Mini Review - (2022) Volume 14, Issue 4
Evidence-based approach to fever and fever of unknown origin in Fiji
Abhijit Gogoi*,
Judith Apondi Oremo,
Ivor Xavier Tsika,
ElisonJimmy,
Alphones Kuma,
Muhammed Ilyas Harun and
Mercy Gogoi
Umanand Prasad School of Medicine and Health Sciences, The University of Fiji, Saweni, Lautoka, Fiji
*Correspondence:
Abhijit Gogoi, Umanand Prasad School of Medicine and Health Sciences, The University of Fiji, Saweni, Lautoka,
Fiji,
Email:
Received: 25-Mar-2022, Manuscript No. ipaom-22-12523;
Editor assigned: 28-Mar-2022, Pre QC No. P-12523;
Reviewed: 17-Mar-2022, QC No. Q-12523;
Revised: 22-Mar-2022, Manuscript No. R-12523;
Published:
27-Apr-2022
Abstract
While Fiji a South Pacific Country is an archipelago of more than
300 islands. With an approximate population of 889, 953, Fiji
faces a growing burden of several communicable diseases and
non-communicable disease including fever of unknown origin.
Surveillance data suggest that Fever has become increasingly
common in rural areas of Fiji and is more frequent amongst acute
respiratory infections, dengue and viral infections. Appropriate
measures are taken by the Ministry of Health Fiji to reduce the
potential for relapse and reinfection in clinical cases, by encouraging
proper hand hygiene of food and drink handlers, water and
sanitation agencies to review current sanitation practices and
vaccination policy targeting epidemiologically relevant populations.
This article initial aim is to examine fever of unknown origin around
the Pacific and Fiji but due to limited data available we mainly
focus on cases of diseases that have at least fever as one of the
associated symptoms in 2018 within the four divisions of Fiji namely
the Northern Central, Eastern and Western regions. A retrospective
study with data obtained from the Fiji Ministry of Health 2018 and
National Notifiable Disease Surveillance System Weekly Bulletin.
Acute respiratory infection is the leading cause of FUO and fever
in Fiji with an average of 64% cases in 2018 followed by Dengue at
14%. Patient in significant numbers continue to present fever/FUO
due to a wide range of diseases. Future prospective data collection
is recommended to identify the cause and trends, which inform the
Ministry of Health and future research priorities hence allowing
the development of appropriate policies and clinical guidelines for
management of fever/FUO.
Keywords
Antibiotic; Fiji; Pacific; Dengue Fever ; Fever of Unknown
Origin (FUO) ; Pyrexia of Unknown Origin (PUO) ;Viral infections
(Viral illness infection); Acute Respiratory Infection (ARI)
Introduction
Fevers of unknown origin still remain one of the most
difficult diagnostic challenges in medicine. While
technology such as F-fluorodeoxyglucose positron emission
tomography (FDG-PET) [1] exists, clinicians often have to
ordernon-clue based imaging and specific testing early in
FUO work up. Fever of unknown origin may be caused by
over 200 malignant/neoplastic, infectious [1]. rheumatic/
inflammatory, and miscellaneous disorders, therefore test
ordered may be inefficient/misleading. Neurons in both the
preoptic anterior and posterior hypothalamus receive two
kinds of signals to control the human body temperature.
One signal from the peripheral nerves transmit information
from warmth or cold receptors in the skin and the other
transmit signal from temperature of the blood bathing
the region. These two are integrated by thermoregulatory
center of the hypothalamus to maintain the normal
temperature [2]. Normal human body temperature ranges
between 36.5°C to 37.5°C. Other sites of the body have
the following normal temperature, mouth 36.8°C, axilla
35.4°C, rectum 37.7°C and ear 36.8°C [3-5]. Fever, also
known as pyrexia is defined as an elevation of the human
body temperature that exceeds the normal daily variation
(35.5°C-37.5°C) and occurs in conjunction with an increase
in the hypothalamic set point, that is 37°C to 39°C. Fever
is caused by infections either bacterial [6]. viral or fungal
that affects the ears, lungs, throat, skin bladder or kidney.
Other causes of fever include heat exhaustion, sunburn,
conditions that causes inflammation such as rheumatoid
arthritis, adverse drug reactions of medications, vaccination
and immunizations, blood clots, autoimmune disorders,
hormone disorders and illegal drug use. Classified in two
ways, acute or chronic fever and continuous, intermittent,
remittent or relapsing fever. Acute fever occurs in less than
7 days and is characteristics of infectious diseases such as
malaria and viral-related upper respiratory tract infection.
Chronic or persistent fevers is fever that occurs and lasts
for more than or equal to two weeks’ duration and are
typical of chronic bacterial infections such as tuberculosis,
viral infections such as HIV, cancers and connective tissue
diseases. However, any cause of acute fever can become
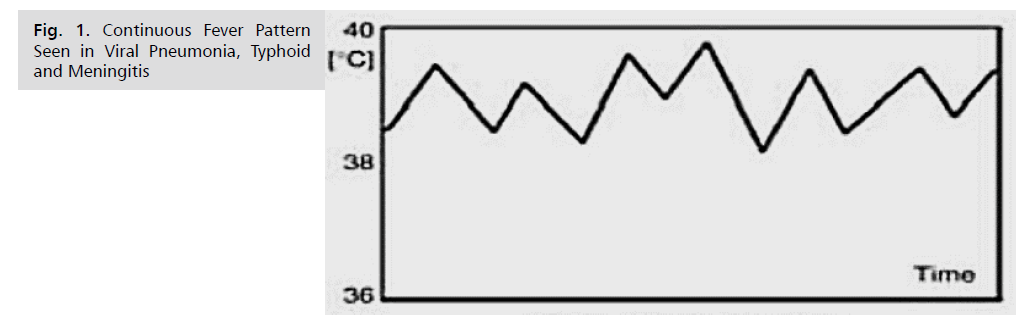
persistent [6] or chronic if untreated. Continuous fever or
sustained fever (Fig. 1-4) is defined as fever that does not
fluctuate more than about 1°C during 24 hours, but at no
time touches normal and are characteristic features of lobar
and gram-negative pneumonia, typhoid, acute bacterial
meningitis, urinary tract infections, among others [7,8].
Pyrexia of Unknown Origin (PUO)also known as fever of
unknown origin ( FUO) was first defined by Petersdof in 1961 but over the year was refinedto any fever greater than
or equals to 38.3°C several occasion with the duration of
more than three weeks the least with no known diagnosis
after many laboratory tests despite one week of inpatient investigations or three outpatient visits [9]. Infections
account for approximately 25 to 30% of cases usually the
most likely cause of FUO [10,1] followed by neoplasm
and noninfectious inflammatory [11]. FUO can also be classified to intonosocomial, neutropenic, classic, and
Human Immunodeficiency Virus (HIV)-associated FUO
[12]. PUO mortality is low, antipyretics or antimicrobials
therapy early on may delay diagnosis hence treatment
before diagnosis not suggested [13]. In 2011, Fiji, had a
concern over the rapid rise in reported cases of typhoid
fever, leptospirosis along dengue fever locally known as
the “three plagues” [6]. The three plagues are common
etiologies of fever of unknown origin in Fiji. Other causes
of FUO in Fiji includes dengue, rheumatic fever, measles, hepatitis, mumps, acute respiratory infections (ARI), TB,
meningitis, viral illness Infections among others.
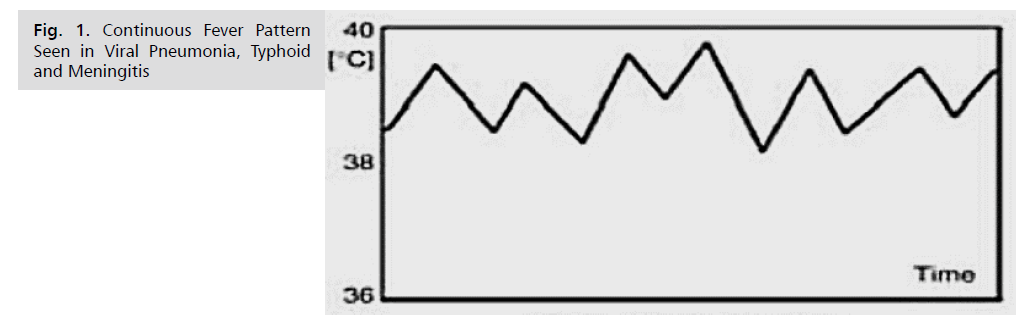
Figure 1: Continuous Fever Pattern Seen in Viral Pneumonia, Typhoid and Meningitis.
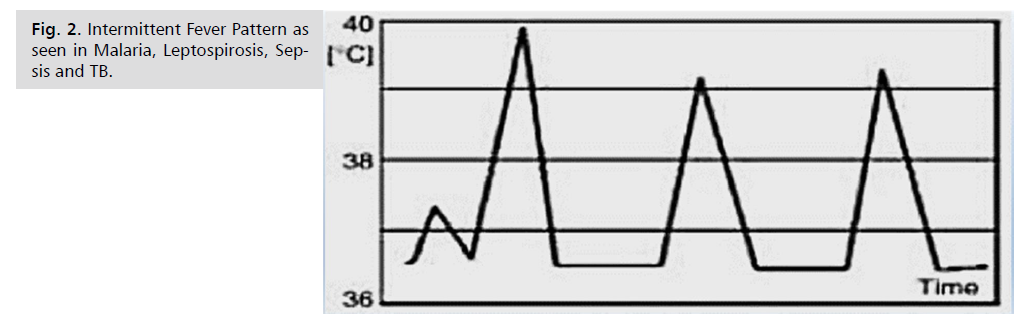
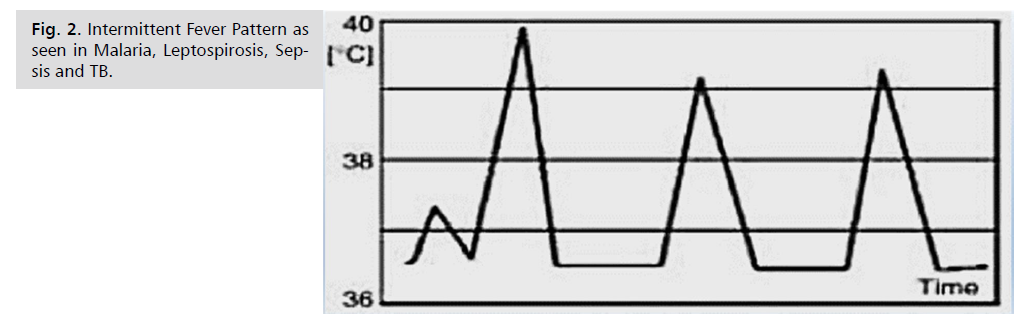
Figure 2: Intermittent Fever Pattern as seen in Malaria, Leptospirosis, Sepsis and TB.
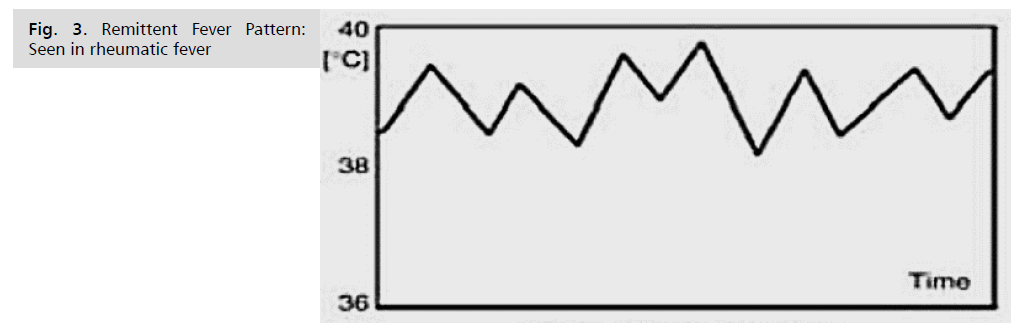
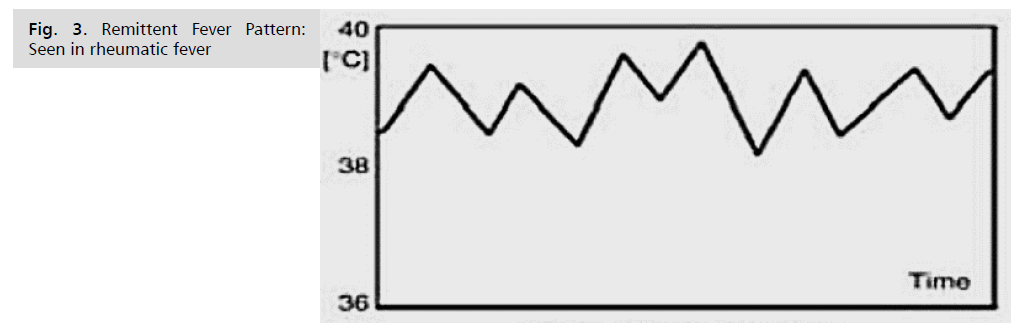
Figure 3: Remittent Fever Pattern: Seen in rheumatic fever.
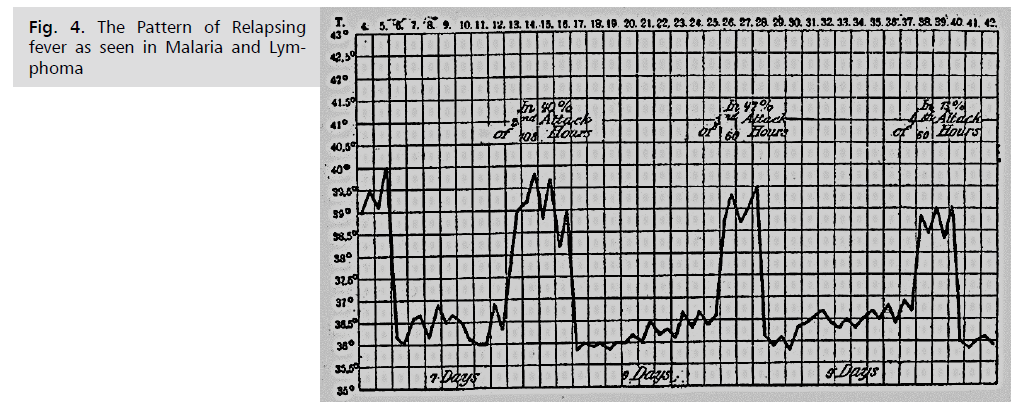
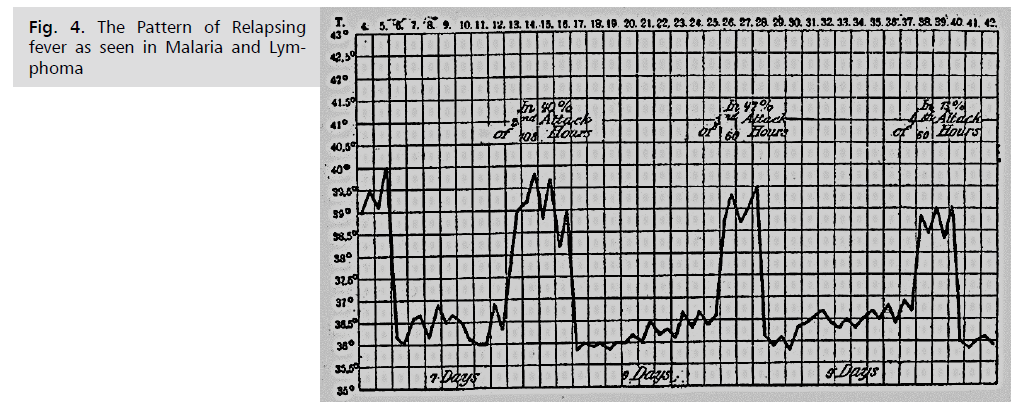
Figure 4: The Pattern of Relapsing fever as seen in Malaria and Lymphoma.
Methodology
Several research on FUO studies since the early
19th century to date has led to understanding and clinical
implementation. This research is a retrospective study,with
focus on available data on FUO and Fever caused by
infection, using this criterion was more effective because most data on Fever and FUO in Fiji is due to infection,
all age groups were included due to the elderly being
susceptible to infection compared to young persons [14].
Data collected also included HIV and this was guided
by a study that proved opportunistic infection and HIV
can cause FUO, patient under HAART may have FUO
at a smaller percentage compared to those not receiving
HAART [15] and in Japan, HIV was the commonest cause
of FUO due to increase in HIV patients [16]. Sources
of information of this research were taken from online
sources and reference textbooks and the main source of
information data regarding diseases relating to FUO and
fever were taken from the Ministry of Health, National
Notifiable Disease Surveillance System Weekly Bulletin
2018 [17-22]. All data were tabulated and charts generated
for data analysis was done using Microsoft Excel software.
Herpes, hepatitis, denguewas tracked separately from other
viral illness because they are of concern and endemic in
Fiji.
Discussion
In this study there are a significant number of cases of
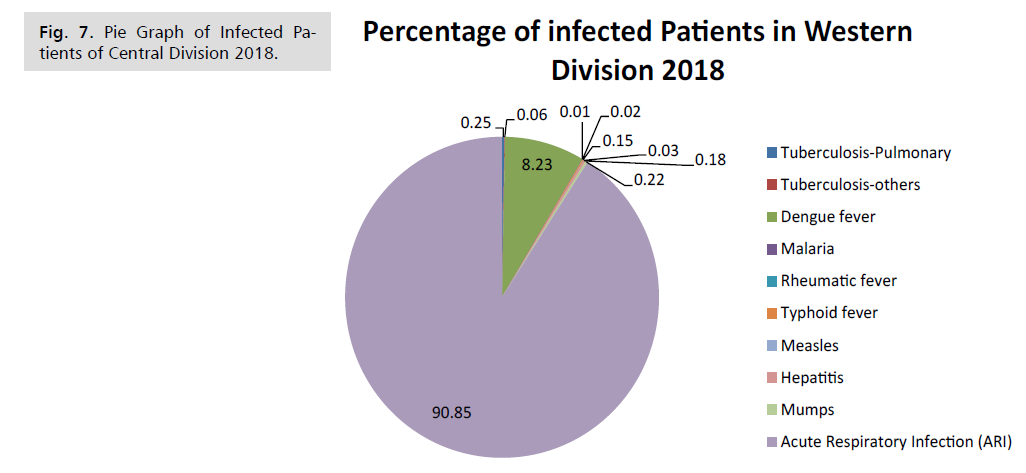
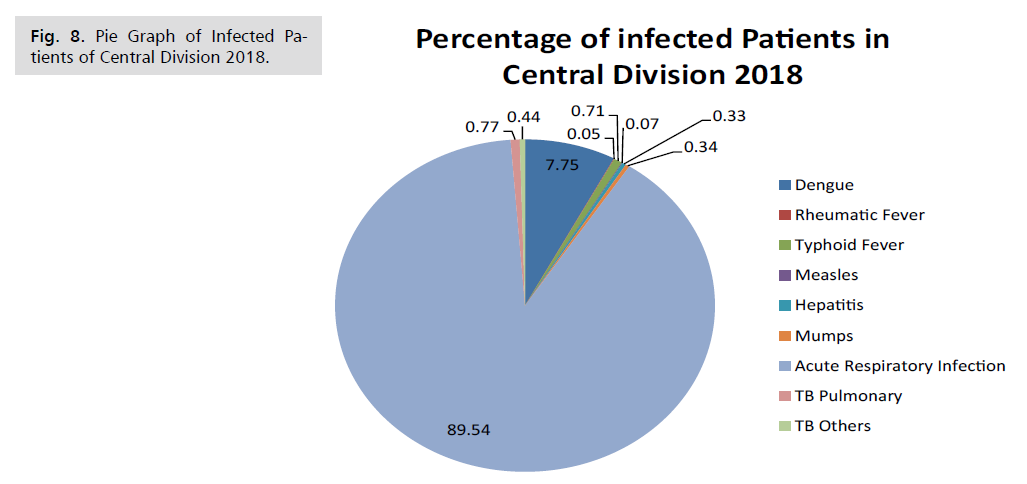
fever and fever of unknown origin in Fiji. The Western and
Central division recorded the highest case of fever/FUO
at 36,985 and 21349 in 2018 respectively this can be due
to several factors as geographic condition and urbanization
and accessible medical facilities. While the Northern
and Eastern division recorded the lowest cases 3762 and
2489 respectively. Acute respiratory infection cases were
the main reason of fever/FUO in Northern, Western and
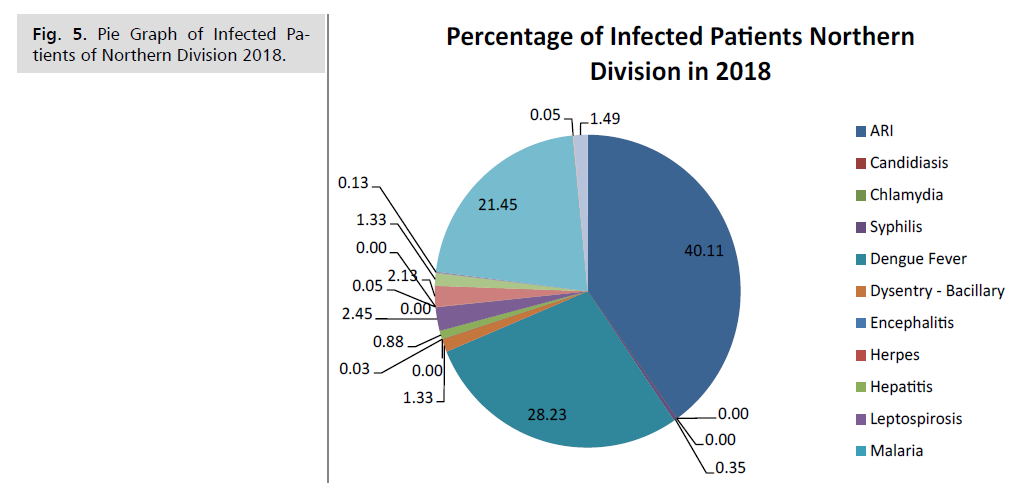
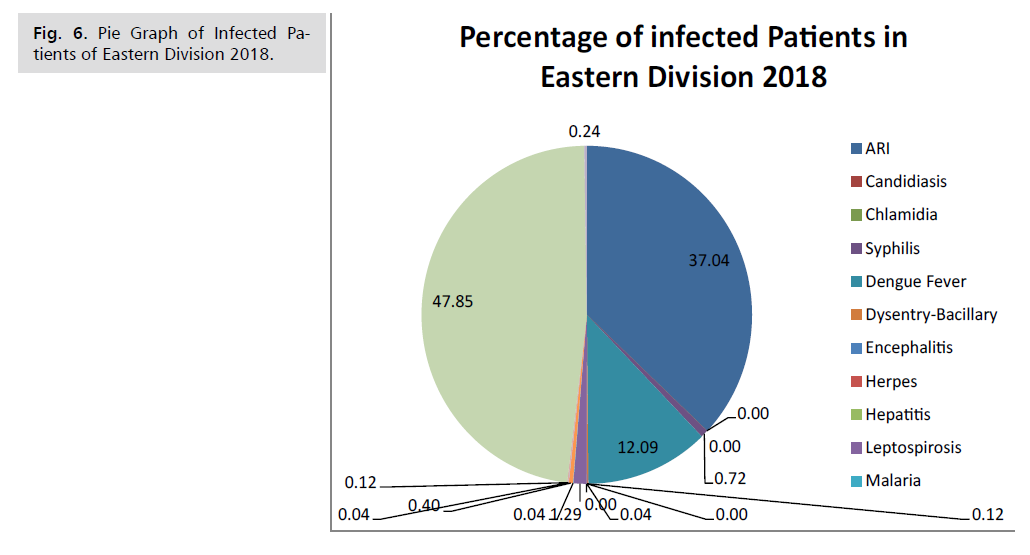
Central division (Fig. 5-8) followed by dengue except in
the Eastern) where the main reason was viral illness, RI and
dengue respectively. Dengue fever has been reported in Fiji
over the years since the 19th century [2] as epidemic, to date there are still cases though controlled through vector
borne clean up campaigns [3]. and public awareness on
prevention. Acute Respiratory Infection can be caused
by a number of pathogen ranging from bacterial, viral
and fungal infection which are more influenced by the
humid climatic condition, living conditions and other
environmental factors such factories in those area. Others
infections such as syphilis, dysentery – Bacillary, herpes,
leptospirosis, amebiasis, meningitis hepatitis, measles,
tuberculosis, rheumatic fever, mtyphoid fever, measles,
hepatitis, mumps causes fever/FUO but this depend on
the location climatic influence. Chlamydia, causes of
FUO/Fever was insignificant in this study and some viral
illness can cause acute respiratory infection. Other fever
cases associated with fever of unknown origin such as TB,
meningitis and typhoid fever were reported but were not
as significant as that of acute respiratory infections and
dengue fever. n ranging from bacterial (Tab. 1-4).
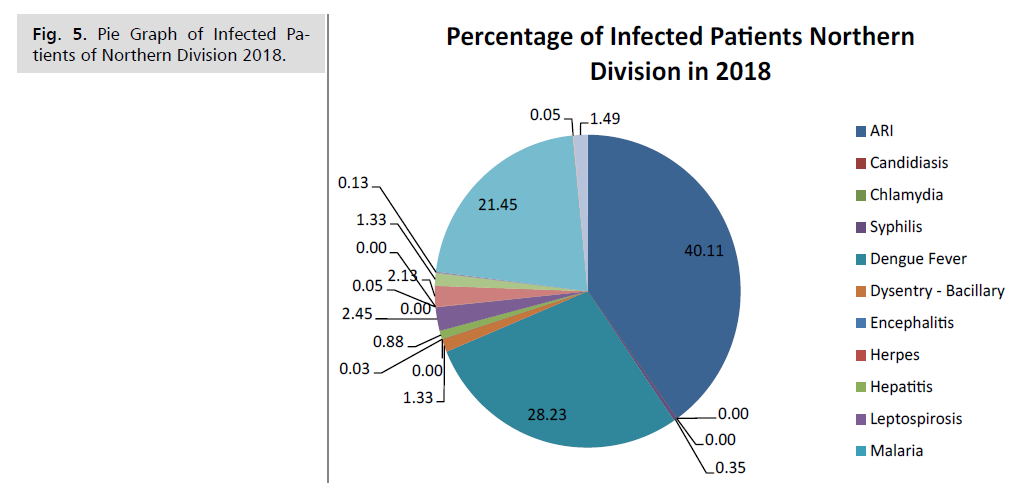
Figure 5: Pie Graph of Infected Patients of Northern Division 2018.
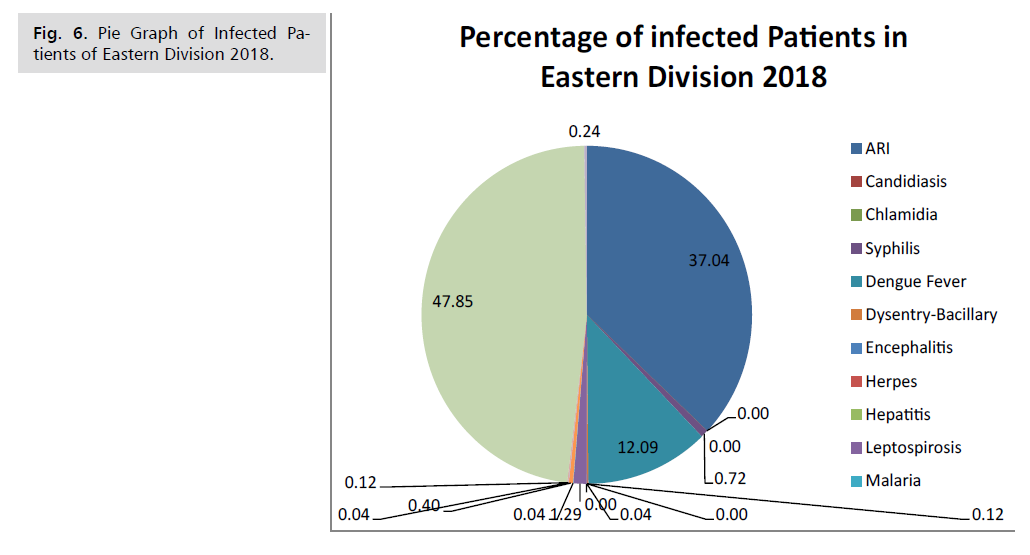
Figure 6: Pie Graph of Infected Patients of Eastern Division 2018.
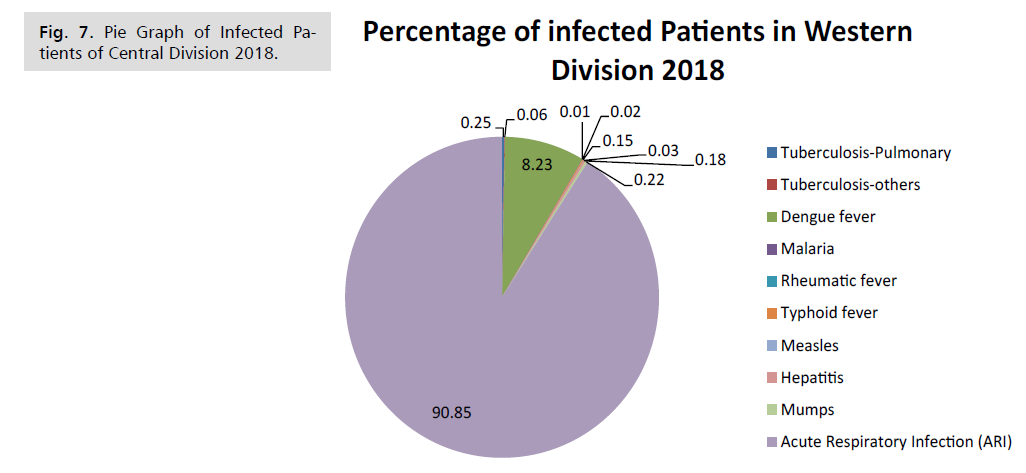
Figure 7: Pie Graph of Infected Patients of Central Division 2018.
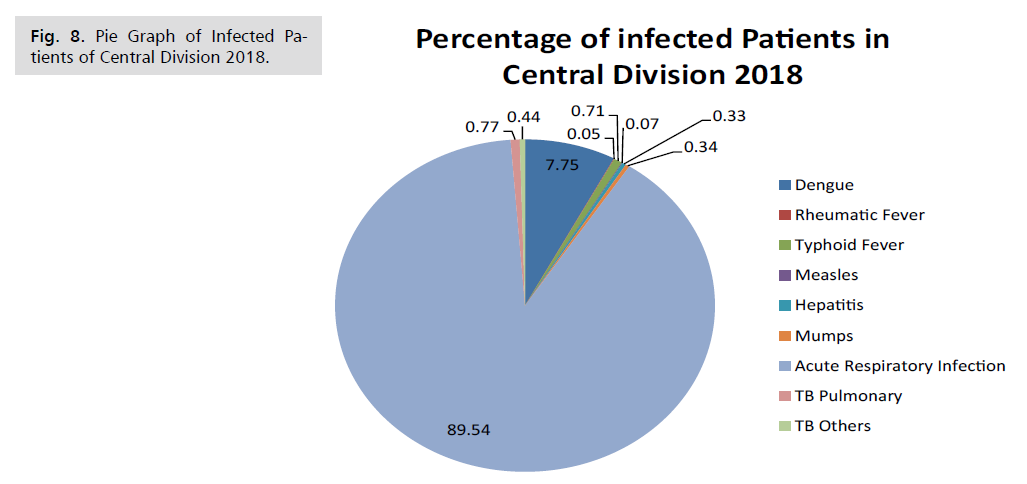
Figure 8: Pie Graph of Infected Patients of Central Division 2018.
| Causes of PUO/Fever |
Number Infected |
Percentage |
| ARI |
1,509 |
40.11 |
| Syphilis |
13 |
0.35 |
| Dengue Fever |
1,062 |
28.23 |
| Dysentery– Bacillary |
50 |
1.33 |
| Herpes |
1 |
0.03 |
| Hepatitis |
33 |
0.88 |
| Leptospirosis |
92 |
2.45 |
| Amebiasis |
2 |
0.05 |
| Typhoid Fever |
80 |
2.13 |
| TB Pulmonary |
50 |
1.33 |
| TB Others |
5 |
0.13 |
| Viral Illness Infection |
807 |
21.45 |
| Rheumatic Fever |
2 |
0.05 |
| Meningitis |
56 |
1.49 |
| Total |
3,762 |
100.00 |
Tab. 1. Shows the total number and percentage of persons infected with different disease causing PUO/fever in the Northern division in the year 2018. ARI having the highest outcome at 40.11% and herpes being the lowest outcome at 0.03%. Other disease such as Chlamydia showed insignificant data.
| Causes PUO |
Number Infected |
Percentage |
| ARI |
922 |
37.04 |
| Syphilis |
18 |
0.72 |
| Dengue Fever |
301 |
12.09 |
| Dysentery-bacillary |
3 |
0.12 |
| Herpes |
1 |
0.04 |
| Leptospirosis |
32 |
1.29 |
| Malaria |
1 |
0.04 |
| Typhoid Fever |
10 |
0.40 |
| TB Pulmonary |
1 |
0.04 |
| TB Others |
3 |
0.12 |
| Viral Illness Infection |
1191 |
47.85 |
| Meningitis |
6 |
0.24 |
| Total |
2489 |
100.00 |
Tab. 2. Shows the total number and percentage of persons infected with different disease causing PUO/fever in the astern division in the year 2018.Viral Illness having the highest outcome at 47.85% and herpes, malaria and pulmonary TB being the lowest outcome at 0.04%. Other diseases such as Chlamydia showed insignificant data.
| Causes of PUO |
Number Infected |
Percentage |
| Tuberculosis-pulmonary |
91 |
0.25 |
| Tuberculosis-others |
24 |
0.06 |
| Dengue fever |
3,044 |
8.23 |
| Malaria |
3 |
0.01 |
| Rheumatic fever |
6 |
0.02 |
| Typhoid fever |
54 |
0.15 |
| Measles |
11 |
0.03 |
| Hepatitis |
68 |
0.18 |
| Mumps |
82 |
0.22 |
| Acute Respiratory Infection (ARI) |
33,602 |
90.85 |
| Total |
36985 |
100.00 |
Tab. 3. Shows the total number and percentage of persons infected with different disease causing PUO/ fever in the Western division in the year 2018. ARI having the highest outcome at 90.85% and malaria being the lowest outcome at 0.01%. Other disease such as Chlamydia showed insignificant data.
| Causes of PUO |
Number Infected |
Percentage |
| Dengue |
1655 |
7.75 |
| Rheumatic Fever |
11 |
0.05 |
| Typhoid Fever |
152 |
0.71 |
| Measles |
14 |
0.07 |
| Hepatitis |
71 |
0.33 |
| Mumps |
72 |
0.34 |
| Acute Respiratory Infection (ARI) |
19115 |
89.54 |
| TB Pulmonary |
165 |
0.77 |
| TB Others |
94 |
0.44 |
| Total |
21349 |
100.00 |
Tab. 4. Shows the total number and percentage of persons infected with different disease causing PUO/ fever in the Central division in the year 2018. ARI having the highest outcome at 89.54% and Rheumatic fever being the lowest outcome at 0.05%. other disease such as Chlamydia showed insignificant data.
Conclusion
The management of PUO should be supportive until
the cause has been determined. Therapeutic trials of
antimicrobials or steroids are not recommended because
they can mask symptoms and signs of the underlying
disease process. The overall mortality of fever of unknown
origin is very low as compared to the rest of the world.
In two situations empirical treatment is appropriate:
antituberculous therapy for suspected miliary or CNS TB
and antimicrobials for patients with suspected infective
endocarditis and signs of sepsis. Empirical treatment for
TB should always be discussed with a specialist, as the risk
of drug resistance needs to be evaluated for each patient,
together with the need for early adjunctive steroid therapy
for CNS and pericardial TB (at differing dosing regimens). In management the best approach is to address the
patient's expectations of diagnosis and treatment. It is very
important to warn the patients about the need methodical
stepwise approach to investigation, which can be sometimes
frustrating for both the patient and physician and as most
of the time it doesn’t lead to a firm diagnosis. Undiagnosed
patients should be reassured that their prognosis is likely
to be good, despite possible continuation of symptoms.
Prospective research can be carried out to give more
specific out of fever and FUO in Fiji, which will contribute
much in research of Fever and FUO and formulation of
specific guideline through the policy makers. A thin line
lies between acute respiratory infection and viral illness
infection.
Conflicts of Interest
All authors declare that they have no conflict of interest.
Data Availability
The data used for the research is available on request
email juditho@unifiji.ac.fj
Funding
No funding although research was performed as part of
the employment at Umanand Prasad School of Medicine
and Health Sciences, The University of Fiji.
Acknowledgments
We thank the Fiji Ministry of Health and Medical
Service for approval, support and for providing access to
historical health records, and to UPSM&HS staff for their
support and technical assistance
REFERENCES
- Beović B, Doušak M, Ferreira-Coimbra J, et al. Antibiotic use in patients with COVID-19: A ‘snapshot’ Infectious Diseases International Research Initiative (ID-IRI) survey. J Antimicrob Chemother. 2020;75:3386-3390.
Google Scholar, Crossref
- Liu C, Wen Y, Wan W, et al. Clinical characteristics and antibiotics treatment in suspected bacterial infection patients with COVID-19. Int Immunopharmacol. 2021;90:107157.
Google Scholar, Crossref
- Seaton RA, Gibbons CL, Cooper L, et al. Survey of antibiotic and antifungal prescribing in patients with suspected and confirmed COVID-19 in Scottish hospitals. J Infect Chemother. 2020;81:952-960.
Google Scholar, Crossref
- Adebisi YA, Jimoh ND, Ogunkola IO, et al. The use of antibiotics in COVID-19 management: A rapid review of national treatment guidelines in 10 African countries. Trop Medi Health. 2021;49:1-5.
Google Scholar, Crossref
- Jing R, Vunnam RR, Schnaubelt E, et al. Co-infection of COVID-19 and influenza A in a hemodialysis patient: A case report. BMC Infect Dis. 2021; 21:1-6.
Google Scholar, Crossref
- Narendrakumar L, Joseph I, Thomas S. Potential effectiveness and adverse implications of repurposing doxycycline in COVID-19 treatment. Expert Rev Anti-Infect Ther. 2021;19:1001-1008.
Google Scholar, Crossref
- Pani A, Lauriola M, Romandini A, et al. Macrolides and viral infections: Focus on azithromycin in COVID-19 pathology. Int J Antimicrob Agents. 2020;56:106053.
Google Scholar, Crossref
- Ulrich H, Pillat MM. CD147 as a target for COVID-19 treatment: Suggested effects of azithromycin and stem cell engagement. Stem Cell Rev Rep. 2020;16:434-440.
Google Scholar, Crossref
- Echeverría-Esnal D, Martin-Ontiyuelo C, Navarrete-Rouco ME, et al. Azithromycin in the treatment of COVID-19: A review. Expert Rev Anti-Infect Ther. 2021;1:147-163.
Google Scholar, Crossref
- Sai Disha K, Rashmi Puranik, Sudheesh N, et al. Structure-based identification of small molecules against influenza A virus endonuclease: An in silico and in vitro approach. Pathog Dis. 2020;78:ftaa032.
Google Scholar, Crossref
- Lin C, Li Y, Zhang Y, et al. Ceftazidime is a potential drug to inhibit SARS-CoV-2 infection in vitro by blocking spike protein–ACE2 interaction. Signal Transduct Target Ther. 2021;6:1-4.
Google Scholar, Crossref
- Karampela I, Dalamaga M. Could respiratory fluoroquinolones, levofloxacin and moxifloxacin, prove to be beneficial as an adjunct treatment in COVID-19? Arch Med Res. 2020;51:741-742.
Google Scholar, Crossref
- US Food and Drug Administration. Drug Safety Communication: FDA warns about increased risk of ruptures or tears in the aorta blood vessel with fluoroquinolone antibiotics in certain patients. 2018.
Google Scholar, Crossref
- Al-Azzam S, Mhaidat NM, Banat HA, et al. An assessment of the impact of coronavirus disease (COVID-19) pandemic on national antimicrobial consumption in Jordan. Antibiotics. 2021;10:690.
- Van Gorp GA, Sanders PJ, Van Waardenburg DA, et al. COVID-19 pneumonia successfully managed with high-flow nasal cannula in a 15-year-old boy. BMJ Case Rep CP. 2021;14:e239682.
Google Scholar, Crossref
- Beraldo RF, Marcondes MB, Dos Santos MN, et al. COVID-19 in a patient with liver cirrhosis. Am J Med Case Rep. 2021;22:e929948-1.
Google Scholar, Crossref
- Haraszti S, Sendil S, Jensen N. Delayed presentation of acute generalized exanthematous pustulosis following treatment with cefepime in a patient with COVID-19 without the use of hydroxychloroquine. Am J Med Case Rep. 2020;21:e926901-1.
Google Scholar
- Min JY, Jang YJ. Macrolide therapy in respiratory viral infections. Mediat Inflamm. 2012.
Google Scholar, Crossref
- Batiha GE, Zayed MA, Awad AA, et al.Management of SARS-CoV-2 infection: Key focus in macrolides efficacy for COVID-19. Front Med. 2021;8.
Google Scholar, Crossref
- Gyselinck I, Janssens W, Verhamme P, et al. Rationale for azithromycin in COVID-19: An overview of existing evidence. BMJ Open Respir Res. 2021;8(1):e000806.
Google Scholar, Crossref
- Sultana J, Cutroneo PM, Crisafulli S, et al. Azithromycin in COVID-19 patients: Pharmacological mechanism, clinical evidence and prescribing guidelines. Drug Safety. 2020;43:691-698.
Google Scholar, Crossref
- Arshad S, Kilgore P, Chaudhry ZS, et al. Treatment with hydroxychloroquine, azithromycin, and combination in patients hospitalized with COVID-19. IntJ Infect Dis. 2020;97:396-403.
Google Scholar, Crossref