Emmanuel Ifeanyi Obeagu1*, Blessing Chimezie Didia2, Getrude Uzoma Obeagu3 and Obioma Azuonwu4
1Department of Health Services, Michael Okpara University of Agriculture, Umudike, Abia State, Nigeria
2Department of Medicine and Surgery, Rivers State University, Rivers State, Nigeria
3Department of Nursing Science, Ebonyi State University, Abakaliki, Nigeria
4Department of Medical Laboratory Science, Rivers State University, Rivers State, Nigeria
*Corresponding Author:
Emmanuel Ifeanyi Obeagu
Department of Health Services
Michael Okpara University of Agriculture
Umudike, Abia State, Nigeria
Tel: +2348037369912
E-mail: emmanuelobeagu@yahoo.com
Received Date: October 01, 2017; Accepted Date: October 27, 2017; Published Date: November 06, 2017
Citation: Obeagu EI, Didia BC, Obeagu GU, Azuonwu O (2017) Evaluation of Changes in Haematological Profile of Cerebral Malaria Patients in Enugu State, Southeast, Nigeria. Ann Clin Lab Res Vol.5: No.4:202. DOI: 10.21767/2386-5180.1000202
Keywords
Haematological profile; Cerebral malaria patients; Enugu state
Introduction
Malaria parasitaemia is one of the most important causes of child mortality worldwide, the most frequently encountered in Nigeria and other parts of the world is Plasmodium falciparum which annually kills not less than 1 Million children in Africa alone [1,2]. This death toll is only one aspect of the global burden of malaria. P. falciparium is estimated to cause about half a billion episode of disease each year [3] and there are hundreds of millions of course due to other parasite species- Plasmodium vivax, Plasmodium malaria, and Plasmodium ovale [3]. Malaria is one of the most important vector born disease, leading to significant morbidity and mortality, transmission of which occurs in all six WHO regions. Globally, an estimated 3.3 billion people are at risk of being infected with malaria and developing disease, and 1.2 billion are at high risk. High risk population is those living in sub Saharan Africa and South-East Asia [4,5]. Approximately 24 million malaria cases and 41000 deaths were reported in 2013 from South Asia, of which 29% deaths were in age group of <5 years of age. It is responsible for major morbidity and mortality in rural paediatric population with varying degrees of presentation. Cerebral malaria (CM) is the most dreaded and not uncommon complication of falciparum malaria and occurs in children under five years of age [6]. Infection with this parasite can be lethal in the absence of prompt recognition of the disease and its complications and urgent appropriate patient management [7].
Materials and Methods
Study area
The study was done in Niger Foundation Hospital, Independence Layout, Enugu, Nigeria.
Study design
The study is a hospital based case study using purposive sampling technique.
Subjects
The subjects comprised of a total of seventy (70) subjects, 20 subjects were patients aged 1-5 years diagnosed with cerebral malaria and 50 subjects were apparently healthy individuals aged matched as the control.
Ethical consideration
Informed consents were obtained before sample collection and the confidentiality of the results ensured.
Statistical analysis
The results were presented in tables as mean and standard deviation and student t-test used for analysis and the level of significance was set at P<0.05.
Haematological investigation
The haematological investigations were done using Mindray BC-5300.
Results
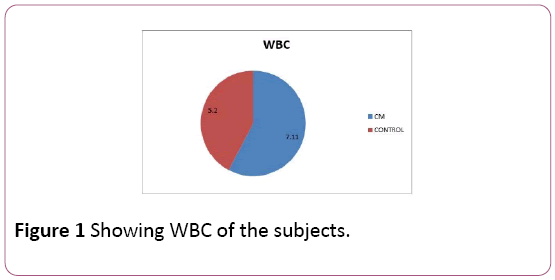
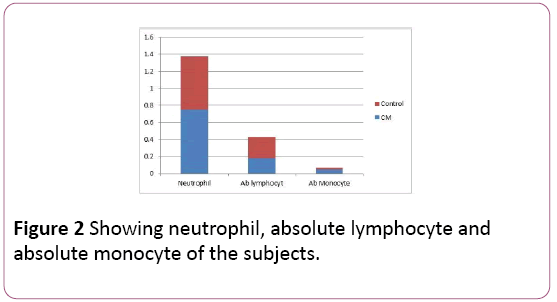
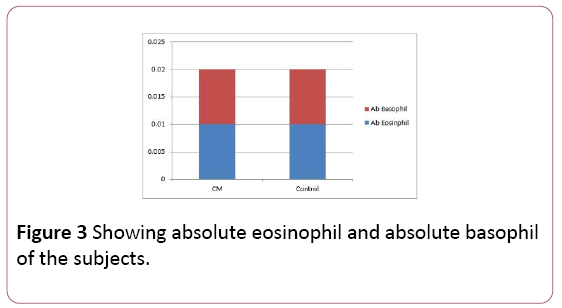
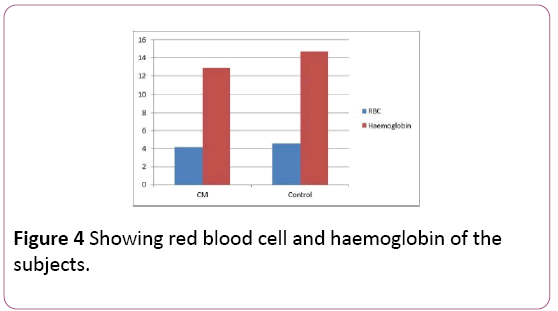
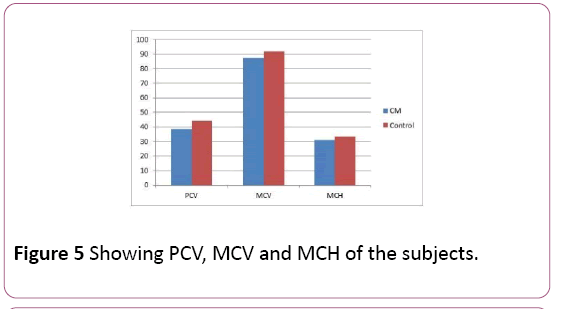
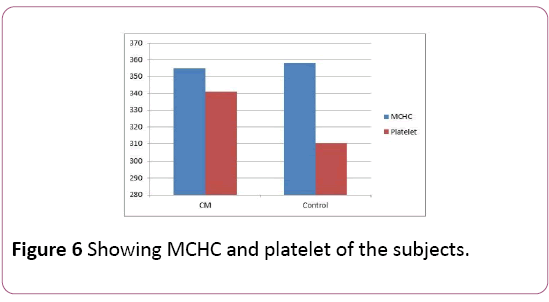
The results showed significant increase (P<0.05) in WBC and platelets of the cerebral malaria subjects (7.11 ± 2.30 × 109/L, 341.00 ± 26.29 × 109/L) compared to the control (5.20 ± 1.56 × 109/L, 310.00 ± 15.06 × 109/L, significant decrease in RBC, Haemoglobin, PCV, PCV, MCV, MCH and MCHC of the cerebral malaria subjects (4.16 ± 0.82 × 1012/L, 12.90 ± 1.30 g/dL, 38.70 ± 3.82%,87.40 ± 8.34 fl, 31.00 ± 2.86 pg, 355.00 ± 20.02 g/L) compared to the control (4.62 ± 0.54 × 1012/L, 14.70 ± 1.76 g/dl, 44.10 ± 6.36%, 92.00 ± 10.21 fl, 33.40 v1.34 pg, 358.02 ± 17.6 g/L) and no significant difference in absolute neutrophils, absolute lymphocyte, absolute monocyte, absolute eosinphils, absolute basophils of the cerebral malaria subjects (0.75 ± 0.12 × 109/L, 0.18 ± 0.10 × 109/L, 0.05 ± 0.01 × 109/L, 0.01 ± 0.01 × 109/L, 0.01 ± 0.01 × 109/L) compared to the control (0.62 ± 0.16 × 109/L, 0.25 ± 0.12 × 109/L, 0.02 ± 0.01 × 109/L, 0.01 ± 0.01 × 109/L, 0.01 ± 0.01 × 109/L) respectively (Table 1) (Figures 1-6).
| Parameters |
CM(20) |
Control(50) |
Level of significance |
| WBC (× 109/L) |
7.11 ± 2.30 |
5.20 ± 1.56 |
P<0.05 |
| Absolute neutrophil (× 109/L) |
0.75 ± 0.12 |
0.62 ± 0.16 |
P>0.05 |
| Absolute lymphocyte (× 109/L) |
0.18 ± 0.10 |
0.25 ± 0.12 |
P>0.05 |
| Absolute monocyte (× 109/L) |
0.05 ± 0.01 |
0.02 ± 0.01 |
P>0.05 |
| Absolute eosinophil |
0.01 ± 0.01 |
0.01 ± 0.01 |
P>0.05 |
| Absolute basophil (× 109/L) |
0.01 ± 0.01 |
0.01 ± 0.01 |
P>0.05 |
| RBC (× 1012 /L) |
4.16 ± 0.82 |
4.62 ± 0.54 |
P<0.05 |
| Haemoglobin (g/dL) |
12.90 ± 1.30 |
14.70 ± 1.76 |
P<0.05 |
| PCV (%) |
38.70 ± 3.82 |
44.10 ± 6.36 |
P<0.05 |
| MCV (fl) |
87.40 ± 8.34 |
92.00 ± 10.21 |
P<0.05 |
| MCH (pg) |
31.00 ± 2.86 |
33.40 ± 1.34 |
P<0.05 |
| MCHC (g/l) |
355.00 ± 20.02 |
358.02 ± 17.61 |
P<0.05 |
| Platelet (× 109/L) |
341.00 ± 26.29 |
310.00 ± 15.06 |
P<0.05 |
WBC: Total White Blood cell; RBC: Red Blood Cell; PCV: Packed Cell Volume; MCV: Mean Cell Volume; MCH: Mean Cell Haemoglobin; MCHC: Mean Cell Haemoglobin Concentration
Table 1: Showing haematological parameters of the cerebral malaria subjects and the control.
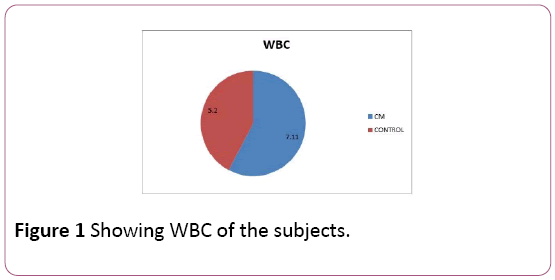
Figure 1: Showing WBC of the subjects.
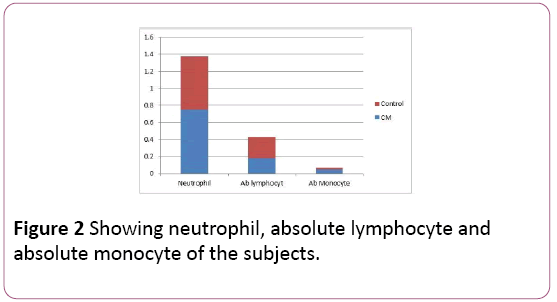
Figure 2: Showing neutrophil, absolute lymphocyte and absolute monocyte of the subjects.
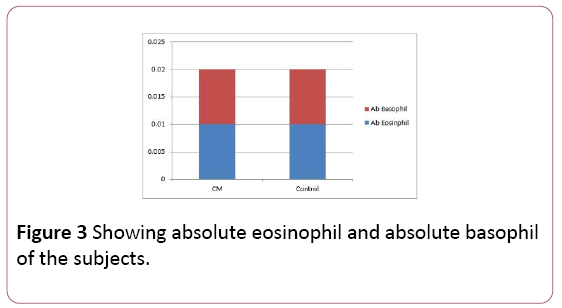
Figure 3: Showing absolute eosinophil and absolute basophil of the subjects.
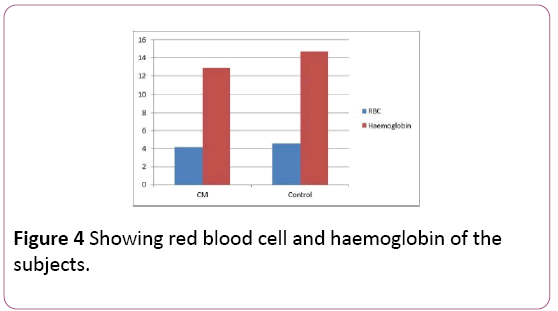
Figure 4: Showing red blood cell and haemoglobin of the subjects.
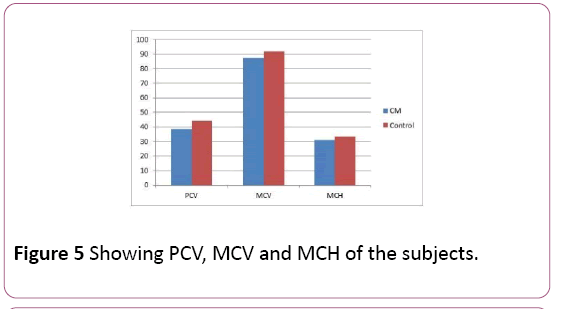
Figure 5: Showing PCV, MCV and MCH of the subjects.
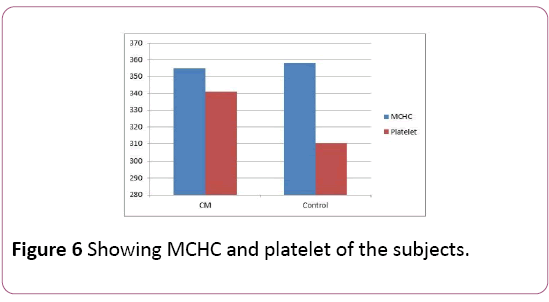
Figure 6: Showing MCHC and platelet of the subjects.
Discussion
The study showed elevation in total white cell and platelets of the cerebral malaria subjects compared to the control and reduced red blood cells, haemoglobin, packed cell volume, cell volume, mean cell haemoglobin and mean cell haemoglobin concentration. This shows that cerebral malaria stimulates the release of leucocytes as a result of infection and stress. The red cell line is reduced significantly showing that anaemia may be one of the consequences of cerebral malaria to the patients. The bone marrow activity may be suppressed and there may be increased destruction of red cells by the reticuloendothelial system.
Falciparum malaria is associated with life-threatening complications in children [2]. It is important for the clinicians in tropical countries to be alert for the symptoms and signs which may progress to life-threatening disease of falciparum malaria [8,9]. The high index of suspicion is rewarding most of the times because the disease has bizarre manifestations, especially in young children; septicaemia and encephalitis illnesses predominate [10].
Anaemia is the important cause for morbidity and mortality in falciparum malaria as seen with this study. The pathogenesis of anaemia in malaria is multifactorial. A complex chain of pathogenetic processes involving mechanical destruction of parasitized RBCs, marrow suppression, ineffective erythropoiesis, and accelerated immune destruction of nonparasitized RBCs have been implicated [11]. Thrombocytopenia was a common observation in falciparum malaria with spontaneous recovery on treatment but in this study, it showed increased thrombocytes. Both leucopenia and leukocytosis have been described in malaria [12,13] but showed significant increase in this study.
Those suffering from this complication of malaria should receive full attention and the haematological parameters should be monitored especially the red cell line which may lead to increase morbidity and mortality. The relatives of the patients should have prompt response in taking them to the hospital when there is any sign of malaria infection so that treatment can commence early and avert the danger associated with cerebral malaria. More enlightenment campaign should be carried out especially to the rural areas and ways of prevention of malaria infection discussed to the populace.
Conclusion
Malaria infection is a serious public heath challenge to humanity in this part of the World with its devastating effects in the entire human systems including the haematological system. Cerebral malaria is seen to impact significantly on the total white cell, red blood cell, packed cell volume, mean cell volume, mean cell heamoglobin, mean cell haemoglobin concentration and platelets. It shows that it may lead to anaemia with it degenerative impact and suppresses bone marrow activity. Adequate health care should be provided to the patients. More attention should be given to prevention of malaria to avoid cerebral malaria as a serious complication and prompt action taken for those infected.
20954
References
- Snow RW, Guera CA, NoovAM,MyintHY,HaysSI (2005)The global distribution of clinical episodes ofPlasmodium falcipariummalaria. Nature 434: 214-217.
- Okoroiwu IL, Obeagu EI,Elemchukwu Q, OcheiKC (2014) Some hematological parameters in malaria parasitaemia.IOSR J Den Med Sci 13: 74-77.
- Snow RN, Trapey JF,Marsh K (2001) The past present and future of childhood malaria mortality in Africa.Trends Parasitol 17: 593.
- Park K (2013) Park’s textbook of preventive and social medicine.(22ndedn). Bhanot.
- World Health Organisation (2014) World malaria report 2014, global and regional malaria trends. WHO. Geneva, Switzerland.
- Phillips RE, Solomon T (1990) Cerebral malaria in children. Lancet 336: 1355-60.
- WHO (2000) New perspectives malaria diagnosis. WHO. Geneva, Switzerland.
- Sharma VP (1996) Re-emergence of malaria in India. Indian J Med Res103: 26-45.
- Mehta SR (1986) Falciparum malaria 210 cases. J Assoc Physicians India 34: 119-20.
- Thapa BR, Mehta S, Singh LM (1985) Complicated chloroquine resistant malaria. Indian J Pediatr 52: 209-212.
- Sen R, Tewari AD, Sehgal PK, Singh U, Sikka R, et al. (1994) Clinico-hematological profile in acute and chronic Plasmodium falciparum malaria in children. J Coin Dis 26: 31-38.
- Lee GR, Foerster J, Leukens J (1999) Wintrobe’s clinical hematology. (10th edn). Bethseda, Maryland: Lippincot Williams and Wilkins, USA.
- Sitalakshmi S, Srikrishna A, Devi S, Damodar P (2003) Changing trends in malaria: A decade’s experience at a referral hospital. Ind J Pathol Microbiol 46: 399-401.