Keywords
Evidence-based medicine; Orthopaedics; Decision-making; Systematic review; Mixed-methods
Introduction
In this study we set out to discover some of the possible underlying drivers for variation in orthopaedic surgical work despite the growing evidence from researchers and policymakers on best practice in orthopaedics. Internationally, the pressure on orthopaedic services is growing. Musculoskeletal (MSK) conditions are a major burden on individuals, health, and social care systems. In the UK for example, the annual budget for treatment of MSK disorders is approximately £10 billion per year [1]. The increasing demands on orthopaedic services brought about by the aging population and rising incidence of arthritis mean that there is a mounting requirement for increasing orthopaedic treatments within a restricted budget. This pressure to deliver more for less has led to patterns of variation in current practice and provision of orthopaedic surgery which are driven by factors unrelated to patient need [2].
Levels of variation are substantial and deemed unacceptable, hence policy making organisations such as the National Institute for Health and Care Excellence (NICE) in the UK and the Agency for Healthcare Research and Quality (AHRQ), the Preventive Services Task Force (USPSTF) in the U.S. set out to standardise care across healthcare systems through the implementation of evidence [3,4]. Evidence-based medicine informs clinical guidelines which are produced to establish clinical effectiveness and criteria for treatments at acceptable levels of expenditure [5,6]. The impact of these evidence-based policies, interventions and recommendations within orthopaedics is unknown, as are the barriers and facilitators to the use of evidence-based medicine in decision-making for orthopaedic surgery.
Previous research dating back to the 1930's highlighted variation in surgical practice across and within geographical areas [7-12] and within different surgical specialties [13,14] and sub-specialties [15,16]. Rates of surgical intervention do not always align to rates of disease. Many reasons are given provided for performing or limiting surgery which may not directly link to the clinical needs of patient or populations [17]. This paper is focused specifically on orthopaedic practice where the rate of joint replacement surgery has been reported to vary by geographical population, hospital and by surgeon [18,19]. Inconsistencies in procedures conducted and the prostheses selected for joint replacement have also been described, as well as significant variation in the level of expenditure and patient reported outcomes [2,20-22].
These differences cannot be explained by differences in the clinical needs of patients and hence it is important to understand the driving forces behind this variation. This research was designed to review and summarise the published literature systematically i) to understand approaches and techniques to knowledge and evidence use, and ii) to identity the factors influencing decisionmaking and practice variation within orthopaedic surgery. Through this systematic review we highlight sources of evidence and knowledge that have been important in decisions made within orthopaedic surgery, and explain how these complex and competing sources of evidence may lead to unjustified variation in practice. We propose a conceptual model to highlight the relationship between evidence sources and practice in healthcare.
Methods
Protocol registration
We used Cochrane Collaboration guidelines to prepare a study protocol for the systematic review [22] and registered with the PROSPERO database: CRD42015016792.
Inclusion and exclusion criteria
We included all study designs and orthopaedic surgical treatments. All healthcare professionals or member of the surgical team involved in decision-making for orthopaedic patients were included. The main outcomes were evidence sources used in decisions and the approaches and techniques to evidence use and uptake. No country restrictions were applied but only English language papers were included. We excluded basic research studies, abstract or conference proceedings, editorials, letters and commentaries; individual case studies and studies including children.
Information sources and selection of studies
Individual studies were identified using a structured electronic search strategy developed for MEDLINE and adapted for other databases. The electronic databases and web resources are listed in Table 1. We scanned reference lists of included studies and contacted key experts in the field. A supplementary search technique was used to search around clusters of papers based on citations, relevant theory and concepts, such as 'evidence-based orthopaedics' [23,24]. Searches were undertaken in February 2014 and included papers published between 1946 to January 2014 (Supplementary file S1).
| Databases |
Web resources and grey literature |
| Medline [OVID] |
King’s Fund Library Database |
| Medline In-Process and Other Citations [OVID] |
Agency for Healthcare Research and Quality National Guideline Clearing House |
| Embase [OVID] |
The Joanna Briggs Institute Library |
| ASSIA [ProQuest] |
|
| Cochrane Library [Wiley] including CDSR, DARE, CENTRAL, NHS EED, HTA Database |
|
| CINAHL [EBSCO] |
|
| PsycINFO[ProQuest] |
|
| Science Citation Index and Social Science Citation Index [Web of Science] |
|
Table 1 Databases and other web resources used in the systematic review.
Data extraction and quality assessment
Two reviewers (AG/RJ) simultaneously extracted the following core data from the included studies: aims and objectives, research methods, participant characteristics, intervention, evidence sources and use in decision-making and approaches and techniques to evidence use and uptake. Other relevant data were extracted, such as any stated theoretical underpinnings or mechanisms of action. During this process provisional categories emerged from the data and were iteratively ‘sense checked’ with the review team. This enabled us to begin to develop a conceptual framework that would bring the studies together in a meaningful narrative [25]. Studies were quality appraised using the Critical Appraisal Skills Programme (CASP) tool for qualitative, quantitative studies and systematic review [26]. The risk of bias was considered across all studies, and results were examined for missing data within individual studies.
Methods of analysis
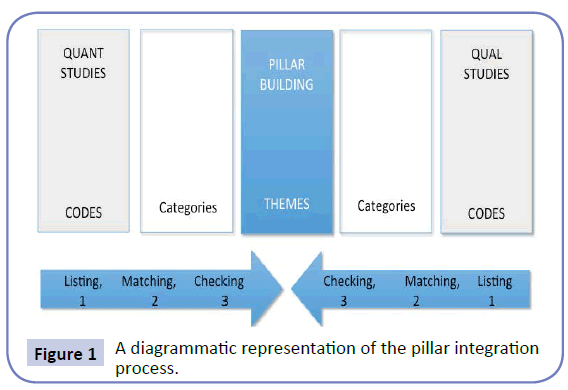
Analysis was undertaken using interpretative mixed methods synthesis and using thematic analysis and narrative synthesis [27]. The initial analysis involved familiarization and immersion in the data, and comparison between the included studies. We used the Pillar Integration Process (PIP) to incorporate both qualitative and quantitative data in a meaningful, yet transparent way [28]. PIP enabled the articles to be drawn together systematically whilst also providing an independent view of the current stateof- the-art and cumulative knowledge on the subject [29-31].
Studies were integrated using a convergence coding matrix and synthesised narratively. The first three stages of PIP (the listing, matching and checking) were followed to construct the foundations of the PIP coding matrix as displayed in Figure 1. Subsequently, we completed the more creative fourth ‘Pillar Building’ stage. Using thematic analysis we coded the data from all papers to develop new constructs by identifying related concepts in the studies. We then summarised the findings of different studies under thematic category headings, reworking and reformulating them together into the central ‘pillar’. Using the emergent categories and conceptual framework, a narrative synthesis was developed to examine relevant themes, identifying patterns and anomalies across the studies.
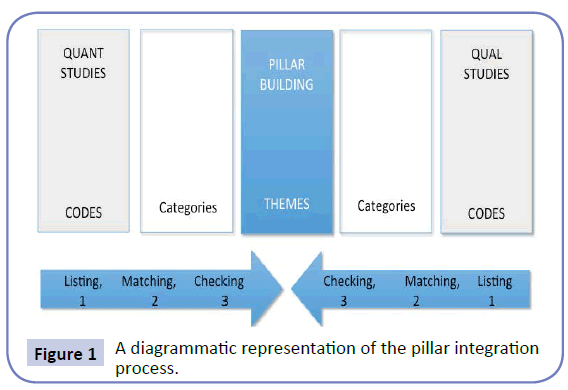
Figure 1: A diagrammatic representation of the pillar integration process.
Results
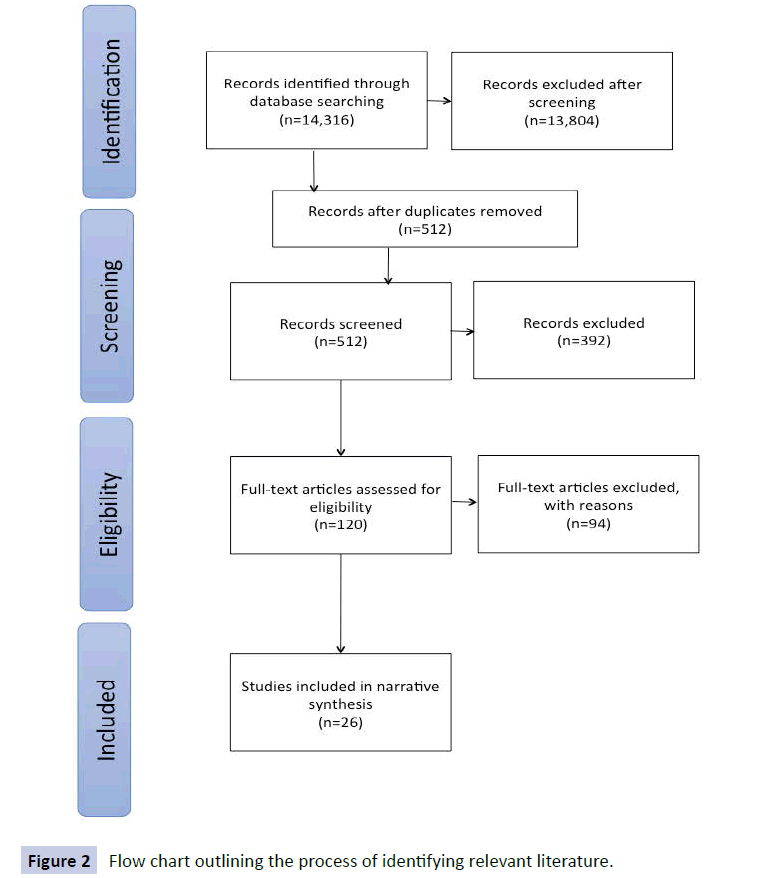
The flow chart outlining the process of identifying relevant literature can be found in Figure 2 [31]. A total of 14,316 articles were found of which 13,804 did not meet the inclusion criteria and were removed. Title and abstract screening removed a further 392 studies, leaving 120 articles to be investigated. Full texts of these studies were examined for inclusion by two reviewers (AG/ RJ). Disagreements were resolved by consensus or third party review. Ninety-four studies were excluded with reasons resulting in 26 final articles (24 primary studies, 2 systematic reviews). Included studies were heterogeneous in methods used and phenomena studied. Hence, meta-analysis of quantitative data was not considered useful.
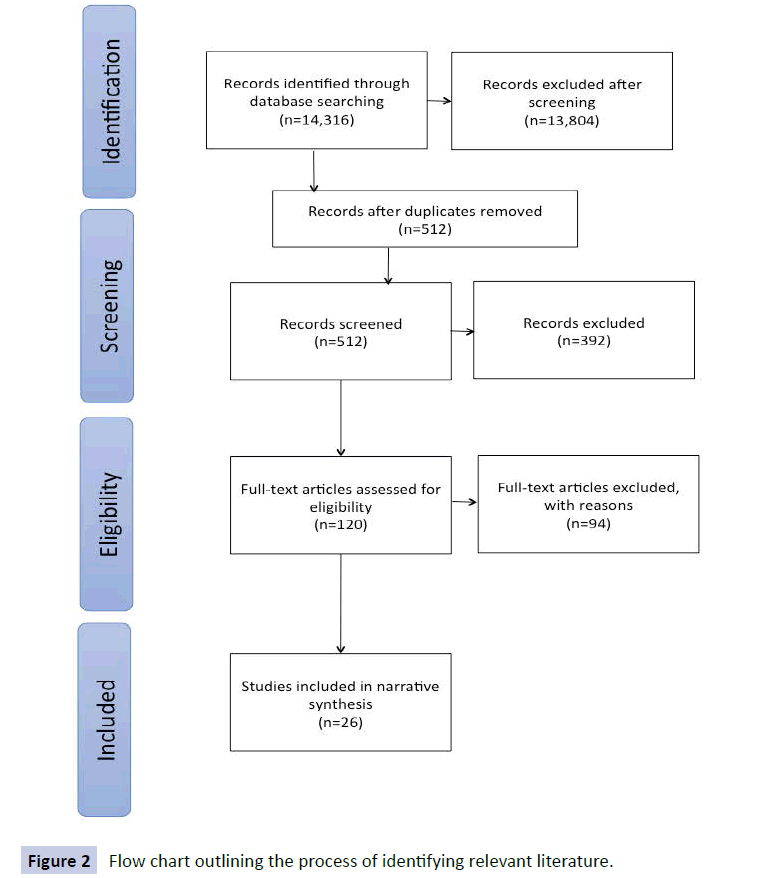
Figure 2: Flow chart outlining the process Figure 2 of identifying relevant literature.
Characteristics of the studies selected
The primary aim of many of the included studies was to identify the influence of a factor or variety of factors on a particular aspect of surgical practice or treatment decision. Studies varied in the factors they assessed over a range of orthopaedic procedures including hip and knee arthroplasty, hip fracture, upper extremity and spine surgery, anterior cruciate ligament surgery and the use of associated procedures such as blood transfusion and drainage, steroid injects and physical therapy.
Summary of primary study evidence
Twenty-four primary studies were included, the majority were quantitative (n=20) the remainder were qualitative (n=4). We brought together the studies systematically using summary tables presented in Supplementary file S2. A summary of SPIDER and PICO characteristics is provided in Supplementary file S3 to order the evidence and produce a description of study characteristics. A large number of the studies reported cross-sectional survey data (n=16). Other study designs included: prospective (n=3), retrospective (n=3) and qualitative studies (n=4) including: interviews (n=2) focus groups (n=1) observation (n=1) and a case study (n=1).
Summary of systematic review evidence
Two systematic review studies were included in the review. These were undertaken by Barr et al. and Bederman et al. [32,33]. The first addressed the drivers of transfusion decision-making in orthopaedic surgery and the second aimed to discover the decision-making drivers for degenerative hip, knee and spine surgery.
Pillar Integration Process
The initial stages of PIP resulted in the identification of 44 prominent codes in the included 26 studies. The PIP central pillar integration process resulted in eight themes (Table 2).
QUANT STUDIES
CITATION |
FACTOR(S)/SOURCES OF EVIDENCE |
PILLAR
THEMES |
FACTOR(S)/SOURCES OF EVIDENCE |
QUAL STUDIES
CITATION |
deBoeret al. (2012),[34] Watts et al. (2005),[35] Zielinski et al. (2013)[36]
Marx et al. (2003),[37] Khan et al. (2013),[38] Krahnet al. (2006)[39]
Marx et al. (2003),[37] Kumar et al. (2010)[40]
Schulz et al. (2013)[41]
Tejawaniet al. (2008)[42]
Cantyet al. (2013),[43] Khan et al. (2013),[38] Tejiwaniet al. (2008)[42] |
Practice guidelines are present More agreement when there is more evidence, use evidence when it exists Poor dissemination of evidence, difficult to access EBM Independent peer reviewed papers Literature (formal) Believe it is evidence based medicine, Belief in RCTs |
Formal codified knowledge |
|
|
deBoeret al. (2012)[34]
Hageman et al. (2013)[44]
Kegalet al. (2013)[45]
Lingardet al. (2000)[46]
Okikeet al. (2014)[47] |
Treatment is too expensive Treatment is cheapest Price of the medication and availability Belief costs and availability of extended care facilities Cost knowledge associated with use of implants |
Managerial knowledge |
|
|
deBoeret al. (2012)[34]
deBoeret al. (2012)[34]
deBoeret al. (2012)[34]
Krahnet al. (2006),[39] deBoeret al. (2012)[34]
Lingardet al. 2000[46]
Lingardet al. (2000),[46] Hageman et al. (2013)[49]
Wright et al. (1999)[48] |
Lack of equipment or facilities Rota limited actions Support staff unable to do what is required Time (pressure) Waiting times/lists Funding status of hospital, reimbursement or surgeons
Organisational status association to a medical school |
Organisational knowledge |
Constraints of the healthcare system/institutional constraints such as available operating theatres
Extensive waiting lists
Suitable doesn’t guarantee surgery unfair/discriminate/best rather than the most appropriate
Prioritisation of patients everyone who needs one is not going to get one
Link with teaching hospital is important in getting evidence into practice
Availability of resources (imagining) |
Hudaket al. (2008)[49] Hudaket al. (2008)[49] Hudaket al. (2008)[49] Hudaket al. (2008)[49] Ferlieet al. (1999)[8] Bedermanet al. (2012)[33] |
deBoeret al. (2012)[34]
Hageman et al. (2013)[44]
Hageman et al. (2013)[44]
Hageman et al. (2013)[44], Kegalet al. (2013)[45]
Kumar et al. (2011)[40] Schulz et al. (2013)[41] Vashitzet al. (2002)[50] |
Supervisor prevented use What my mentor taught me Burns fewer bridges with colleagues What others are doing, what colleagues use More likely to discuss with colleagues Meetings with colleagues and conferences Influenced by opinion of others and previous opinions |
Socialisation and association with colleagues |
Clinician plays a role/clinicians as the experts/assigned and adopted
Roles Relationship building between surgeon and patient/negotiating
relationships with other professionals/maintaining professional networks
/maintain position in the organisation/maintain peer network/social and cultural Change in opinion is fast, decision making and opinion was volatile Not trust the RCTs from outside their group/always find a paper to
support your idea, ortho journals most powerful position Indirect channels of information transfer Decisions made locally/negotiated/a core group of professionals have
legitimacy and are believed Influential actors work is more likely to be believed The orthopaedic community is important/professional community with distinct norms (resilient/embedded/retain control)/internal community/group knowledge |
Gooberman-Hill et al. (2010)[51] Hudaket al. (2010)[49] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] |
Watts et al. (2005)[35]
Watts et al. (2005)[35]
Schulz et al. (2013)[41] |
Medico-legal concerns Uniformity in the region in which surgeon practices Pharmaceutical companies, implant manufactures |
Cultural, normative and political influence norms of the sector |
High level of group and individual autonomy over work, Highly professionalised form of clinical work Orthopaedics is different/ separate/autonomous, Pharmaceutical companies Orthopaedics are actors not reflectors, personality characteristics are distinct/certain people Medico-legal concerns Authority figure/judgment/control of specialists/experts Supply and demand/gaming the system/having a strategy Lack of homecare/post operative support/judgment based on aftercare support Playing the middle man/medical broker |
Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Gooberman-Hill et al. (2010)[51] Hudaket al. (2010)[49] Hudaket al. (2010)[49] |
Cantyet al. (2013)[43]
deBoeret al. (2012)[34]
Irwin et al. (2005)[52]
Kumar et al. (2011)[40]
Kumar et al. (2011)[40]
Schulz et al. (2013)[41]
Tejawaniet al. (2008)[42]
Kegalet al. (2013)[45] |
Learned in practice Did not learn it Different training background Academic qualifications in EBM Formal training in EBM Training course Gained during traditional training Educated, learned in fellowship |
Training and formal education |
|
|
Cantyet al. (2008)[43]
Cantyet al. (2008),[43] Dusiket al. (2013)[53]
Wright et al. (1999)[48]
Wright et al. (1999)[45]
Tejiwaniet al. (2008)[42]
Kumar et al. (2010)[40]
|
Personal reasons Don’t believe in evidence (based) Surgeons opinions about treatment Surgeons enthusiasm for procedure Personal experience gained in practice
Believe it is difficult to adhere to EBM |
Informal experiential Implicit knowledge |
Surgeons appraisal of the patients complexity, various explicit factors play a part in the judgment including lifestyle and clinical influences Skills come from experience and instinct Surgeons style of approach to patient, surgeons confidence in their own ability/more confident more likely to perform surgery/enthusiasm Personality characteristics/ paternalistic diplomatic conservative assertive/styles influence behaviour Belief who is able and better, not who is in need Implicit definition of patient candidacy/definitions are rarely
explicit/not knowing the rules of the game Patient prioritisation influences behaviour Highly professionalised form of clinical work, disagree with science/different views/skeptical about formal science Controversy in treatment options/not trust the RCTs from outside their group/always find a paper to support your idea, orthopaedic journals most powerful position The individual consultant on the inside is more important than external source of evidence Orthopaedics is a learnt craft/tacit and experiential more important Patients in research do not match the real patients in practice Practice is learnt slowly, it does not transfer across groups easily Surgeon believes surgery ‘Works in my hands’ Individual learning ad reflection is favoured over EBM/experience |
Gooberman-Hill et al. (2010)[51] Gooberman-Hill et al. (2010)[51] Gooberman-Hill et al. (2010), [51]Bedermanet al. (2012)[33] Gooberman-Hill et al. (2010)[51] Hudaket al. (2008),[49] Bedermanet al. (2012)[33] Hudaket al. (2008)[49] Hudaket al. (2008)[49] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] |
Bhandariet al. (2005),[54] Irwin et al. (2005),[42] Wright et al. (1999),[48] Zielinski et al. (2013)[36]
Bhandariet al. (2005),[54] Curtis et al. (2011),[55] Watts et al. (2005),[35] Cantyet al. (2003)[43]
Bhandariet al. (2005),[54] Curtis et al. (2011)[55]
Borkhoffet al. (2008)[56]
Cantyet al. (2013),[43] Dusiket al. (2013),[53] Kegalet al. (2013),[45] Zielinski et al. (2013)[36]
Cantyet al. (2013),[43] Hageman et al. (2013)[44]
Curtis et al. (2011),[55] Cantyet al. (2008),[43] Dusiket al. (2013),[53] Irwin et al. (2005)[52]
deBoeret al. (2012)[34] Dusiket al. (2013),[53] Hageman et al. (2013),[44] Kegalet al. (2013)[45]
Irwin et al. (2005),[52] Marx et al.
(2003),[37]
Marx et al. (2003)[37]
Borkhoffet al. (2008)[56] |
Patients age Patients medical condition Patient lifestyle factors, social circumstance Patients sex Clinical treatment and medication Practical or pragmatic reason, shorter procedure Symptoms, pain Need to have patient with the problem Years in practice, level of experience Surgeons age Surgical volume Surgeons sex |
Individual Patients and surgeon factors |
Clinical factors most important/symptom severity/pain/stiffness Patient lifestyle factors/social/work context, family support/
Post-operative support Pragmatic reasons Personality characteristics are distinct/certain people Patients age Patients medical condition Patients sex Surgical volume Patients weight Surgeons sex Patients insurance coverage |
Gooberman-Hill et al. (2010),[51] Barr et al. (2011),[32] Bedermanet al. (2012)[33] Gooberman-Hill et al. (2010)[51] Ferlieet al. (1999)[8] Ferlieet al. (1999)[8] Barr et al. (2011),[32] Bedermanet al. (2012)[33] Barr et al. (2011)[32] Barr et al. (2011),[32] Borkhoffet al. (2008)[56] Barr et al. (2011)[32] Barr et al. (2011)[32] Bedermanet al. (2012)[33] Bedermanet al. (2012)[33] |
Table 2 Pillar integration process convergence coding matrix.
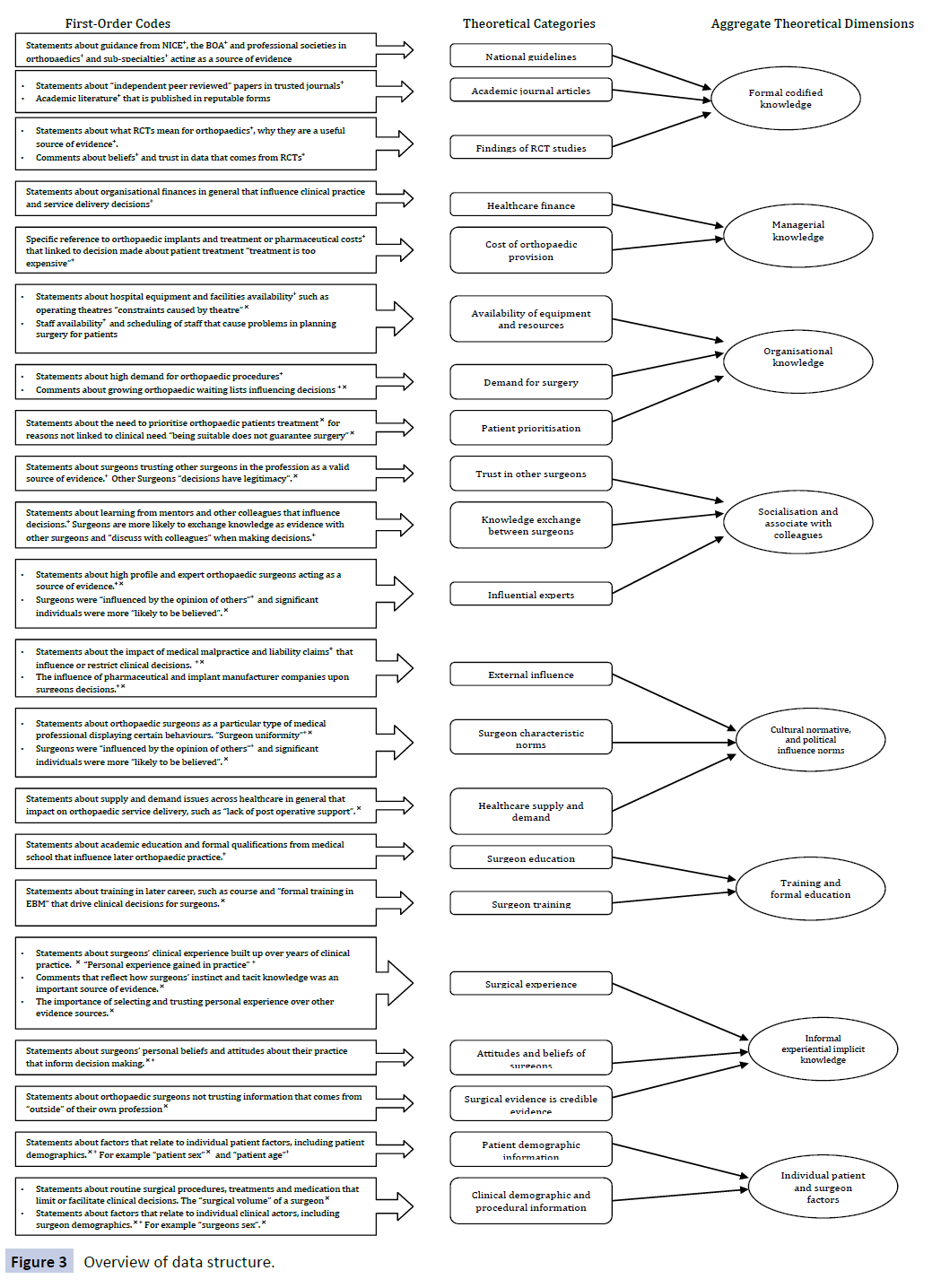
An overview diagram of the data structure is presented in Figure 3. Displaying the data structure in this way is recommended by Pratt et al. 2006, 2009 [34,35] Pratt argues that the challenge of qualitative and quantitative research is that there are no accepted “boilerplate” for writing up methods and determining quality [35] and objectivity. The boilerplate refers to a standardised language and format for presenting research findings, and this is not something qualitative and mixed methods researchers strive to achieve. This equifinality can make it extremely problematic to portray qualitative and qualitative research [35]. However, presenting the data using an overview diagram as in Figure 3, enables us to honor the worldview of the articles that were included in the review, provide sufficient evidence for claims made, and allows us to contributes to extant theory through the conclusions made [35].
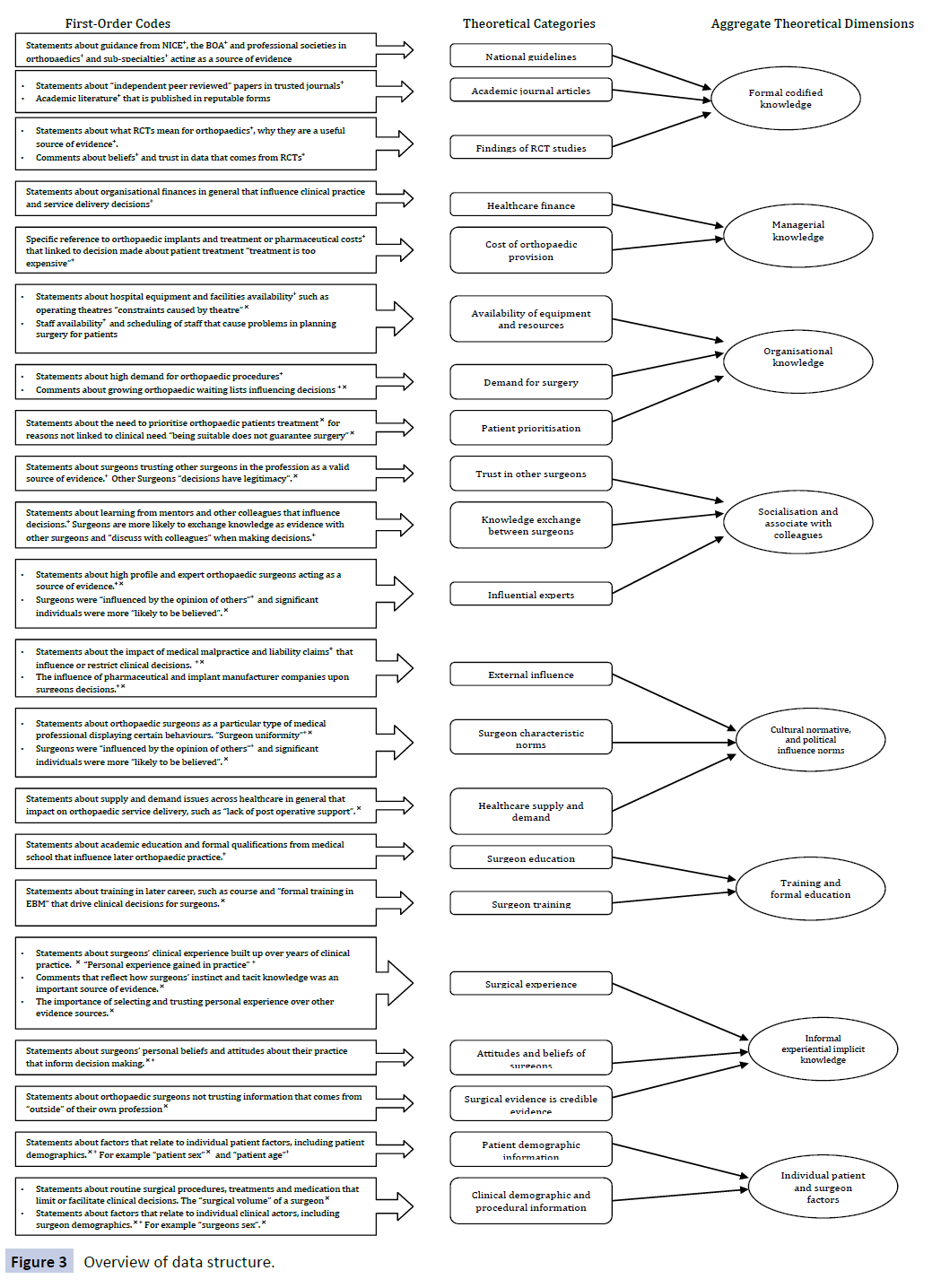
Figure 3: Overview of data structure.
Discussion
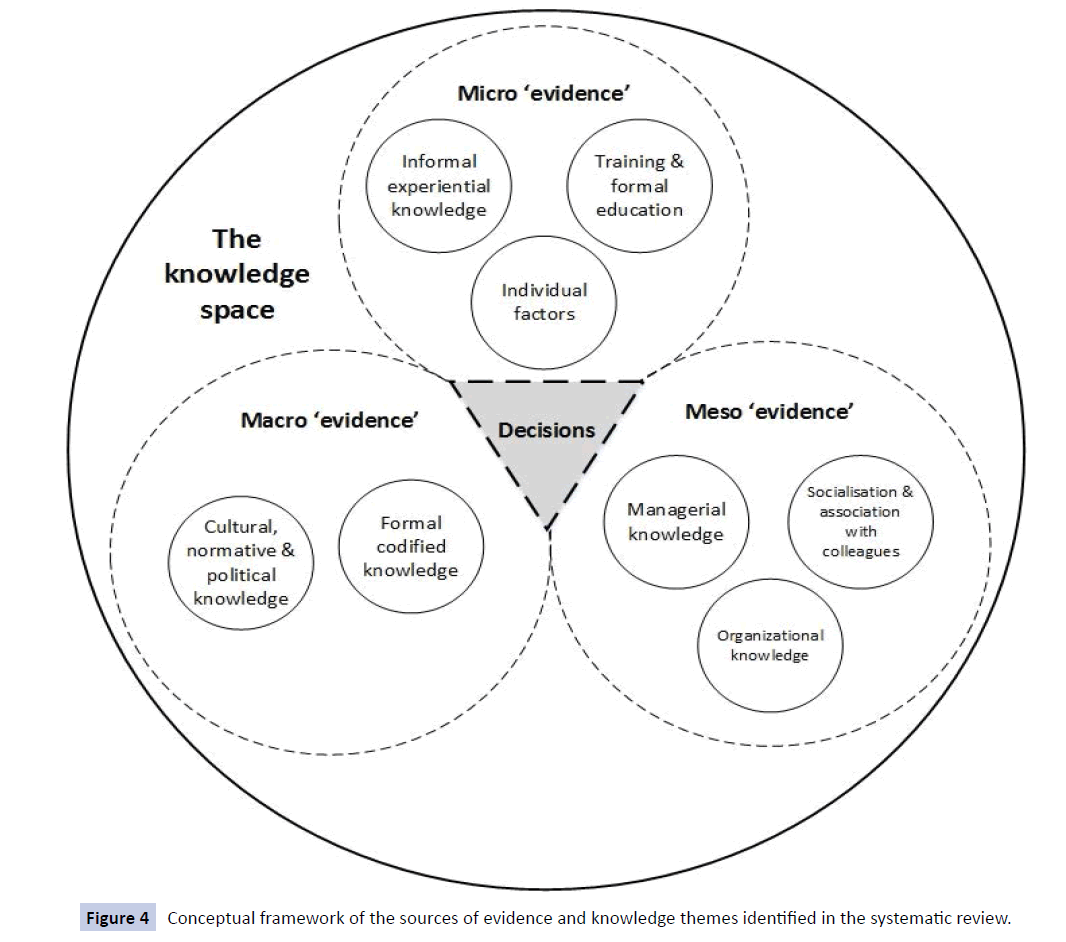
The review identified sources of evidence, or the knowledge types reported as important for orthopaedic decision-making. These sources are influential in determining patient treatment and help to explain how and why there is unwarranted variation in orthopaedic surgical practice. Factors were identified and categorised into eight themes which reflect the micro-level patient and clinical drivers; and meso factors such as characteristics of the organisation or surgeon through to the impact of formal training. At the macro-level we identified the influence of evidence, policy and guidelines. Each theme is described below and a conceptual model is presented which demonstrates the relationship between these sources of evidence and knowledge types.
Formal codified knowledge
Formal codified knowledge is explicit, written down and thus available to everyone to use alongside personal judgment [34]. In our review, formal codified knowledge represents the macro-level clinical guidelines and scientific literature to which orthopaedic surgeons can (and are expected to) refer when making evidencebased decisions. This knowledge is hard, factual, spelt out and easy to transfer between individuals. Hence the assumption is to ‘policy makers is that’ standardised knowledge in guidelines can be disseminated across clinical populations.
Formal codified knowledge was reported to influence decisionmaking in ten of the 26 studies. It included reference to guidelines [36-38], evidence-based medicine [39-44] and independent peer reviewed literature [43,45]. The included studies reported a low influence of this type of knowledge. This low influence is in contrast to what would be expected by the advocates of evidence-based medicine and the significance attached to the hierarchy of evidence in the clinical field.
Managerial knowledge
Managerial knowledge represents an important component of clinical decision-making within orthopedics as it can underpin the routines and capabilities of practice – i.e., the scope of work conducted. In this area, the literature often referred to resource issues such as time, cost and safety or quality of services but without definite or consistent criteria of what is considered acceptable. For example, a “treatment is too expensive” was considered a factor that influences clinical decisions but without providing a context within which to benchmark the concept of ‘expensive’ [36]. Managerial knowledge is subjective and experiential and is often not written down for healthcare staff to access. This makes it difficult to transfer between and across organisational, departmental and also across professional boundaries within the same organisation [35].
In the six studies which mention managerial knowledge, cost [36,46-51] and availability of resources [47,48] were most influential in clinical decision-making. The knowledge and skills of individuals who manage healthcare organisations were considered valuable but intangible in the organisations. This led to uncertainly, for example treatment costs influenced decisions when both expensive options [36] and cheaper treatment options were available [44]. Surgeons’ knowledge of treatment and orthopaedic implant costs was also associated with their use in practice but the definition of acceptable cost was not explicit [49]. The weight assigned to managerial knowledge in orthopaedics is increasingly important due to the rising demand for treatment, and reinforced by pressures to reduce resource use.
Organisational knowledge
Organisational knowledge has a wider structural emphasis. It is anecdotally referred to as “the way we do things around here” as it shapes the perspectives of clinicians working in an organisation. It is embedded in the processes of healthcare organisations and influences the behavior of its members. Organisational processes become normative and reflect the common education, training and career structures of particular organisations [50]. This type of knowledge is ingrained in the routines of the orthopaedic departments and hospitals but not necessarily acknowledged by the individuals themselves [47].
Organisational constraints such as theatre availability, surgical waiting lists and patient prioritisation acted as forms of organisational knowledge in the included studies [8,47,51]. Variation in the practice of patient categorisation or treatment delay resulted from organisational knowledge that does not diffuse but becomes sticky within the organisation. One paper stated “prioritisation of patients means that everyone who needs one is not going to get one” [51]. Time pressures and staffing influenced clinical decisions when planning surgery [36,41]. These organisational factors develop over time and become entrenched, so that knowledge exists in the processes and clinical pathways themselves not in the individual actors. The likelihood of finding a common ground for collaboration and knowledge sharing within but not across orthopaedic departments to reduce variation in the healthcare organisations is limited.
Socialisation and association with colleagues
The socialisation of individuals into different clinical professions plays an important role in their decision-making processes. Orthopaedic surgery represents a highly professionalised area of clinical work as a specialty where an elite community of practice is strongly embedded [8,9]. This community has socialised knowledge that impacts on the way decisions are made by its members. The knowledge is treated as a vital source of evidence which is held in the group but not shared with outsiders. Nine papers reported socialised knowledge influenced decisions. Examples include “what my mentor taught me”, restrictions placed on practice by supervisors [31,43] “what my colleagues are doing”[46,47,51] and the notion that “decisions made locally and negotiated by a core group of professionals have legitimacy and are believed” [8,51-53].
There was a distinction between knowledge that came from inside or outside the defined group, in this case the orthopaedic community [8,52]. Surgeons reportedly did not “trust the RCTs from outside their group” [38] and were more influenced by work that came from “influential actors” in the field [8] Particularly important were knowledge and evidence gained at local professional meetings and conferences [42,43] Decisions are said to be driven by socialised knowledge because orthopaedic communities share common values, language, procedures and know-how, and hence act as a source of learning and practice for each other.
Culture, norms and political influence of the sector
This theme demonstrates how the wider orthopaedic profession can influence clinical practice and drive decision-making for patients. For example, the presence of professional societies, such as the British Orthopaedic Association in the UK and the American Academy of Orthopaedic Surgeons in the USA, enabled the members to retain substantial autonomy, authority and control over their work practices and to resist external intervention [8,51,53]. This external intervention might be in the form of clinical guidelines and regulation which are codified evidence produced outside the orthopaedic sector. The use of this type of evidence in decision-making was likely to be complex and fraught with political challenges. It was to a certain extent linked to how surgeons maintained their elite position in the wider clinical field by privileging their normative professional knowledge over clinical guidelines that can be accessed by anyone [51,54]. Therefore, it can influence decisions at all levels: the micro individual surgeon deciding to operate or not, the meso communities of practice who plan and allocate intervention thresholds, and the macro professional groups who build consensus statements and establish orthopaedic criteria.
Medico-legal challenges to practice drove patterns of a- to decision-making to minimise legal action in two papers [8,35]. The power of pharmaceutical and implant manufacturing companies within this sector was also highlighted [8]. As was the “struggle to balance supply and demand” of services [49] and beliefs about how allied health professions can or cannot contribute to service delivery [51,55]. In one study, a decision for surgery depended on the surgeons subjective view of “appropriate post-operative support” [50] Attitudes towards the ability and or use of non surgeon professionals varied [53]. This could be associated with incentives to maintain professional control and power over clinical decisions. The process of prioritising, negotiating and juggling these factors during decision-making was referred to as “medical brokering” and defined as “a procedural strategy used by physicians when demands in a system are perceived to exceed resources” in one paper [51].
Training and formal education
It would be expected that a surgeons’ training and formal education might have an impact upon how they make decisions for patients. Seven papers reported that some form of training influenced surgeons’ clinical decisions [36,42-45,47,54]. The training and formal education theme covered the standard “academic qualifications” [40] such as medical training but also the apprenticeship style training gained through fellowship programmes and practice-based learning [45,51,54]. Training courses undertaken later in surgical practice were considered more important to surgeons [43]. This is maybe because these reflect the subspecialist training that the surgeons were most attracted to. Formal training in evidence-based medicine was reported its to increase its use in clinical decisions, and the perceived importance of evidence to practice [42]. Training and formal education becomes an important foundation which can be built on over time using elements from all other knowledge types.
Informal experiential knowledge
This represents the tacit knowledge that surgeons ‘know’ which has built up over time but which can be difficult to describe. This type of knowledge is treated as one of the most important sources of evidence in decision-making in orthopaedic practice because it represents a surgeon’s lifetime’s work, and in turn their identity as a surgeon. When considering the tacit – explicit knowledge spectrum, informal experiential knowledge sits in opposition to formal codified knowledge. It cannot easily be explained, transferred and understood by another person, particularly someone outside the orthopaedic community. Individual knowledge gained from their experience does not exist in the activity alone, but in the knowledge that individuals use to perform the activity [56]. Hence, a surgeon possesses tacit knowledge of how to perform an operation when they are outside of theatre.
The included studies reported several examples of informal experiential knowledge which drive decisions [8,51,53]. Reference to surgeon’s judgment, skill, craft, experience and instinct were all reported as important [8,51,53]. As were confidence, style and approach to patients’ after treatment alongside beliefs about patients in general [55]. For example surgeons had a “belief in who is able and better (for surgery) not who is in need”[49] which contrasts with the concept of clinical need or a patients’ requirement for surgery which might be expected when applying the principles of evidence-based guidelines.
Individual patients and surgeons factors
The final theme clusters all factors that were directly related to the characteristics of the patient or surgeon that influenced clinical practice decisions in the included studies. Surgeons with a greater surgical volume in joint replacement would be more inclined to conduct a joint replacement compared to non-surgical management. Patient factors included age, [38,41,51,56] medical condition, [36,45,35,56] sex, [33,56] lifestyle, [51,54,55] treatment options, medication and symptoms [39,43,49,51,53,55]. Surgeon factors included age, [39,54] sex, [33] personality type [8] and surgical volume [39]. Some pragmatic factors were also important, such as time taken to perform surgery where certain procedures were selected because they were shorter than other options [8,45,46].
What does this mean for orthopaedic practice?
We have identified many sources of evidence which compete for space and prominence in the process of decision-making. The competition may be subconscious as medical professionals may broker various evidence sources and knowledge types within current organisational contingencies. This element of tacit practice came through strongly in many of the included studies [8,51-58] and has been recognised elsewhere in the medical literature [14,63].
It is important that surgeons and orthopaedic departments develop an awareness of this subjective and subconscious brokering process. It is essential in clinical practice to enable surgeons to be cognizant of who and what is influencing their clinical decisions and the contingencies and constraints they are working within. Once the drivers of decisions are apparent to the decision-makers, it will be possible to adjust, improve or eliminate factors which can be considered inappropriate and which may lead to unfair or inappropriate and unwarranted variation in practice. Across the literature each of these drivers, can be considered a viable source of evidence or knowledge for surgeons, on a par with formal codified clinical guidelines, and our review demonstrates that they influence clinical practice decisions [59-62].
Our findings highlight the power of local clinical communities, networks and hierarchies within the orthopaedic profession. They result in decision-making that is grounded in “that’s what we do around here” evidence, rather than the evidence-based medicine which is of proven effectiveness for patients. Utilising these strong clinical networks for positive knowledge sharing may be an avenue for future investigation particularly relevant for this clinical group. We have found from this review that although clinical evidence, such as patients’ functional score, is important and necessary for decision-making they are not sufficient to drive a clinical decision. Other sources of evidence for example, current waiting lists and operating room availability (organisational knowledge) or the necessity to maintain good relationships with colleagues and superiors (socialised knowledge) can take precedence. The different ways in which sources of evidence and knowledge are brokered and privileged in practice result in the variation in delivery of orthopaedic services and in potentially unsatisfactory outcomes for patients.
Conceptual framework of themes
We have not set out to present the eight themes hierarchically, as the ways they interact depend on the contingencies of the current context. This may change over time for individuals and organisations as and when the different evidences come into focus. Instead we propose a conceptual framework (Figure 4) structured around the wider definition of an evidence-based decision to describe how the different evidence and knowledge sources can act as micro, meso or macro drivers of variation in orthopaedic surgical work.
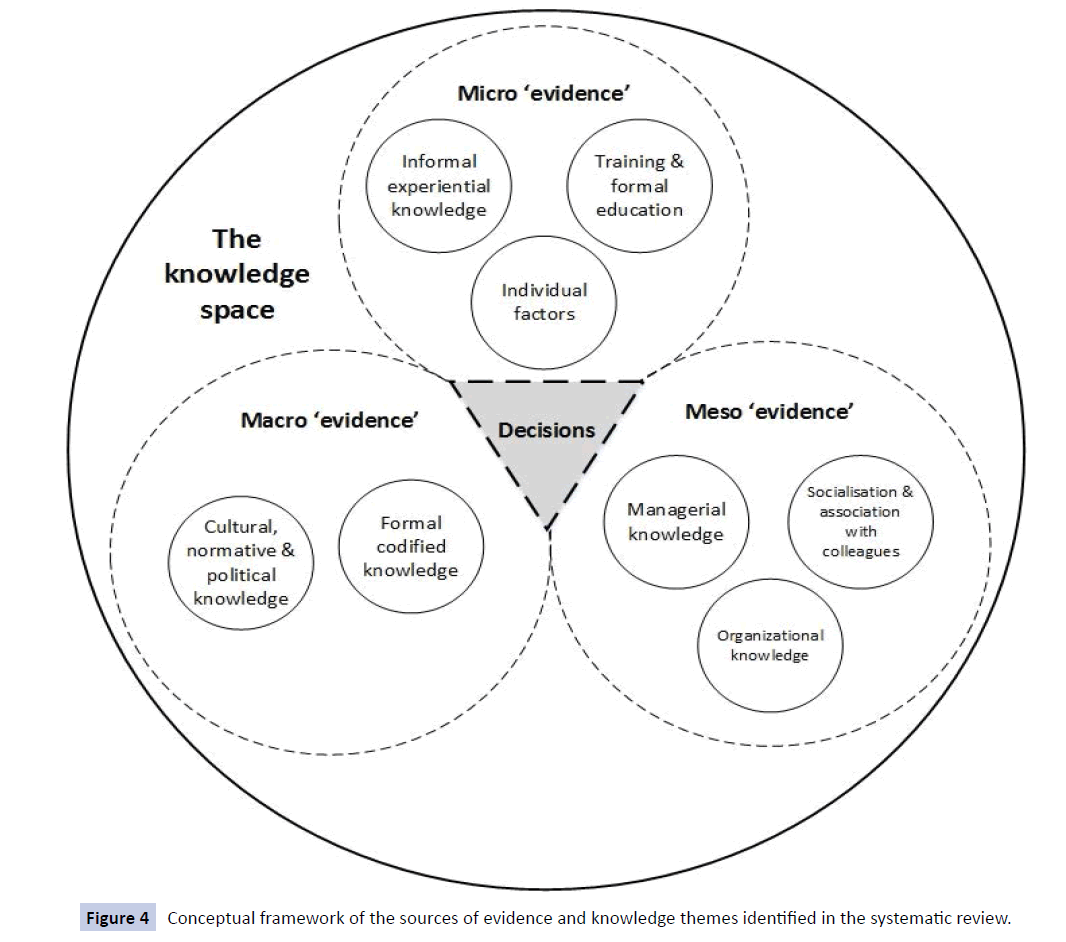
Figure 4: Conceptual framework of the sources of evidence and knowledge themes Figure 4 identified in the systematic review.
The next step is to test this conceptual framework in practice and to understand its applicability to modern healthcare organisations, we need to understand whether there are situations in which the alignment and hence importance of the different themes change. Each source of evidence has strengths and weaknesses and contributes to variation in orthopaedic practice depending on who is making the decision and in what circumstance. Decisions made from a financial stance may not lead to effective outcomes for a patient on the ward, and hence are reported to carry less weight for the individual surgeon [49,63-65]. However, when examining the level of organisational practice (clinical commissioning) or national policy (clinical and cost-effectiveness analysis) financial decisions play a central role in decision-making. What is important here is how evidence is combined in the real life pragmatic process of decision-making, where decisions are complex and challenging.
Conclusion
We systematically reviewed and summarised published literature on the approaches and techniques towards evidence use, and the factors that influence to evidence-based decision-making and practice within orthopaedic surgery. Data were integrated using the Pillar Integration Process and analysed thematically to produce eight themes which can be treated as the sources of evidence that influence the decisions of orthopaedic surgeons. These factors may be explicit, or may act outside conscious decision-making processes. They are brokered directly or indirectly in competition with each other.
In this review we have found that formal codified knowledge, e.g., clinical guidelines produced by NICE and other national bodies, appears to play a small part in orthopaedic decision-making. More significant drivers of variation include the socialisation of medical professionals, the cultural and normative factors at play and the existence of complex and competing sources of knowledge.
Patient candidacy does not in itself account for the reported variation in the delivery of orthopaedic services. Individual surgeons, their clinical communities and wider professional societies coupled with the constraints and contingencies of healthcare systems influence and complicate the decisionmaking process. As a result, the factors feeding into decisions, contribute to the widespread variability in surgical practice. Services are not as high quality; cost-effective and equitable as they could be which means that “not everyone who needs one is going to get one”. Until the process of decision-making is fully explored, and strategies are developed to mitigate against this incongruous evidence use, interventions, policies and recommendations aimed at achieving equitable, clinical and costeffective orthopaedic decisions will be limited in their reach and effectiveness.
Funding
Amy Grove is supported by the National Institute for Health Research (NIHR) Doctoral Research Fellowship Programme grant number DRF-2013-06-064. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Rebecca Johnson, Aileen Clarke and Graeme Currie are supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care West Midlands at University Hospitals Birmingham NHS Foundation Trust.
Acknowledgements
The authors would like to acknowledge Samantha Johnson and Rachel Court, Information Specialists at the University of Warwick who assisted in the development of the search strategies used in this review.
Competing Interests
All authors declare that we have no competing interests. All authors have completed the ICMJE uniform disclosure form and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Data Sharing
No additional data available.
Ethical Approval
No ethical approval was sought for this systematic review.
8815
References
- Briggs T (2015) Getting It Right First Time (GRIFT). British Orthopaedic Association.
- Judge A, Welton NJ, Sandhu J, Ben-Shlomo Y (2010) Equity in access to total joint replacement of the hip and knee in England: cross sectional study. BMJ 341: c4092.
- Amick HR, Gartlehner G, Gaynes BN, Forneris C, Asher GN , et al. (2015) Comparative benefits and harms of second generation antidepressants and cognitive behavioral therapies in initial treatment of major depressive disorder: systematic review and meta-analysis. BMJ 351: h6019.
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS (1996) Evidence based medicine: what it is and what it isn't. BMJ 312: 71-72.
- Kelly M, Morgan A, Ellis S, Younger T, Huntley J, et al. (2010) Evidence based public health: A review of the experience of the National Institute of Health and Clinical Excellence (NICE) of developing public health guidance in England. SocSci Med 71: 1056-1062.
- Glover JA (1938) The Incidence of Tonsillectomy in School Children: (Section of Epidemiology and State Medicine). Proc R Soc Med 31: 1219-1236.
- Ferlie E, Wood M, Fitzgerald L (1999) Some limits to evidence-based medicine: a case study from elective orthopaedics. Qual Health Care 8: 99-107.
- Ferlie E, Fitzgerald L, Wood M, Hawkins, C et al. (2005) The nonspread of innovations: the mediating role of professionals. AcadManag J 48:117-134.
- Wennberg J, Gittelsohn (1973) Small area variations in health care delivery. Science 182: 1102-1108.
- Wennberg JE (2002) Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ 325: 961-964.
- Mulley A, Wennberg J (2011) Reducing unwarranted variation in clinical practice by supporting clinicians and patients in decision making. Chp 3. In Gigerenzer G, Gray MJA eds. Better Doctors, Better Patients, Detter Decisions: EnvisioiningHelath Care 2020. MA: Massachusetts Institute of Technology.
- Moritz S, Bates T, Henderson SM, Humphreys S, Michell MJ (1997) Variation in management of small invasive breast cancers detected on screening in the former south east Thames region: observational study. BMJ 315: 1266-1272.
- Pope C. Contingency in everyday surgical work. Sociology of Health & Illness 2002:24:369-384.
- Birkmeyer JD, Sharp SM, Finlayson SR, Fisher ES, Wennberg JE (1998) Variation profiles of common surgical procedures. Surgery 124: 917-923.
- Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, et al. (2005) Variation in orthopaedic surgeons' perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am 87: 1978-1984.
- McPherson K (2008) Reprints and reflections: The incidence of tonsillectomy in school children. IntEpidemiol Ass 37: 9-19.
- South East Public Health Observatory, Atlas of Variation (2010) NHS Atlas of variation
- Appleby J (2010) Which English hospital is best at hips? The Kings Fund.
- Appleby J, Devlin N (2010) Getting the most out of PROMS. Putting health outcomes at the heart of NHS decision-making. The Kings Fund.
- Higgins JPT, Green S (eds). (2001) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration.
- Chalmers I, Glasziou P (2009) Avoidable waste in the production and reporting of research evidence. Lancet 374: 86-89.
- Booth A, Papaioanno D, Sutton A (2012) Systematic Approaches to a Successful Literature Review. UK:Sage Publications Limited.
- Gough D, Thomas J, Oliver S (2012) Clarifying differences between review designs and methods. Syst Rev 1: 28.
- CASP (2015) Critical Appraisal Skills Programme. Critical appraisal tools.
- Dixon-Woods M, Agarwal S, Young B, Jones D, Sutton A (2004) Integrative approaches to qualitative and quantitative evidence. London: NHS Health Development Agency.
- Johnson J, Grove A, Clarke A (2015) Pillar Integration Process: A technique to mix methods in the health sciences. JMMR
- Britten N, Campbell R, Pope C, Donovan J, Morgan M, et al. (2002) Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy 7: 209-215.
- Campbell R, Pound P, Morgan M, Daker-White G, Britten N, et al. (2011) Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess 15: 1-164.
- Moher D, Liberati A, Tetzlaff J, Altman DG (2009) The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 151: 264-269.
- Barr PJ, Donnelly M, Cardwell C, Alam SS, Morris K, et al. (2011) Drivers of transfusion decision making and quality of the evidence in orthopedic surgery: a systematic review of the literature. Transfus Med Rev 25: 304-316.
- Bederman SS, Rosen CD, Bhatia NN, Kiester PD, Gupta R (2012) Drivers of surgery for the degenerative hip, knee, and spine: a systematic review. ClinOrthopRelat Res 470: 1090-1105.
- Pratt MG, Rockmann KW, Kaurmann JB (2006) Constructing professional identity: the role of work and identity learning cycles in the customization of identity among residents. Academy of Management Journal 49: 235-262.
- Pratt MG (2009) For the lack of a boilerplate: tips on writing up (and reviewing) qualitative research. Academy of Management Journal 52: 865-862.
- de Boer PG, Buckley R, Schmidt P, Fox B (2012) Barriers to orthopaedic practice--why surgeons do not put into practice what they have learned in educational events. Injury 43: 290-294.
- Watts AC, Brenkel IJ (2005) A postal survey of current thromboprophylactic practices of consultant orthopaedic surgeons in the treatment of fracture of the hip. J Bone Joint Surg Br 87: 296-300.
- Zielinski SM, Meeuwis MA, Heetveld MJ, Verhofstad MH, Roukema GR, et al. (2013) Adherence to a femoral neck fracture treatment guideline. IntOrthop 37: 1327-1334.
- Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF (2003) Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy 19: 762-770.
- Khan H, Hussain N, Bhandari M (2013) The influence of large clinical trials in orthopedic trauma: do they change practice? J Orthop Trauma 27: e268-274.
- Krahn J, Sauerland S, Rixen D, Gregor S, Bouillon B, et al. (2006) Applying evidence-based surgery in daily clinical routine: a feasibility study. Arch Orthop Trauma Surg 126: 88-92.
- Kumar M, Gopalakrishna C, Swaminath PV, Mysore SS (2011) Evidence-based surgery--evidence from survey and citation analysis in orthopaedic surgery. Ann R CollSurgEngl 93: 133-138.
- Schulz AP, Jönsson A, Kasch R, Prithee J, Bhandari M (2013) Sources of information influencing decision-making in orthopaedic surgery-an international online survey of 1147 orthopaedic surgeons. BMC MusculoskeletDisord 14: 96.
- Tejwani NC, Immerman I (2008) Myths and legends in orthopaedic practice: are we all guilty? ClinOrthopRelat Res 466: 2861-2872.
- Canty SJ, Shepard GJ, Ryan WG, Banks AJ (2003) Do we practice evidence based medicine with regard to drain usage in knee arthroplasty? Results of a questionnaire of BASK members. Knee 10: 385-387.
- Hageman MG, Guitton TG, Ring D, Science of Variation Group (2013) How surgeons make decisions when the evidence is inconclusive. J Hand Surg Am 38: 1202-1208.
- Kegel G, Marshall A, Catalano L, Barron OA, Glickel SZ, et al. (2013) Steroid injections in the upper extremity: experienced clinical opinion versus evidence-based practices. Orthopedics 36: e1141.
- Lingard EA, Berven S, Katz JN, Kinemax Outcomes Group (2000) Management and care of patients undergoing total knee arthroplasty: variations across different health care settings. Arthritis Care Res 13: 129-136.
- Okike K, O'Toole RV, Pollak AN, Bishop JA, McAndrew CM, et al. (2014) Survey finds few orthopedic surgeons know the costs of the devices they implant. Health Aff (Millwood) 33: 103-109.
- Wright JG, Hawker GA, Bombardier C, Croxford R, Dittus RS, et al. (1999) Physician enthusiasm as an explanation for area variation in the utilization of knee replacement surgery. Med Care 37: 946-956.
- Hudak PL, Grassau P, Glazier RH, Hawker G, Kreder H, et al. (2008) "Not everyone who needs one is going to get one'': the influence of medical brokering on patient candidacy for total joint arthroplasty. Med Decis Making 28: 773-780.
- Vashitz G, Pliskin JS, Parmet Y, Kosashvili Y, Ifergane G, et al. (2012) Do first opinions affect second opinions? J Gen Intern Med 27: 1265-1271.
- Gooberman-Hill R, Sansom A, Sanders CM, Dieppe PA, Horwood J, et al. (2010) Unstated factors in orthopaedic decision-making: a qualitative study. BMC MusculoskeletDisord 11: 213.
- Irwin ZN, Hilibrand A, Gustavel M, McLain R, Shaffer W, et al. (2005) Variation in surgical decision making for degenerative spinal disorders. Part I: lumbar spine. Spine 30: 2208-2213.
- Dusik CJ, Buckley RE, Robertson-More C (2013) Orthopedic surgeon perspectives on appropriate referral of trauma patients to physical therapy (PT). Arch Orthop Trauma Surg 133: 603-608.
- Bhandari M, Devereaux PJ, Swiontkowski MF, Schemitsch EH, Shankardass K, et al. (2003) A randomized trial of opinion leader endorsement in a survey of orthopaedic surgeons: effect on primary response rates. Int J Epidemiol 32: 634-636.
- Curtis AJ, Wolfe R, Russell CO, Elliott BG, Hart JA, et al. (2011) Determining priority for joint replacement: comparing the views of orthopaedic surgeons and other professionals. Med J Aust 195: 699-702.
- Borkhoff CM, Hawker GA, Kreder HJ, Glazier RH, Mahomed NN, et al. (2008) The effect of patients' sex on physicians' recommendations for total knee arthroplasty. CMAJ 178: 681-687.
- Tsoukas H, Vladimirou E (2005) ‘What is organizational knowledge?. Managing Knowledge: An Essential Reader pp: 85.
- Currie G, Suhomlinova O (2006) The impact of institutional forces upon knowledge sharing in the UK NHS: the triumph of professional power and the inconsistency of policy. Public Administration 84:1-30.
- Roberts A (2015) Very Short, Fairly Interesting and Reasonably Cheap Book About Knowledge Management. UK:Sage Publications.
- Grove A, Clarke A, Currie G (2015) The barriers and facilitators to the implementation of clinical guidance in elective orthopaedic surgery: a qualitative study protocol. Implement Sci 10: 81.
- Lave J, Wenger E (1991) Situated learning: Legitimate peripheral participation. Cambrige Cambridge University Press.
- Polanyi M (2012) Personal knowledge: Towards a post-critical philosophy. Chicago: University of Chicago Press.
- Gabbay J, le May A (2004) Evidence based guidelines or collectively constructed "mindlines?" Ethnographic study of knowledge management in primary care. BMJ 329: 1013.