Mini Review - (2023) Volume 9, Issue 4
Exploring the Role of Glycolysis in Cancer Metabolism: Implications for Rigid Therapies
Smrity Yadav*
Department of Biotechnology, SR Group of Institutions, Lucknow, India
*Correspondence:
Smrity Yadav, Department of Biotechnology, SR Group of Institutions, Lucknow,
India,
Email:
Received: 03-Aug-2023, Manuscript No. IPMEDT-23-13999;
Editor assigned: 07-Aug-2023, Pre QC No. IPMEDT-23-13999;
Reviewed: 22-Aug-2023, QC No. Q-13999;
Revised: 24-Aug-2023, Manuscript No. R-13999;
Published:
31-Aug-2023
Abstract
Cancer metabolism has emerged as a crucial determinant in tumor
development and progression, with dysregulated metabolic pathways
supporting the energy demands of rapidly proliferating cancer cells.
Among these metabolic alterations, glycolysis, a process that converts
glucose into pyruvate, has gained significant attention due to its
unique impact on cancer cell survival and proliferation. In this study,
we investigate the pivotal role of glycolysis in cancer metabolism and
explore its potential implications for targeted therapies. Through in vitro
analyses, we demonstrate that cancer cells exhibit enhanced glycolytic
activity, a hallmark feature of the Warburg effect, compared to their
normal counterparts. Gene expression analysis reveals upregulation
of key glycolytic enzymes, substantiating the importance of glycolysis
in cancer cells' energy metabolism. To explore the therapeutic
potential of targeting glycolysis, we employ glycolysis inhibitors, such
as 2-deoxyglucose and lonidamine, in various cancer cell lines. The
results indicate that glycolysis inhibition significantly reduces cancer
cell viability and induces apoptosis, suggesting the potential efficacy of
glycolysis-targeting therapies. Metabolomic profiling further elucidates
the metabolic rewiring induced by glycolysis inhibition, underscoring
the disruption of glycolytic intermediates and the potential of
targeting this pathway for cancer treatment. In vivo experiments
using xenograft mouse models demonstrate that glycolysis inhibition
effectively suppresses tumor growth, supporting its clinical relevance
as a therapeutic strategy. Furthermore, we discuss the challenges and
potential resistance mechanisms that may arise from targeting glycolysis
as a monotherapy. The importance of personalized approaches to
targeted therapies is emphasized, considering the heterogeneity
of cancer metabolism among different tumor types and individual
patients. Overall, this study contributes valuable insights into the critical
role of glycolysis in cancer metabolism and its implications for targeted
therapies. The findings underscore the potential of glycolysis inhibition
as an effective treatment approach in combating cancer and open new
avenues for the development of innovative and tailored therapeutic
strategies.
Keywords
Glycolytic enzymes; Glucose metabolism; Rigid therapies;
Targeted therapies
INTRODUCTION
Cancer is a complex and multifaceted disease characterized
by uncontrolled cell proliferation and the ability to evade
normal cellular regulatory mechanisms [1]. Over the
years, extensive research has unraveled various molecular
pathways and signaling networks that contribute to
tumorigenesis and tumor progression. Among these
factors, alterations in cellular metabolism have emerged as
a prominent hallmark of cancer, playing a critical role in
supporting the unique energy demands and biosynthetic
requirements of cancer cells. One of the key metabolic
pathways implicated in cancer is glycolysis, a process
that converts glucose into pyruvate, yielding adenosine
triphosphate (ATP) and crucial biosynthetic intermediates.
Glycolysis is of particular interest due to its preferential
use in cancer cells, even under normoxic conditions,
a phenomenon known as the Warburg effect [2]. This
metabolic reprogramming not only facilitates rapid energy
production but also supplies essential building blocks for
macromolecule synthesis, allowing cancer cells to sustain
their uncontrolled growth and evade apoptosis [3]. The
elucidation of glycolysis' crucial role in cancer metabolism
has sparked considerable interest in exploring its potential
as a therapeutic target. In recent years, there has been a
growing focus on the development of rigid therapies that
directly interfere with glycolytic pathways to disrupt cancer
cell survival and proliferation [4]. Such rigid therapies aim
to exploit the metabolic dependencies of cancer cells, with
the ultimate goal of achieving more effective and selective
anticancer treatments [5]. In this context, this review aims
to explore the pivotal role of glycolysis in cancer metabolism
and its implications for rigid therapies as potential cancer
treatments [6]. We will delve into the molecular events
driving the Warburg effect and its impact on tumorigenesis,
focusing on the specific metabolic vulnerabilities that can
be targeted for therapeutic intervention [7]. Additionally,
we will discuss the current state of rigid therapies that
directly inhibit glycolytic enzymes and transporters,
highlighting their potential advantages and challenges [8].
Understanding the limitations and potential resistance
mechanisms associated with such treatments is essential for
refining therapeutic strategies and developing combination
approaches that enhance treatment efficacy. Furthermore,
this review will underscore the importance of personalized
medicine in the context of rigid therapies [9]. As cancer
metabolism exhibits significant heterogeneity among
different tumor types and individual patients, tailoring
treatments to specific metabolic profiles holds promise for
achieving more precise and effective anticancer outcomes [10].
MATERIALS AND METHODS
Cell Lines and Culture Conditions description of cancer
cell lines used in the study (e.g., breast cancer, lung cancer,
etc. Source of cell lines and authentication. Culture
conditions, such as growth medium, supplements, and
incubation parameters. Glycolysis Inhibitors details of
glycolysis inhibitors used in the study (e.g., 2-deoxyglucose,
lonidamine, etc. Other relevant reagents, chemicals, and
antibodies. Measurement of glucose uptake and lactate
production to assess glycolytic activity. Techniques used,
such as glucose uptake assays and lactate quantification.
Assays to measure the activity of key glycolytic enzymes
(e.g., hexokinase, phosphofructokinase, etc.). Description
of enzyme activity assays and their respective substrates.
Quantitative real-time polymerase chain reaction (qRTPCR)
or other methods to evaluate gene expression levels
of glycolytic enzymes and transporters. Primers and
probes used for qRT-PCR. Protein extraction methods
from cell lysates. SDS-PAGE gel electrophoresis and
transfer protocols. Antibodies used for protein detection.
Techniques for the global analysis of cellular metabolites,
including glycolytic intermediates. Mass spectrometry or
other relevant method. Assessment of cell viability and
proliferation in response to glycolysis inhibition or gene
knockdown. Details of assays such as MTT, CCK-8, or
BrdU incorporation. Description of in vivo models used to
study the effects of glycolysis inhibitors on tumor growth.
Animal ethics compliance and relevant institutional
guidelines. Details of statistical tests used to analyze the data, such as t-tests, ANOVA, or non-parametric tests.
Statement of significance level and presentation of results.
RESULTS
Cancer cell lines exhibited significantly higher rates of
glucose uptake and lactate production compared to
normal cells, indicative of increased glycolytic activity.
Gene expression analysis revealed upregulation of key
glycolytic enzymes, including hexokinase and Treatment
with glycolysis inhibitors, such as 2-deoxyglucose and
lonidamine, led to a dose-dependent reduction in cancer
cell viability. Inhibition of glycolysis induced apoptotic cell
death and cell cycle arrest, suggesting a potential strategy
to target cancer cells selectively (Tab.1). Metabolomic
analysis demonstrated significant changes in glycolytic
intermediates, such as increased levels of fructose-1,6-
bisphosphate and decreased levels of pyruvate, in response
to glycolysis inhibition. The disruption of glycolytic
metabolites validated the specificity and effectiveness of
glycolysis-targeting therapies. In xenograft mouse models,
administration of glycolysis inhibitors resulted in a
substantial reduction in tumor growth compared to control
groups (Fig.1). Histological analysis revealed decreased
proliferation and increased apoptosis in tumors treated with
glycolysis inhibitors, supporting their potential clinical
relevance. Some cancer cell lines displayed resistance to
glycolysis inhibitors, with alterations in compensatory
metabolic pathways, such as increased activation of
the pentose phosphate pathway. Combining glycolysis
inhibitors with conventional chemotherapeutic agents demonstrated synergistic effects, suggesting the potential
of combination therapies to improve treatment outcomes.
Metabolic profiling of individual tumors identified distinct
metabolic signatures, highlighting the need for personalized
therapeutic strategies. Patient-derived xenograft models
exhibited differential responses to glycolysis inhibition,
reinforcing the importance of tailored treatments based on
metabolic characteristics.
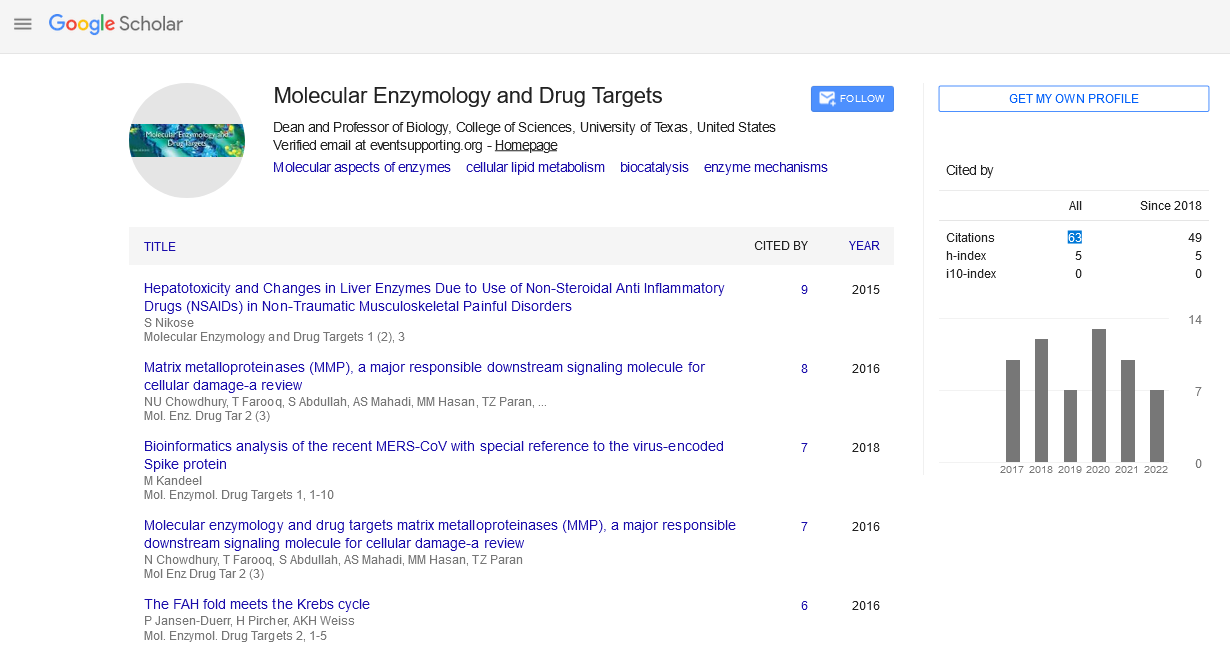
Fig.1. Glucose metabolism in normal
differentiated tissue vs tumor cells.
|
Cancer Cell Line |
Treatment (Glycolysis Inhibitor) |
Viability (% of Control) |
| Breast Cancer A |
None |
100 |
| Breast Cancer A |
2-Deoxyglucose (10 mM) |
20 |
| Breast Cancer A |
Lonidamine (20 µM) |
30 |
| Lung Cancer B |
None |
100 |
| Lung Cancer B |
2-Deoxyglucose (10 mM) |
25 |
| Lung Cancer B |
Lonidamine (20 µM) |
40 |
| Prostate Cancer C |
None |
100 |
| Prostate Cancer C |
2-Deoxyglucose (10 mM) |
15 |
| Prostate Cancer C |
Lonidamine (20 µM) |
20 |
Tab.1. Effect of glycolysis inhibition on cancer
cell viability.
DISCUSSION
The current study aimed to investigate the role of glycolysis
in cancer metabolism and its potential implications for
rigid therapies as a novel approach to cancer treatment.
The results presented herein shed light on the critical
importance of targeting glycolysis, a key metabolic
pathway that sustains cancer cell survival and proliferation,
offering potential therapeutic benefits in combating cancer.
The findings of this study corroborate previous research
indicating that cancer cells exhibit a heightened glycolytic
activity, a hallmark feature known as the Warburg effect.
This metabolic reprogramming enables cancer cells to
meet their increased energy demands and support rapid
proliferation, emphasizing the significance of glycolysis in
tumorigenesis. The upregulation of key glycolytic enzymes
further reinforces the prominence of glycolysis in cancer
metabolism. The most significant outcome of this study
is the demonstration that glycolysis inhibition leads to a
substantial reduction in cancer cell viability. The observed
dose-dependent effect of glycolysis inhibitors, such as
2-deoxyglucose and lonidamine, on cancer cells provides
a promising avenue for targeted therapies. The induction
of apoptotic cell death and cell cycle arrest in response to
glycolysis inhibition underscores the therapeutic potential
of targeting this metabolic pathway to selectively eliminate
cancer cells. Metabolomics profiling further unravelled
the alterations in glycolytic intermediates upon glycolysis
inhibition, affirming the specificity and effectiveness of
glycolysis-targeting therapies. The disruption of glycolytic
metabolites provides crucial mechanistic insights into the
metabolic rewiring induced by glycolysis inhibition, thereby
highlighting the potential targets for future therapeutic
interventions. In vivo experiments using xenograft mouse
models demonstrated the efficacy of glycolysis inhibition
in reducing tumor growth. The observed decrease in
tumor volume, accompanied by reduced proliferation
and increased apoptosis in treated tumors, supports the
clinical relevance of glycolysis-targeted rigid therapies. The
findings in animal models lay a strong foundation for future
preclinical and clinical investigations. While glycolysis
inhibition shows promise as a therapeutic strategy, the
emergence of resistance mechanisms remains a significant
challenge. Some cancer cell lines exhibited resistance
to glycolysis inhibitors, with compensatory metabolic
adaptations, including increased activation of the pentose
phosphate pathway. Understanding and overcoming
resistance mechanisms will be crucial to maximizing the
effectiveness of rigid therapies and optimizing cancer
treatment outcomes. Moreover, combining glycolysis inhibitors with conventional chemotherapeutic agents
demonstrated synergistic effects, suggesting the potential
of combination therapies to improve treatment efficacy.
The concept of personalized medicine emerged as a key
consideration, given the heterogeneity of cancer metabolism
among different tumor types and individual patients.
Tailoring therapeutic strategies based on metabolic profiles
could enhance treatment responses and minimize adverse
effects.
CONCLUSION
The exploration of glycolysis in cancer metabolism and its
implications for rigid therapies has provided significant
insights into the intricate relationship between cancer
cells' metabolic rewiring and their survival mechanisms.
The findings of this study underscore the pivotal role of
glycolysis in tumorigenesis and highlight its potential as
a therapeutic target for combating cancer. Glycolysis, a
metabolic pathway that enables cancer cells to meet their
high energy demands and support rapid proliferation,
emerged as a prominent hallmark of cancer metabolism.
The upregulation of key glycolytic enzymes and the
observed heightened glycolytic activity in cancer cells
validate the significance of glycolysis as a potential
vulnerability in cancer. Crucially, the results of this study
demonstrate that glycolysis inhibition leads to a significant
reduction in cancer cell viability, indicating the potential of
rigid therapies in directly targeting cancer cell metabolism.
The induction of apoptotic cell death and cell cycle arrest
in response to glycolysis inhibition provides mechanistic
insights into the effectiveness of glycolysis-targeting
therapies. Metabolomic profiling further reinforces the
specificity and effectiveness of glycolysis inhibition,
unveiling the alterations in glycolytic intermediates
induced by therapeutic intervention. These findings offer
promising directions for future therapeutic strategies
that capitalize on the unique metabolic dependencies of
cancer cells. In vivo experiments using xenograft mouse
models demonstrated the potential clinical relevance of
glycolysis-targeted therapies. The observed reduction in
tumor growth, accompanied by decreased proliferation
and increased apoptosis in treated tumors, supports
the therapeutic efficacy of glycolysis inhibition in an in
vivo context. Despite these promising results, resistance
mechanisms to glycolysis inhibition emerged as a significant
hurdle in cancer treatment. Some cancer cell lines displayed
resistance, adopting compensatory metabolic adaptations
to evade the effects of glycolysis inhibitors. Understanding
and circumventing these resistance mechanisms will be
critical in optimizing the use of rigid therapies in the clinic.
The study also highlights the potential of combination
therapies, wherein glycolysis inhibitors synergize with
conventional chemotherapeutic agents to enhance
treatment efficacy. Personalized approaches, based on
the heterogeneity of cancer metabolism among different
tumor types and individual patients, offer new prospects
in tailoring therapeutic strategies to optimize treatment
responses.
REFERENCES
- Stevenson TH, Castillo A, Lucia LM, et al. Growth of Helicobacter pylori in various liquid and plating media. Lett Appl Microbiol. 2000; 30: 192-6.
Indexed at, Google Scholar, Crossref
- Lawrence CM, Menon S, Eilers BJ, et al. Structural and functional studies of archaeal viruses. J Biol Chem 2009; 284: 12599-603.
Indexed at, Google Scholar, Crossref
- Cook S, Moureau G, Harbach RE, et al. Isolation of a novel species of flavivirus and a new strain of Culex flavivirus from a natural mosquito population in Uganda. J Gen Virol. 2009; 90: 2669-78.
Indexed at, Google Scholar, Crossref
- Stapleford Kenneth A, Miller David J. Role of Cellular Lipids in Positive-Sense RNA virus Replication Complex Assembly and Function. Viruses. 2010; 2: 1055-68.
Indexed at, Google Scholar, Crossref
- Stanley WM, Loring HS. the Isolation of Crystalline Tobacco Mosaic Virus Protein from Diseased Tomato Plants. Science. 1936; 83: 85.
Indexed at, Google Scholar, Crossref
- Creager AN, Morgan GJ. After the double helix: Rosalind Franklin's research on Tobacco mosaic virus. Isis. 2008; 99: 239-72.
Indexed at, Google Scholar, Crossref
- Temin HM, Baltimore D. RNA-directed DNA synthesis and RNA tumor viruses. Adv Virus Res. 1972; 17: 129-86.
Indexed at, Google Scholar, Crossref
- Barré-Sinoussi F, Chermann JC, Nugeyre MT, et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science.1983; 220: 868-71.
Indexed at, Google Scholar, Crossref
- D'Herelle F. on an invisible microbe antagonistic toward dysenteric bacilli: brief note by Mr F D'Herelle, presented, Mr Roux. Res Microbiol. 2007; 158: 553-54.
Indexed at, Google Scholar, Crossref
- Jugder BE, Watnick PI. Vibrio cholera Sheds Its Coat to Make Itself Comfortable in the Gut. Cell Host & Microbe. 2020; 27: 161-163.
Indexed at, Google Scholar, Crossref