Keywords
Ergonomics; GDP: General Dental Practitioners; WMSD: Work Related Musculoskeletal Disorders; CDE: Continued Dental Education
Key message
The prevention and reduction of WMSDS among dentists should include their education in ergonomic principles as applied to dental practice and awareness regarding the importance of work related risk factors.
Occupational health hazards due to dental practice among dental professionals are on a continuous rise resulting in a significant negative impact on the overall quality of life. Dentists tend to assume stressful body positions due to work place restrictions, and to obtain better access and visibility to the operating site. This results in isometric contractions of large group of muscles involving head, neck and shoulders- the cumulative effect known as Cumulative trauma disorders (CTD) [1]. (CTD) or repetitive strain injuries [2] (RSI) or occupational overuse syndromes [3] (OOS) of the musculoskeletal system or work-related musculoskeletal disorders [4] (WRMSDs) - Musculoskeletal Disorders has been defined by W.H.O [5,6] as “disorders of the muscles, tendons, peripheral nerves or vascular system not directly resulting from an acute trauma or instantaneous event”. Two most common Cross sectional study causes for musculoskeletal disorders in the dental health profession are cumulative traumas & prolonged static postures. Studies reported prevalence of WRMSDs among nurses, [7] physical therapists, [8] physicians, [9] surgeons, [10] and dentists [11].
Literature suggests that the symptoms of pathological conditions which are prevalent in the upper body regions are more common among dentists than subjects working the different environment such as farmers, pharmacists and office employees [12]. Scientific research works by Rising et al. [13], Ayers et al. [14] and Al Wazzan [15] correlating ergonomics in dental procedures suggested that dental professional, whether they are dentists, dental hygienists or assistants, experienced more neck, shoulder and back pain than practitioners in other Profession. National differences were found to exist in work-related attitudes [16] which in turn influence work performance and WRMSD prevalence.
Several studies shows relationship between inadequate posture while doing clinical practice and appearance of pain in the various muscles of the body [17-19]. Unthank showed in his study that Lighting at the work place: the lack or excess of light can generate myopia and irreversible retinal lesions, among others [20].
Ergonomics is the Science that fits the job to a person’s anatomical physiological and psychological characteristics in such a way that it enhances human efficiency and well-being (International ergonomic Association). It is the Science that designs tools, equipments, work stations that fits the job to the worker and not worker to the job. Physically challenging nature of work in dentistry combined with the risk factors such as prolonged static postures, repetitive movements, working in a confined space, challenges in positioning the practitioner or the patient and the limitations with the tools and equipments used results in poor ergonomics. These factors can initiate progress or worsen the musculoskeletal disorders. The present study is an attempt to understand the incidence and prevalence of musculoskeletal disorders among the general dental practitioners (GDP) in Mysore district, categorize them according to its type and severity, understand the risk factor involved and to utilize appropriate ergonomic principles to reduce the occurrence of WMSD.
Aim of this study
1. assess the awareness about ergonomically designed work station to reduce the effect of WMSD
2. to find the correlation of the ergonomic factors and its association with age, gender, musculoskeletal problems due to wrong postures
3. identify prophylactic measures used as self-management strategies for prevention so as to promote a healthy professional and personal life during the professional practice
Materials and Methods:
Study design: An epidemiologic survey was conducted to assess the awareness and practices of ergonomics among General dental practitioners of Mysore district- which was the inclusion criteria, the exclusion criteria was-subjects suffering from any kind of medical problems (arthritis, fracture etc).
A self-administered Questionnaire was designed to obtain information about the awareness of ergonomic practices, the possibility of postural risk factors affecting them and the nature of treatment they seek were also included in the study during the period of August 2012- December 2013.
Study population: A list of the dental practitioners with contact numbers was obtained from the IDA (Indian Dental Association) Mysore branch. Prior appointment was taken through telephone and a self-administered questionnaire was handed over to the dental practitioners at their respective clinics. Out of 260 General Practitioners 120 agreed to participate in the questionnaire in the study. Participation in the study was voluntary and informed consent was duly signed by the participants. The response rate was 56.07%. The method of sampling questionnaire in this study is depicted in (Table 1).
Table 1: Method of sampling questionnaires in this study.
| |
Total participants |
Contacted |
consented |
Returned |
included |
Response rate |
| Frequency |
335 |
290 |
214 |
120 |
120 |
120/214 |
| Percent |
100.0 |
86.57 |
63.9 |
35.8 |
35.8 |
56.07 |
Questionnaire development and screening validation: The method for answering the questionnaire was explained and the questionnaire was collected according to the convenience of the practitioners over a maximum period of one week. The screening questionnaire had a total 15 questions. Prior to the study, the questionnaire was tested for comprehensibility and relevance among ten dentists. The purpose of the questionnaire and how they should be answered was explained, and whenever necessary further information was provided.
Questionnaire description: The variables included in the questionnaire were information on the demographic details, respondent's individual characteristics, job history, years of experience and method of work, , and musculoskeletal complaints which were identified defined by the presence or absence of pain in each specific body region using standardized Nordic questionnaire [21-23]. This questionnaire records the prevalence of MSD in terms of musculoskeletal symptoms (ache, pain, discomfort) in the preceding 12 months. SNQ consists of structured, forced, binary, or multiple choice variants and prophylactic methods adopted in relation to musculoskeletal complaint. The SNQ includes a diagram of the human body viewed from the back, divided into nine anatomical areas. This helps the subjects in identifying the areas of the body to which the questions are directed. These areas have been shown to accumulate musculoskeletal symptoms and are distinguishable from each other by the responder [21]. The recording also included demographic variables such as age, gender, qualification, duration of practice, average patients seen per day, nature of practice, and whether the subjects were right handed or left handed.
Participation confidentiality: Each dentist was presented with a separate copy of the questionnaire personally by the investigators (M&R) and requested to answer the questions which was collected on the same day or the previous day. Written notification was received from the private dental practitioners confirming that the participation in the study was voluntary. Informed consent was duly signed by the participants included in the study.
Data analysis: Data gathered was statistically analyzed using SPSS software version 16 using chi-square test. The chi-square values were calculated. P-value of p<0.05 was considered to be significant. The results were presented by a simple bar graph. A Chi- square test with 95% of probability and 0.5% margin error was done to establish differences when relating two qualitative variables and, to find out if there was statistical significance or were due to chance.
Results
In the present study the prevalence of various health hazards among general dentists practicing in Mysore district was interpreted. A total of 260 dentists who were members of IDA Mysore branch were surveyed out of which 120 general dentists agreed to participate in the study.
Gender: According to the study 40.8% samples corresponded to females and 59.2% samples were males who responded to the questionnaire.
Age: 108 dentists were between 31-50 years of age where as 12 were above 51 years of age.
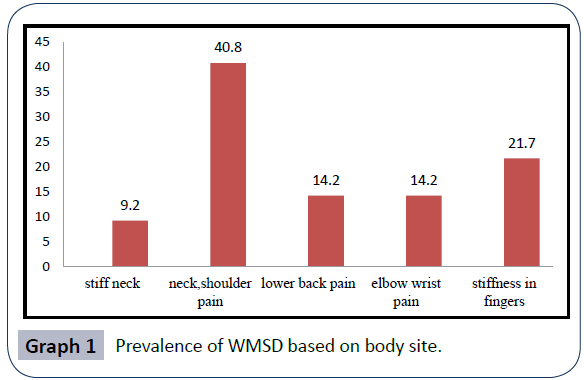
Out of120 dentists, 60 dentists had neck and shoulder pain, 17 dentists had low back pain, 17 dentists had elbow and wrist pain and 26 dentists had stiffness of fingers. Many of the dentists had two or more of the above mentioned physical limitations (Graph 1).
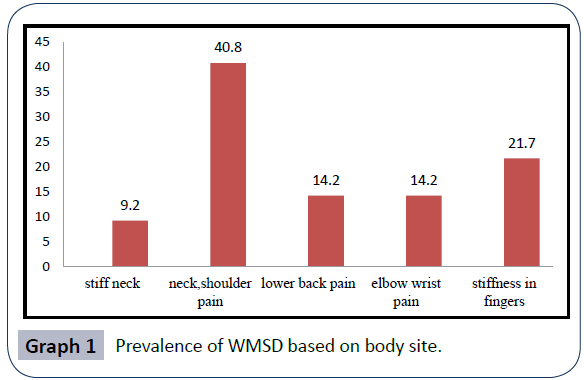
Graph 1: Prevalence of WMSD based on body site.
The number of hours they practice a day was also a crucial deciding factor. Of the sample of 120, incidence of WMSD was observed in 33.3% of GDP who practiced for less than 4 hours 58.6% GDP who practiced for 4-6 hours, and 70.2% of GDP who practiced for 6hours and above. This clearly showed that the incidence of WMSD increased with hours of practice.
In the present study, GDP who had 5 years of experience, 73.1% practiced sitting dentistry, 26.9% practiced standing dentistry. GDP who had experience above 5 years of experience, 7.4% practiced sitting dentistry, 44.7% practiced standing dentistry, 47.9% practiced both sitting and standing dentistry.
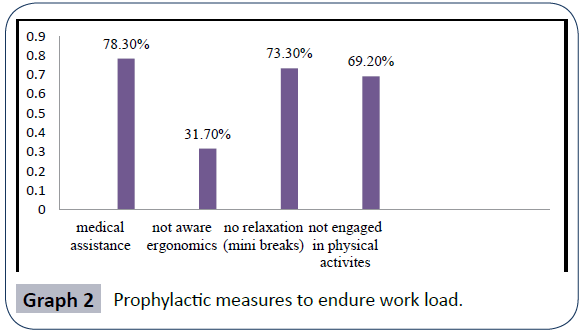
Awareness: In the present study 94 dentists (78.3%) have undertaken medical assistance/physiotherapy for experiencing musculoskeletal complaints. 31.7% were not aware of the term ergonomics and 68.3% were aware of the ergonomic principles. But, when questioned about utilization of ergonomically designed dental chair and equipment in their practice, 55.8% of the dentists were not following the usage (Graph 2).
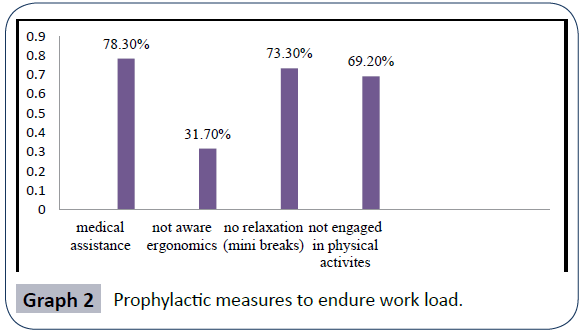
Graph 2: Prophylactic measures to endure work load.
Relaxation while working: Present study showed that around 73.3% of the practitioners do not relax by taking mini breaks and 26.7% take mini breaks while working, when questioned whether they perform any of the hand exercises after the dental procedure, only 37.5% perform some form of hand exercises such as all fingers spread. Around 69.2% of the dentists are not engaged in any form of physical activities/exercise as a prophylactic measure to endure the work load. Thus the results clearly demonstrate that the WMSD was directly related to the number of hours they practice and also sedentary life style and not involved in any form of physical activities.
Discussion
Published literature has shown a high prevalence of MSD among dentists [24-27]. The sedentary nature of work together with altered posture and lack of application of ergonomic principles can result in the imbalance of specific group of muscles. This Study was undertaken to determine the prevalence and distribution of WMSD among GDP of Mysore district. Musculoskeletal disorders are a diverse group of disorders with reference to pathophysiology. According to WHO WMSD is often accompanied by pain and impaired functioning related to musculoskeletal system or in relation to the cause such as joint disease/trauma [28]. The instrument used in this study is a self-administered Questionnaire and SNQ which records musculoskeletal symptoms and screens for musculoskeletal disorders in an ergonomic context [21]. It serves as a diagnostic tool for analyzing the work environment and identifying incompatibilities in the working environment [21]. The present study has revealed a prevalence of MSD 77.5% among GDP of Mysore district. This prevalence is higher than that reported in a study in Saudi Arabia (59.2%) but lower that the reports from Australia (87.2%), [29] Lithuania (86.5%) [30] and Turkey (94%) [31]. The prevalence of WMSD among GDP in the present study was higher than the prevalence observed in a cross-sectional study conducted by Bihari et al. in Delhi where the prevalence was 25% among General Indian Population.
The current study revealed no difference in prevalence of MSD between males and female general dental practitioners as compared to study done by Lindfors et al. in 2006 reported that the female group of dentists showed a higher incidence of muscular skeletal disorders.
Dentists predispose to pain/injury in different regions of the body depending on the type of work and position adopted. In the present study, the commonly affected areas were neck and shoulders which accounted for 40.8%, low back pain 14.2%, elbow and wrist 14.2%, stiffness in fingers 21.7% which were similar to the studies from Queensland [29] and New Zealand [32,33], Southern state of AP which showed high prevalence of MSD among GDP regardless of the qualification and specialty, the prevalent site affected was low back and neck. These results indicate that most of the practitioners adopt positions which frequently result in MSD of neck and low back regions. However, Szymanska [34] and Pureine et al. [35] have reported that most revalent musculoskeletal complaint was MSD of low back which could be attributed to forward positioning of the operator to gain access to operating site.
When age of GDP and their practicing hours were associated, a significant association was observed (Contingency co-efficient cc=.534, p=0.000). It was found that those with in the age group of 31-50 years were more into practice between 4-6 hours and above 6hours. However, in the case of GDP with more than 51 years, were into dental practice for less number of hours and very few of them were practicing for 4-6 hours and above 6 hours (Table 2).
Table 2: Age and hours of practice- a significant association was observed (Contingency co-efficient cc=.534, p=0.000).
| Age vs. Hours of Practice |
| |
|
|
AGE |
Total |
| 31-50 y |
51+ |
| Hours of Practice |
<4 |
Count |
6 |
9 |
15 |
| % of participants |
5.6% |
75.0% |
12.5% |
| 4-6 |
Count |
57 |
1 |
58 |
| % of participants |
52.8% |
8.3% |
48.3% |
| 6+ |
Count |
45 |
2 |
47 |
| % of participants |
41.7% |
16.7% |
39.2% |
| Total |
Count |
108 |
12 |
120 |
A significant association was observed between practicing hours and WMSD where contingency co-efficient value .227 was found to be significant at .038 level. From the table it is clear that with increasing and age, incidence of WMSD also increased linearly and significantly (Table 3). The number of hours of practice play an important role in the occurrence of MSDs although both younger and older dentists report the same symptoms as confirmed in other studies [36]. In contrast to other studies done among GDP of Saudi Arabia and New South wales, where MSD decreased with age and duration of Practice [37-39] which could be attributed to older practitioners taking up less number of patients as a result of age /years of practice or having undertaken selective measures adjusting position while working, involved exercises and relaxation breaks for MSD. Our study is in agreement with the study conducted in AP which showed high prevalence of MSD among GDP regardless of the qualification and specialty and the most prevalent site affected was low back and neck.
Table 3: A significant association was observed between practicing hours and WMSD where contingency co-efficient value .227 was found to be significant at .038 level.
| Hours of practice vs. prevalence of WMSD |
| |
|
|
WMSD |
Total |
| + |
_ |
| Hours of practice |
<4 |
Count |
5 |
9 |
15 |
| % of participant |
33.3% |
66.7% |
100.0% |
| 4-6 |
Count |
34 |
24 |
58 |
| % of participant |
58.6% |
41.4% |
100.0% |
| 6+ |
Count |
33 |
14 |
47 |
| % of participant |
70.2% |
29.8% |
100.0% |
| Total |
Count |
72 |
48 |
120 |
| % % of participant |
100.0% |
100.0% |
100.0% |
Hours of practice vs. prevalence of WMSD
In the present study, 73.3% of GDP were not involved in any kind of rest breaks during their practice. The results were consistent with the studies by Szymanska [34] who discovered that more than 30% of dentists work without breaks.
A significant association was observed between years of experience and body posture (cc=.559; P=0.000). It was found that most of GDP with less experience were practicing sitting dentistry followed by standing. GDP with more than 5 years of experience were practicing alternative sitting and standing dentistry instead of sitting posture alone. GDP with 0-5 years of experience, 73.1% of them adopt sitting dentistry and GDP above 5 years of experience, 7.4% adopt sitting dentistry, 44.7% adopt sitting and standing /postural alterations. Ratzon et al. [40] conducted a study to determine the effect of work posture on musculoskeletal complaints. And concluded that those working in sitting position alone had more severe low back pain than those who alternated between sitting and standing positions (Table 4).
Table 4: Hours of dental practice vs. type of dental practice A significant association was observed between years of experience and body posture (cc=.559; P=0.000).
| Hours of dental practice vs. type of dental practice |
| |
|
|
Type of dental practice |
Total |
| sitting |
stand |
Both |
| Years of experience |
0-5 |
count |
19 |
7 |
0 |
26 |
| % of participants |
73.1% |
26.9% |
.0% |
100.0% |
| 5+ |
Count |
7 |
42 |
45 |
94 |
| % of participants |
7.4% |
44.7% |
47.9% |
100.0% |
| Total |
Count |
26 |
49 |
45 |
120 |
| % of participants |
21.7% |
40.8% |
37.5% |
100.0% |
Hours of dental practice vs. type of dental practice
The inference we get through this study is that sedentary nature of work together with faulty posture –fewer repetitive motions, work place constrictions and lack of application of ergonomic principles can result in the imbalance of specific group of muscles. Operators strive to maintain a balance posture while 50% of their body’s muscles are made to contract to hold the body motionless. The awkward posture retained for prolonged periods of time can cause irreversible damage to the muscles thus causing a threat to dentist’s career. It is postulated that upper limb muscles and skeleton are more implicated during dental operation rather than other sites of the body. Åkesson et al. [41] assumed that the work posture of dentists plays an important role as a risk factor for the development of work-related disorders. A high frequency of MSDs among dentists was confirmed in numerous subsequent studies [42-44]. Maintaining poor posture for long periods of time, can result in chronic muscular fatigue, discomfort or pain, even if the soft tissues are not structurally altered. More significantly, prolonged exposure to high static muscle and joint load may lead the soft tissues to adaptively change, and with time may lead to pathological effects and permanent disability [44-51]. Finsen et al. [45] presumed that an increased variation in work postures may reduce the risk of overloaded spine and lower and upper limbs. Newell and Kumar [42] confirmed that attention and awareness of MSDs in the dental profession has noticeably increased due to a rise in the number of reported MSDs. Some of the improper postures that detour the dentist to the route of ill health are working with neck in flexion, with shoulders elevated, or either flexed and abducted, side bending to left or right, forward bending or over reaching at waist, excessive twisting, elbows getting flexed greater than 90°, thumb hyperextension and wrists getting flexed in grasping [46]. Maintaining the same position for more than 40 minutes per patient can also be deleterious. Forceful pinching of the instruments during scaling is considered an important risk factor and the use of ergonomically designed instrument significantly helps reducing the musculoskeletal disorders that develop due to the former [47]. Similarly repetitive movements with low task variation had a higher incidence of RSI in dentists, rather than those who practice with varied type of movements [48,49].
Recommendations:
In a nut shell, it is indispensible to change poor work habits.
Some of the Parameters of the correct working postures: [42,50,52]
1. The sitting posture is upright and symmetrical
2. The shoulders hanging down relaxed with the upper arms beside the upper body
3. The minimal elevation of forearms.
4. The angle between lower and upper legs is approx. 105- 110
5. The legs are slightly apart, making an angle of between 30-45°,
6. The position of the back of the patient chair
7. The patient’s head is appropriately rotated in 3 directions
8. The light beam of the dental operating light is as parallel as possible to the viewing
9. The sitting location, between 09.00-12.00 o’clock (for lefthanded people 03.00-12.00 o’ clock position)
10. The patient’s head is rotated and the sitting location adjusted
11. Instruments held in 3 supporting points
Limitations: Subjectivity of responses can be a limitation; practitioners with recent episodes of MSD will remember the events much better and can affect the response to questionnaire. Decreased sample size limits the gereralizability of findings.
Conclusion
Dental surgeons must become more educated regarding the impact of their choices in seating in their work area. Improper adoption of ergonomics may cause untoward changes in our body leading to WMSD. The prevention and reduction of MSDs among dentists should include their education in dental ergonomics through regular CDE programmes and awareness regarding the importance of work-related risk factors.
7272
References
- Baker NA (1999) How useful is the term "Cumulative Trauma Disorder"? Work 13: 97-105.
- McNaughton H (2000) The label 'Occupational Overuse Syndrome': time to change. NZ Med J 113: 193-194.
- Yassi A (2000) Work-related musculoskeletal disorders. CurrOpinRheumatol 12: 124-130.
- Snashall D (1996) ABC of work related disorders. Hazards of work. BMJ 313: 161-163.
- Zeng Y (2009) Review of work-related stress in mainland Chinese nurses. Nurs Health Sci 11: 90-97.
- Westgaard RH (1999) Effects of physical and mental stressors on muscle pain. Scand J Work Environ Health 25 Suppl 4: 19-24.
- Campo M, Weiser S, Koenig KL, Nordin M (2008) Work-related musculoskeletal disorders in physical therapists: a prospective cohort study with 1-year follow-up. PhysTher 88: 608-619.
- Skjørshammer M, Hofoss D (1999) Physician in conflict: a survey study of individual and work-related characteristics. Scand J Caring Sci 13: 211-216.
- Szeto GP, Ho P, Ting AC, Poon JT, Cheng SW, et al. (2009) Work-related musculoskeletal symptoms in surgeons. J OccupRehabil 19: 175-184.
- Hayes M, Cockrell D, Smith DR (2009) A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg 7: 159-165.
- Kierklo A, Kobus A, Jaworska M, Botulinski B (2011) Work-related musculoskeletal disorders among dentists - a questionnaire survey. Ann Agric Environ Med 18: 79-84.
- Rising DW, Bennett BC, Hursh K, Plesh O (2005) Reports of body pain in a dental student population. J Am Dent Assoc 136: 81-86.
- Ayers KM, Thomson WM, Newton JT, Morgaine KC, Rich AM (2009) Self-reported occupational health of general dental practitioners. Occup Med (Lond) 59: 142-148.
- Al Wazzan KA, Almas K, Al Shethri SE, Al-Qahtani MQ (2001) Back & neck problems among dentists and dental auxiliaries. J Contemp Dent Pract 2: 17-30.
- Kirkcaldy BD, Furnham A, Martin T (1998) National differences in personality, socio-economic and work related attitudinal variables. Eur psychol. 3: 255-262.
- Andersson GB (1999) Epidemiological features of chronic low-back pain. Lancet 354: 581-585.
- (1999) Clinical Guidelines for the Management of Acute Low Back Pain, Royal College of Surgeons.
- Unthank M, True G (1999) Interior design for dentistry. J Am Dent Assoc 130: 1586-1590.
- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, et al. (1987) Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. ApplErgon 18: 233-237.
- Dickinson CE, Campion K, Foster AF, Newman SJ, O'Rourke AM, et al. (1992) Questionnaire development: an examination of the Nordic Musculoskeletal questionnaire. ApplErgon 23: 197-201.
- Baron S, Hales T, Hurrell J (1996) Evaluation of symptom surveys for occupational musculoskeletal disorders. Am J Ind Med 29: 609-617.
- Lehto TU, Helenius HY, Alaranta HT (1991) Musculoskeletal symptoms of dentists assessed by a multidisciplinary approach. Community Dent Oral Epidemiol 19: 38-44.
- Lindfors P, von Thiele U, Lundberg U (2006) Work characteristics and upper extremity disorders in female dental health workers. J Occup Health 48: 192-197.
- Hayes J, Smith DR, Cockrell D (2009) Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students International Journal of Dental Hygiene 7: 176–181.
- Morse T, Bruneau H, Dussetschleger J (2010) Musculoskeletal disorders of the neck and shoulder in the dental professions. Work 35: 419-429.
- Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81: 646-656.
- Leggat PA, Smith DR (2006) Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust Dent J 51: 324-327.
- Puriene A, Janulyte V, Musteikyte M, Bendinskaite R (2007) General health of dentists. Literature review. Stomatologija 9: 10-20.
- Polat Z, Baskan S, Altun S, Tacir I(2007) “Musculoskeletal symptoms of dentists from South-East Turkey,” Biotechnology and Biotechnological Equipment, 21: 86–90
- Ayers KM, Thomson WM, Newton JT, Morgaine KC, Rich AM (2009) Self-reported occupational health of general dental practitioners. Occup Med (Lond) 59: 142-148.
- Szymanska J (2002) Disorders of the musculoskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann Agric Environ Med 9: 169-173.
- Puriene A, Aleksejuniene J, Petrauskiene J, Balciuniene I, Janulyte V (2008) Self-reported occupational health issues among Lithuanian dentists. Ind Health 46: 369-374.
- Al Wazzan KA, Almas K, Al Shethri SE, Al-Qahtani MQ (2001) Back & neck problems among dentists and dental auxiliaries. J Contemp Dent Pract 2: 17-30.
- Abduljabbar TA (2000) “Musculoskeletal disorders among dentists in Saudi Arabia,” Pak Oral Dental J, 28: 135–144.
- Marshall ED, Duncombe LM, Robinson RQ, Kilbreath SL (1997) Musculoskeletal symptoms in New South Wales dentists. Aust Dent J 42: 240-246.
- Muralidharan D, Fareed N, Shanthi M (2013) “Musculoskeletal Disorders among Dental Practitioners: Does It Affect Practice?” Epidemiology Research International, vol., Article ID 716897, 2013.
- Ratzon NZ, Yaros T, Mizlik A, Kanner T (2000) Musculoskeletal symptoms among dentists in relation to work posture. Work 15: 153-158.
- Akesson I, Hansson GA, Balogh I, Moritz U, Skerfving S (1997) Quantifying work load in neck, shoulders and wrists in female dentists. Int Arch Occup Environ Health 69: 461-474.
- Newell TM, Kumar S (2004) Prevalence of musculoskeletal disorders among orthodontics in Alberta. Int J IndErgon 33: 99–107.
- Pandis N, Pandis BD, Pandis V, Eliades T (2007) Occupational hazards in orthodontics: a review of risks and associated pathology. Am J OrthodDentofacialOrthop 132: 280-292.
- Finsen L, Christensen H, Bakke M (1998) Musculoskeletal disorders among dentists and variation in dental work. ApplErgon 29: 119-125.
- Sartorio F, Vercelli S, Ferriero G, D'Angelo F, Migliario M, et al. (2005) [Work-related musculoskeletal diseases in dental professionals. 1. Prevalence and risk factors]. G Ital Med LavErgon 27: 165-169.
- Valachi B, Valachi K. (2003) Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 134:1344-1350.
- Dong H, Barr A, Loomer P, Laroche C, Young E, et al. (2006) The effects of periodontal instrument handle design on hand muscle load and pinch force. J Am Dent Assoc 137: 1123-1130.
- Solovieva S, Vehmas T, Riihimäki H, Takala EP, Murtomaa H, et al. (2006) Finger osteoarthritis and differences in dental work tasks. J Dent Res 85: 344-348.
- Szymanska J (2001) Dentist's hand symptoms and high-frequency vibration. Ann Agric Environ Med 8: 7-10.
- Valachi B, Valachi K (2003) Mechanism leading to musculoskeletal disorders in dentistry. J Am Dent Assoc134: 1344–1350.
- Valachi B, Valachi K (2003) Preventing musculoskeletal disorders in clinical dentistry: strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc 134: 1604-1612.
- Katrova LG, Ivanov I, Ivanov M, Pejcheva (2012) “Ergonomization” of the working environment and building up of healthy working posture of dental students. JIMAB. 18:243-250.