Key words
Visits. Cost. Direct. Economy. Epilepsy. Drugs. Hospitalisation.
Introduction
The economic cost of a disease increases its impact on the patient and his/her family [1]. The most prevalent conditions are the main burdens on a country’s health budget [2]. Health-related economic studies are therefore important in a context of growing healthcare expenditure. The objective of this study is to evaluate the costs associated with the medical management of epilepsy, one of the most common neurological conditions.
Patients and methods
Prospective, observational, 6-month study. Patients over 14 years of age with a diagnosis of epilepsy according to 1989 ILAE criteria [3] were included. To ensure that the costs were attributable to epilepsy, patients with concomitant conditions (tumours, degenerative diseases, metabolic conditions and mental retardation) that could affect its course, therapeutic protocols or the impact of treatment were excluded, even when these conditions were believed to be the cause of the epilepsy.
In order to evaluate the direct medical and non-medical costs of epilepsy, after obtaining the patients’ informed consent in writing, the hospital database containing their medical records was consulted.
Medical direct costs included: number of neurology specialist; primary care and A&E visits for reasons related to epilepsy; number and type of diagnostic tests performed (basic blood test, analysis of anti-epileptic drug levels, brain CT scan, brain MRI, brain SPECT and PET, electrocardiogram, electroencephalogram, electroencephalogram with sleep deprivation, Holter electroencephalogram, video electroencephalogram and Holter electrocardiogram), days of hospitalisation; and the treatment administered (drugs, dose and presentation). Nonmedical direct costs referred to the use of transport to and from hospital and psycho-educational and social support.
The data obtained were translated to monetary units expressed in euros, according to the hospital cost price list (visits, diagnostic techniques, hospitalisation, psycho-educational and social support and healthcare transport) of the Galician Health Service in 2008. Drug prices were taken from the 2008 Medicinal Products Catalogue. As the study lasted for 6 months, the cost of one year was obtained by multiplying the values obtained by two.
Data analysis. The qualitative variables are expressed as absolute frequencies and percentages and the cost-related variables are expressed as mean and standard deviation. The Wilcoxon non-parametric test for paired data was used to assess whether or not cost differences were statistically significant; p-values of less than 0.05 were classified as significant. The data were analysed using the SPSS 15.0 program for Windows.
Results
The study analysed 171 patients, 90 men (52.6%) and 81 women (47.4%). The mean age was 41.6 years, with a standard deviation of 17.0. The patients had been suffering from the disease for a mean of 15.3 years, with a standard deviation of 15.2, although 35 patients (20.5%) were diagnosed in the six months prior to their inclusion in the study.
One hundred and twenty-seven (127) patients (74.3%) were diagnosed with partial seizures and 44 (25.7%) with generalised seizures. Fifty-four (54) patients (31.6%) had cryptogenic epilepsy, 39 (22.8%) idiopathic epilepsy and 78 (45.6%) symptomatic epilepsy.
Sixty-eight (68) patients (39.8%) had no seizures during the study and 103 (60.2%) continued to present seizures, although only 39 (22.8%) suffered more than two, 12 (7%) of whom also visited the epilepsy surgery department.
Nine (9) patients (5.3%) were not receiving treatment, 78 (45.6%) were receiving monotherapy and 84 (49.1%) were receiving more than one anti-epileptic drug. Sixty-one (61) patients (37.7%) were receiving classic drugs, 19 (11.7%) were treated with new drugs, 19 (11.7%) received classic drugs in polytherapy, 57 (35.2%) were taking classic and new drugs in polytherapy and 6 (3.7%) were taking new drugs in polytherapy.
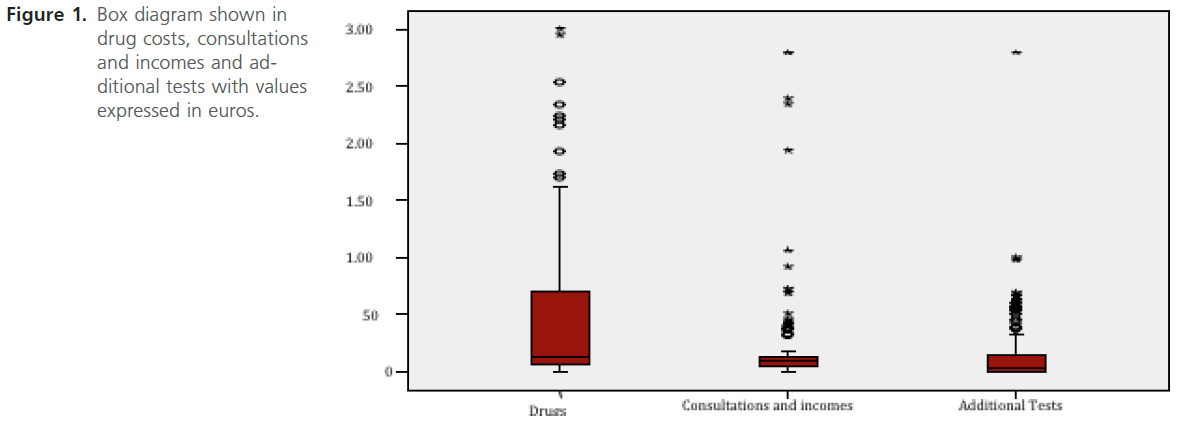
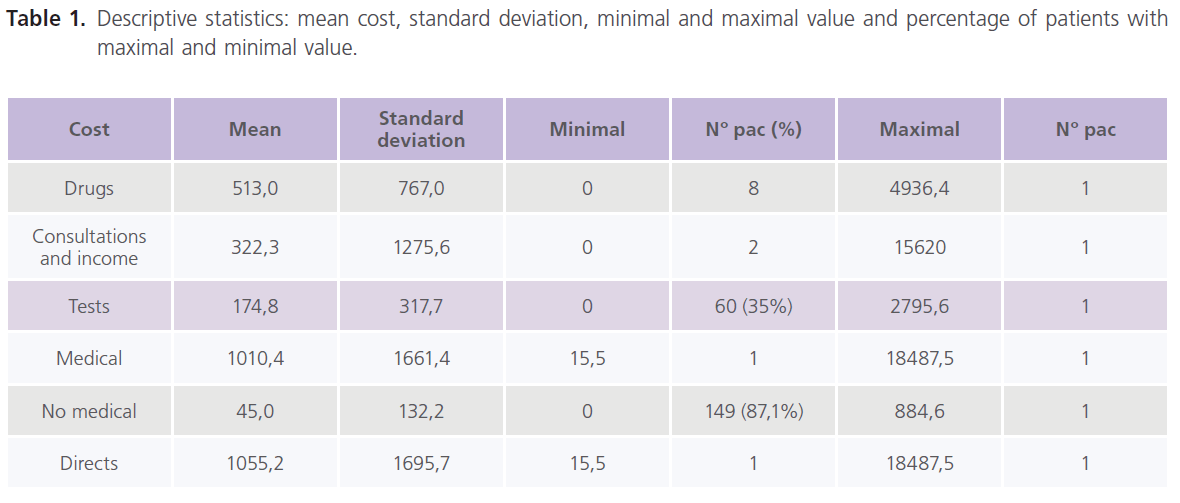
The mean cost of anti-epileptic drugs was 513.6 € per patient, with a standard deviation of 767.0 €; 0 € was the lowest cost because 8 patients were not receiving treatment, and 4,936.4 € was the highest individual amount. The annual cost per patient was 1,027.2 €.
The mean cost of medical visits plus hospitalisations was 322.3 € per patient, with a standard deviation of 1,275.6 €. Two patients had no medical visits or hospitalisations, with a cost of 0 €, while the cost of one patient totalled 15,620 €.
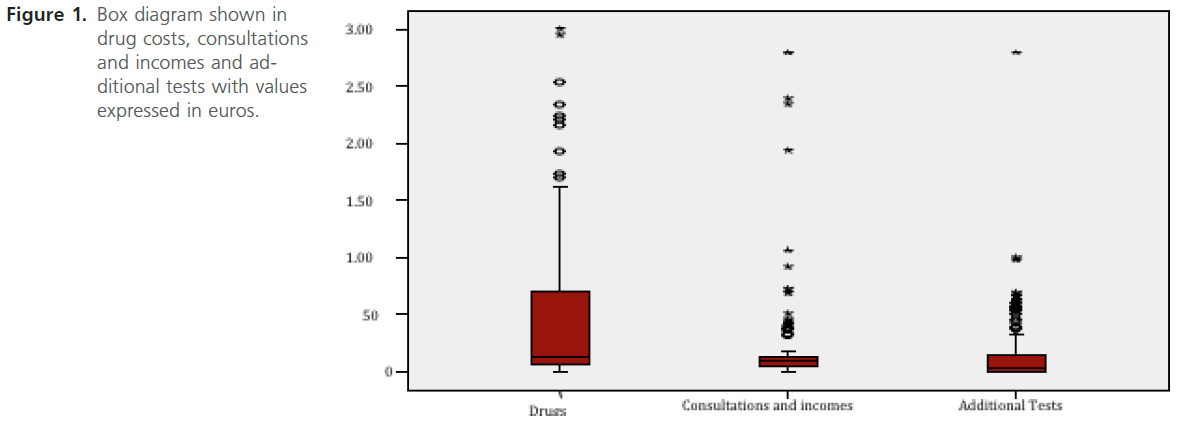
Figure 1: Box diagram shown in drug costs, consultations and incomes and additional tests with values expressed in euros.
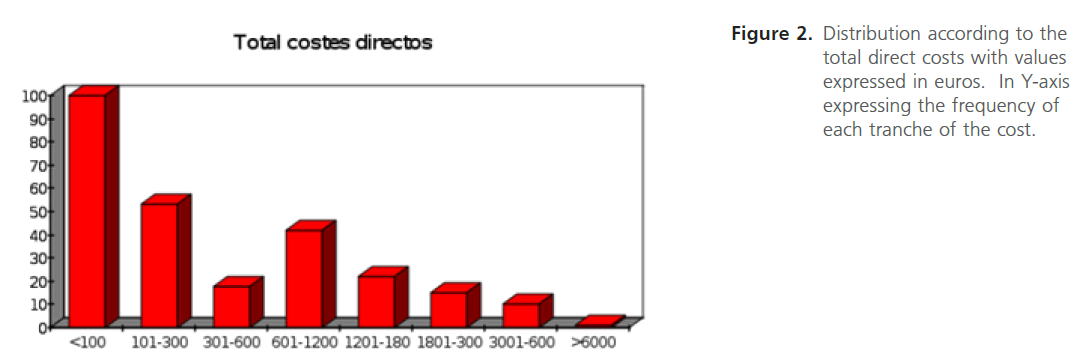
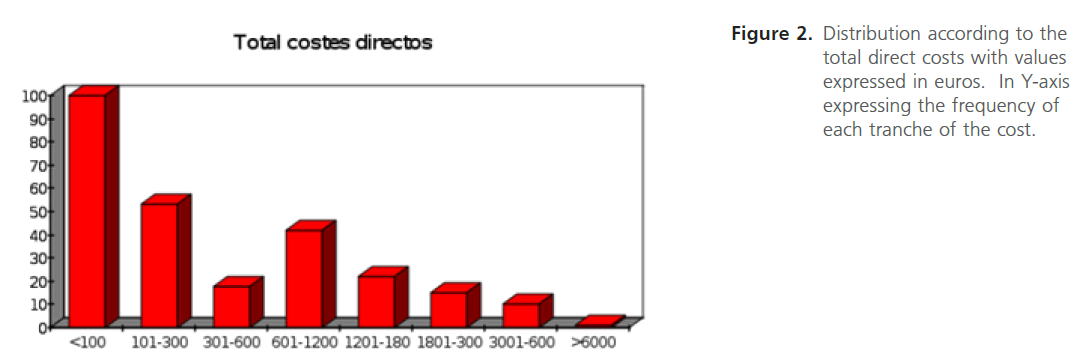
Figure 2: Distribution according to the total direct costs with values expressed in euros. In Y-axis expressing the frequency of each tranche of the cost.
The mean cost of investigations per patient was 174.8 €, with 60 patients generating no expenditure but one with 2,795.6 €.
The mean total medical direct cost per patient was 1,010.4 €, with the lowest being 15.5 € and the highest 18,487.5 €. The mean annual cost per patient was 2,020 €, with expenditure on drugs having the most affect on this figure (p<0.05). In the non-medical direct costs, the mean cost per patient was 45 €, with a standard deviation of 132.2 €. The highest expenditure was 884.6 €, while 149 patients (87.1%) had no spending in this parameter.
Analysing the total direct costs, we find that each study patient represents a mean cost of 1,055.2 €, with a standard deviation of 1,695.7 €. The lowest cost was 15.5 € and the highest 18,487.5 €, with 100 patients (58.4%) generating expenditure of less than 100 €. In the 12 patients (7%) who also visited the epilepsy surgery department, the mean cost was 2,193.2 € (±1193.2 €). Mean annual total direct costs were 2,100.4 € and the difference between medical and nonmedical costs was statistically significant, showing that medical costs have the greatest impact on direct costs (p< 0.05).
Discussion
For the 21st century, the European White Paper on Epilepsy establishes a target of effective care for epilepsy being available for all those who need it, irrespective of borders and economic constraints [4]. In this respect, our study evaluated the costs associated with epilepsy from a social perspective. We obtained data from 171 patients, with a mean age and gender distribution similar to the mean population in Spain in 2006 [5]. We found a predominance of partial seizures and symptomatic epilepsy, similar to the descriptions of community -based population studies [6,7], although obviously the rates for epilepsy of known aetiology depend on the quantity and quality of diagnostic techniques used.
The patients had been diagnosed with epilepsy for a mean of 15.3 years, although approximately 20.5% were diagnosed in the six months prior to their inclusion in the study, so we included both recently-diagnosed patients (incident cases) and patients with long-standing diagnosis (prevalent cases).
Analysing the degree of disease control, we found that only 40% of the patients were seizure-free. This figure is lower than the global prognosis for the control of epilepsy, which considers that 80% of patients achieve remission [8], although the same figure was obtained in other observational, prospective, cross-sectional studies conducted in epilepsy clinics [9,10]. The difference is related to the fact that well-controlled patients do not need monitoring in specialised neurology clinics, and can be followed up by their general practitioners. We may in fact have recruited more patients with uncontrolled epilepsy, who are more likely to be seen by a neurologist.
Forty-five percent (45%) of the patients were receiving monotherapy and nearly 50% polytherapy. Although the basic criterion for treatment of epilepsy is the use of a single drug in order to reduce the risk of undesirable effects, facilitate compliance and reduce the risk of interactions with other drugs, monotherapy is only capable of satisfactorily controlling seizures in around 75% of patients [11]. Consequently, when adequate control is not achieved, after trying a new monotherapy with a different drug, polytherapy needs to be tried using drugs with complementary mechanisms of action based on the principle of rational polypharmacy [12]. A study conducted in Spain showed that, prior to the diagnosis of drug-resistant epilepsy, the most common treatment is monotherapy. After this diagnosis is made, however, the most common treatment is polytherapy, with a mean of 2.2 drugs used [13]. With regard to the 5% of patients who were not receiving any treatment, this could be because they were recently diagnosed and it had not yet been started or that they had stopped treatment for different reasons (side effects, intolerance or patients tired of being on long-term treatment).
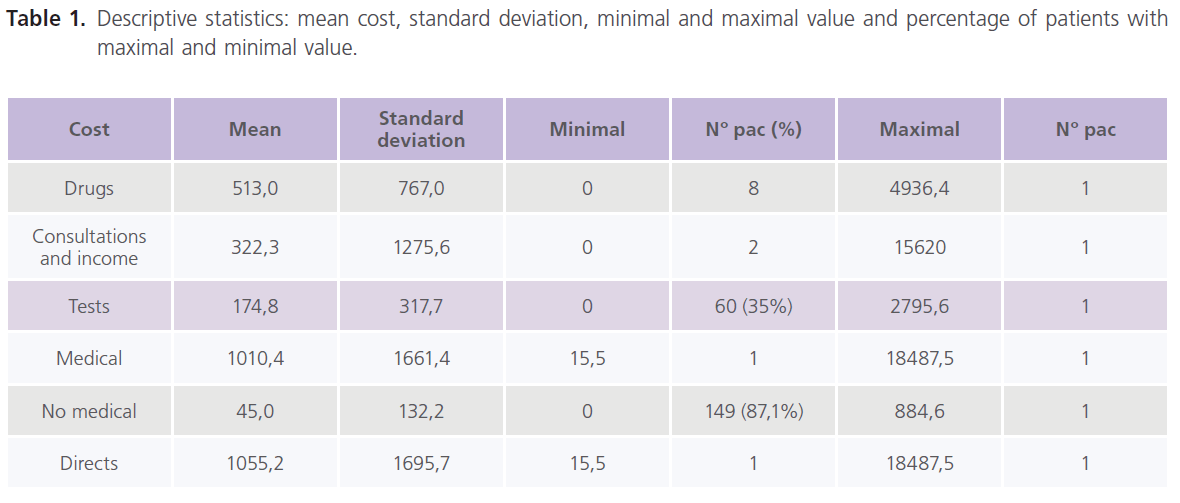
Table 1: Descriptive statistics: mean cost, standard deviation, minimal and maximal value and percentage of patients with maximal and minimal value.
In terms of the type of drug used, most of the patients in monotherapy were receiving a classic drug. In polytherapy, however, the most common option was a combination of classic and new drugs, as reported in other studies [14,16].
The mean cost of anti-epileptic drugs in the 6-month study period was 513.6 € per patient, representing an annual cost of 1,027.2 €, much higher than the mean pharmaceutical expenditure per person in Spain in 2003, which was 224 € [17]. It is clear therefore that the use of anti-epileptic drugs represents a heavy burden for the Spanish health service. Indeed, as a group, anti-epileptic drugs were 10th on the list of most prescribed drug substances in the national health service in 2005 [18], although the patients’ perception of this cost is minimal as anti-epileptic drugs are fully financed by the Spanish health service. In other countries, however, where these costs are covered by the patient, drug prices have a significant impact on prescription habits [19]. At times, drug costs can actually represent 30% of the patients’ regular income [20]. With regard to the large differences in drug costs between individuals, ranging from 0 € to 4,936.4 €, 60% of the included patients suffered seizures despite treatment and 3.7% were receiving polytherapy with new, more expensive, anti-epileptic drugs. The 8 patients with a drug cost of 0 € were newly diagnosed and had not yet started treatment or had stopped treatment due to side effects or because they were tired of being on long-term therapy.
The mean cost of medical visits, including visits to general practitioners, neurologists, A&E and hospitalisations, was 322.3 €; added to the mean cost of investigations, 174.8 € per patient, the total cost of care per epileptic patient was 497.1 € in the 6-month study period. The mean annual cost is therefore 994.2 €, much higher than the mean annual cost per patient in the health service, which was 648 € [17]. However, the real cost difference between epileptic patients and the general population is even greater, as the health service includes the cost of emergency ambulance transport as part of specialist care, while our study included this in nonmedical direct costs. Furthermore, to ensure that the analysed costs were only attributable to epilepsy, we excluded patients with concomitant conditions that could effect the course of the disease or the treatment, even if they were the cause of the seizures, so many of the costs deriving from other associated conditions in epileptic patients were not considered. The large difference found in medical visit and hospitalisation costs between the 2 patients whose cost was 0 € and the 15,620 € generated by another patient was because the former 2 visited the clinic after the 6-month study period; they were nevertheless considered because they show that patients often forget their appointments, especially when their condition is under control. However, the costs of visits and hospitalisation are greater when they involve admission to intensive care unit, above all for the treatment of status epilepticus. With regard to investigations, 60 patients required zero expenditure. This is because, once the disease is diagnosed and suitably controlled, further investigations tend not to be required unless there are side effects or other complications.
The mean direct medical cost associated with epilepsy per patient in the study period was 1,010.4 €, with a large difference between the lowest 15.5 € (a well-controlled patient who forgot an appointment and was receiving a low dose of a classic drug) and the highest 18,487.5 € (a patient who required two lengthy admissions to intensive care and was being treated with two new and one classic drug in polytherapy).
In this respect, the price of drugs has the greatest impact on medical direct costs in both the adult and paediatric population, although its percentage varies from recently diagnosed patients, where cost of hospitalisation is greater, to resistant patients, for whom drug costs are higher, as found in previous studies [1, 21-25]. In the initial studies, however, hospitalisation was most significant in the total amount, because the prescribing of new anti-epileptic drugs was limited to less than 5% of the patients [26-29].
In our study, the mean medical direct costs per patient and year for the control of epilepsy was 2,020 €, much higher than the amount found in studies in other countries such as Chile, Cuba, India or Burundi. This is related to the fact that the shortage of economic resources in these countries causes large differences in patient treatment relative to developed countries. There is less prescribing of new anti-epileptic drugs and use of MRI or other diagnostic tests, so the costs are lower. In any event, the Cuban or Chilean studies did not consider hospitalisation costs as the patients were not hospitalised [25-30]. When we compare our study with another conducted in Spain in a paediatric population, we find that the mean medical direct cost in children is approximately 600 € greater than in adults, because hospitalisation is more common for diagnosis at early ages [1].
On the other hand, the mean non-medical direct cost was 45 € per patient, including transport to or from hospital, particularly use of ambulance transport to A&E, and psychoeducational and social support, although 87% of the patients did not use these services.
Analysis of the total direct costs produces an annual cost of 2,110.4 €, double the mean cost per person in the Spanish health service in 2003 [17]. This shows that epilepsy is a heavy burden for the health service, as it involves a greater need to use the services included in medical direct costs, particularly the purchase of anti-epileptic drugs. We should highlight, however, that 58% of the patients registered a cost of less than 100 € during the 6-month study period.
In comparison with other international studies, therefore, our results show that the direct costs generated by each patient in Spain are nearly 50 times greater than in rural areas of Burundi, but approximately half the expenditure in a tertiary epilepsy centre in Germany [31]. The costs generated by patients vary significantly depending on where they receive care; they are greater in teaching hospitals with advanced equipment, intermediate in general hospitals, where patients are cared for by neurologists specialising in epilepsy but without access to the latest technology, and lower in hospitals where care is provided by a general neurologist [29].
Conclusions
The use of anti-epileptic drugs represents a high cost for the health service. The cost of medical visits, hospitalisations and investigations in epilepsy is higher than the mean annual cost per patient in the health service.
6463
References
- Argumosa, A., Herranz, JL. Economic costs of childhood epilepsy in Spain. Rev Neurol. 2000; 30: 104-8.
- Meerding, WJ., Bonneux, L., Polder, JJ., Koopmanschap, MA., Van der Maas, PJ. Demographic and epidemiological determinants of healthcare costs in Netherlands: cost of illness study. BMJ 1998; 317: 111-115.
- Commission on Classification and Terminology of the Internacional League Against Epilepsy. Proposal for revised classification epilepsias and epileptic syndromes. Epilepsia 1989; 30: 389-99.
- Eucare. European white paper on epilepsy. Eucare UCB S.A. Bruselas. 2002. p. 94.
- INE. Instituto Nacional de Estadística. Población por edad (año a año) y sexo. Revisión del Padrón municipal 2007.
- Manford, M., Hart, YM., Sander, JW., Shorvon, SD. The National General Practice Study of the Internacional League Against Epilepsy applied to epilepsy in a general population. Arch Neurol. 1992; 49: 801-8.
- Zarrelli, MM., Beghi, E., Rocca, WA., Hauser, WA. Incidence of epileptic syndromes in Rochester, Minnesota: 1980-1984. Epilepsia 1999; 40: 1708-14.
- Cockerell, OC., Johnson, AL., Sander, JW., Shorvon, SD. Prognosis of epilepsy: a review and further analysis of the first nine years of the British National General Practice Study of Epilepsy, a prospective population-based study. Epilepsia 1997; 28: 31-46.
- Herranz, JL., Sellers, G. Análisis de datos epidemiológicos de la epilepsia en España. Estudio GABA 2000. Madrid: CIBEST. 1996. p. 84.
- Collaborative Group for the Study of Epilepsy. Prognosis of epilepsy in new referred patients. A multicentre prospective study of the effects of monotherapy on the long-term course of epilepsy. Epilepsia 1992; 33: 45-51.
- Kwan, P., Brodie, MJ. Early identification of refractory epilepsy. N Engl. J Med. 2000; 342: 314-9.
- Perucca, E. Antiepileptic drug monotherapy versus polytherapy: The on-going controversy. Epilepsia 1997; 38: 1-20.
- Rufo-Campos, M., Sancho-Rieger, J., Peña, P., Masramon, X., Rejas-Gutiérrez, J. Grupo de colaboradores del estudio LINCE. Drug regimens in patients with medication-resistant epilepsy in neurology and epilepsy outpatient departments in Spain. Rev Neurol. 2008; 47: 517-24.
- Beghi, E., Garattini, L., Ricci, E., Cornago, D., Parazzini, F. EPICOS Group. Direct cost of medical management of epilepsy among adults in Italy: a prospective cost-of-illness study (EPICOS). Epilepsia 2004; 45: 171-8.
- Landmark, CJ., Rytter, E., Johannessen, SI. Clinical use of antiepileptic drugs at referral centre for epilepsy. Seizure 2007; 16: 356-64.
- Abasolo-Osinaga, E., Abecia-Inchaurregui, LC., Etxeandia-Ikobaltzeta, I., Burgos-Alonso, N., García-del Pozo, J. A pharmacoepidemiological study of antiepileptic drug consumption (1992-2004). Rev Neurol. 2008; 46: 449-53.
- Instituto de estudios fiscales, editores. Informe para el análisis del gasto sanitario. Madrid: Artegraf. 2006.
- Subgrupos ATC y Principios activos de mayor consumo en el Sistema Nacional de Salud en 2005. Información técnica del Sistema Nacional de Salud 2006; 30: 42-9.
- Thomas, SV., Koshy, S., Nair, CR., Sarma, SP. Frequent seizures and polytherapy can impair quality of life in persons with epilepsy. Neurol India 2005; 53: 46-50.
- Thomas, SV., Sarma, PS., Alexander, M., Pandit, L., Shekhar, L., Trivedi, C., Vengamma, B. Economic burden of epilepsy in India. Epilepsia 2001; 42: 1052-60.
- Begley, CE., Annegers, JF., Lairson, DR., Reynolds, TF., Hauser, WA. Cost of epilepsy in the United States: a model based on incidence and prognosis. Epilepsia 1994; 35: 1230-43.
- Tetto, A., Manzoni, P., Millul, A., Beghi, E., Garattini, L., Tartara, A., Avanzini, G. Osservatorio Regionale per l’Epilessia (OREp). The costs of epilepsy in Italy: a prospective cost-of-illness study in referral patients with disease of different severity. Epilepsy Res. 2002; 48: 207-16.
- Forsgren, I., Beghi, E., Ekman, M. Cost of epilepsy in Europe. Eur J Neurol. 2005; 12: 54-8.
- Hamer, HM., Spottke, A., Aletsee, C., Knake, S., Reis, J., Strzelczyk, A., Oertel, WH., Rosenow, F., Dodel, R. Direct and indirect costs of refractory epilepsy in a tertiary epilepsy center in Germany. Epilepsia 2006; 47: 2165-72.
- Mesa, T., Mesa, JT., Guarda, J., Mahaluf, F., Pauchard, F., Undurraga, F., Asmad, C., Silva, G. The direct costs of epilepsy in a Chilean population. Rev Neurol. 2007; 44: 710-4.
- Cockerell, OC., Hart, YM., Sander, JW., Shorvon, SD. The cost of epilepsy in the United Kingdom: an estimation based on the results of the two population-based studies. Epilepsy Res. 1994; 18: 249-60.
- Berto, P., Tinuper, P., Viaggi, S. The Episcreen Group. Cost-of-illness of epilepsy in Italy. Data from a multicenter observational study (Episcreen). Pharmacoeconomics 2000; 17: 197-208.
- De Zélicourt, M., Buteau, L., Fagnanin, F., Jallon, P. The contributing factors to medical cost of epilepsy: an estimation based on French prospective cohort study of patients with newly diagnosed epileptic seizures (the CAROLE study). Seizure 2000; 9: 88-95.
- Guerrini, R., Battini, R., Ferrari, AR., Veggiotti, P., Besana, D., Gobbi, G., Pezzani, M., Berta, E., Tetto, A., Beghi, E., Monticelli, ML., Tediosi, F., Garattini, L., Russo, S., Rasmini, P., Amadi, A., Quarti, P., Fabrizzi, R. Epilepsy Collaborative Study Group. The cost of childhood epilepsy in Italy: comparative findings from three health care settings. Epilepsia 2001; 42: 641-6.
- González-Pal, S., Quintana Mendoza, J., Román López, JR., Fernández- Pérez, JE. The direct cost of epilepsy in Cuba. A study in outpatients. Rev Neurol. 2005; 41: 379-81.
- Strzelczyk, A., Reese, JP., Dodel, R., Hamer, HM. Cost of epilepsy. A systematic review. Pharmacoeconomics 2008; 26: 463-76.