.
Indexed at, Google Scholar, Crossref
- Thompson BL, Rider JV, Frechette A (2023) Using neuroscience education to address chronic pain. The American Journal of Occupational Therapy 28: 10-14.
Google Scholar
- Catani M, Sandrone S (2015) Brain Renaissance: From Vesalius to Modern Neuroscience. Oxford University Press.
Google Scholar
- Wolf SL (2006) Effect of Constraint-Induced Movement Therapy on Upper Extremity Function 3 to 9 Months after Stroke. Randomized Controlled Trial 296: 2095-2104.
Indexed at, Google Scholar, Crossref
- Cicerone KD, (2000) Evidence-based cognitive rehabilitation: updated review of the literature from 1998 through. Arch Phys Med Rehabil 81: 1684-1692.
Indexed at, Google Scholar, Crossref
- Walker MF, Clarke T, Lincoln NB (1999) Evaluation of a cognitive and functional skills training program to promote independence in stroke patients. Clinical Rehabilitation 13: 478-487.
Google Scholar
- Daly JJ, Ruff RL (2007) Feasibility of combining multi-channel functional neuromuscular stimulation with weight-supported treadmill training. Journal of Neurological Sciences 253: 45-56.
Indexed at, Google Scholar, Crossref
- Crasta JE (2024) The NeuRO Lab: NeuROscience Research in Occupational Therapy. The Ohio State University.
Google Scholar
- American Occupational Therapy Association (2023) Linking Neuroscience, Function, and Intervention: A Scoping Review of Occupational Therapy Research. The American Journal of Occupational Therapy 71:7105100040-71051000401.
Google Scholar
- Taub E, Uswatte G, Pidikiti R (1999) Constraint-Induced Movement Therapy: A new family of techniques with broad application to physical rehabilitation-a clinical review. Journal of Rehabilitation Research and Development 36: 237-251.
Indexed at, Google Scholar
- Cramer SC, Nudo RJ (2010) Brain repair after stroke 41:10.
Google Scholar
- Kwakkel G, Kollen BJ, Lindeman E (2004) Understanding the pattern of functional recovery after stroke: facts and theories. Restorative Neurology and Neuroscience 22: 281-299.
Indexed at, Google Scholar
- Daly JJ, Wolpaw JR (2008) Brain-computer interfaces in neurological rehabilitation. The Lancet Neurology. 7:1032-1043.
Indexed at, Google Scholar, Crossref
- Gharabaghi A (2016) What turns assistive into restorative brain-machine interfaces?. Frontiers in Neuroscience 10: 456.
Indexed at, Google Scholar, Crossref
- Biasiucci A, Leeb R, Del R Millán J (2010) Brain-machine interfaces and neurorehabilitation. Handbook of Neuroengineering 2: 641-658.
Google Scholar
- Laver K (2015) Virtual reality for stroke rehabilitation. Cochrane Database of Systematic Reviews 11: CD008349.
Indexed at, Google Scholar, Crossref
- Rizzo AA, Kim GJ (2005) A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence: Teleoperators & Virtual Environments 14: 119-146.
Indexed at, Google Scholar, Crossref
- Saposnik G, Levin M (2011) Stroke Outcome Research Canada (SORCan) Working Group. Virtual reality in stroke rehabilitation. A meta-analysis and implications for clinicians 42: 1380-1386.
Indexed at, Google Scholar, Crossref
- Field A (2013) Discovering Statistics Using IBM SPSS Statistics. Sage.
Google Scholar
- Pallant J (2016) SPSS Survival Manual. McGraw-Hill Education.
Google Scholar