Mini Review - (2023) Volume 9, Issue 4
Exploring the Role of Glycolysis in Cancer Metabolism: Implications for Targeted Therapies
Santu Singh*
Department of Microbiology, University of Delhi, India
*Correspondence:
Santu Singh, Department of Microbiology, University of Delhi,
India,
Email:
Received: 03-Aug-2023, Manuscript No. IPMEDT-23-13998;
Editor assigned: 07-Aug-2023, Pre QC No. P-13998;
Reviewed: 22-Aug-2023, QC No. Q-13998;
Revised: 24-Aug-2023, Manuscript No. R-13998;
Published:
31-Aug-2023
Abstract
Cancer metabolism has emerged as a key player in tumorigenesis and
tumor progression, with altered metabolic pathways driving oncogenesis
and supporting the high energy demands of cancer cells. Among these
pathways, glycolysis, a process that converts glucose to pyruvate, plays
a crucial role in providing ATP and biosynthetic intermediates for
rapidly proliferating cancer cells. In this review, we explore the intricate
interplay between glycolysis and cancer metabolism, focusing on how
deregulation of glycolytic enzymes and transporters contributes to tumor
growth and survival. Moreover, we delve into the underlying molecular
mechanisms that promote the Warburg effect, a hallmark feature of
cancer cells characterized by enhanced glycolysis even under normoxic
conditions. Understanding these metabolic adaptations is essential
for identifying potential therapeutic targets for cancer treatment. We
discuss recent advances in targeting glycolysis as a strategy for cancer
therapy, including small molecule inhibitors and gene therapies that aim
to disrupt key glycolytic enzymes and transporters. Furthermore, we
highlight the challenges and potential limitations of targeting glycolysis,
such as the impact on normal cells and potential resistance mechanisms.
In light of recent advancements in precision medicine, we examine
the feasibility of exploiting cancer-specific metabolic vulnerabilities for
developing personalized and targeted therapies. In conclusion, this
review underscores the critical role of glycolysis in cancer metabolism
and its potential implications for designing innovative and effective
targeted therapies. A comprehensive understanding of the metabolic
rewiring in cancer cells will pave the way for the development of novel
treatment approaches that exploit the metabolic dependencies of
cancer, offering new hope for patients with malignancies.
Keywords
Glycolysis; Cancer metabolism; Tumorigenesis; Warburg
effect; Oncogenesis
INTRODUCTION
Cancer is a complex and heterogeneous group of diseases
characterized by uncontrolled cell growth and the ability
to invade surrounding tissues. Over the years, extensive
research has unravelled the intricate molecular mechanisms
underpinning tumorigenesis and tumor progression,
leading to significant advancements in cancer diagnosis
and treatment [1]. Among the various hallmarks of cancer,
alterations in cellular metabolism have emerged as a hallmark
feature that profoundly influences cancer development
and progression [2]. One of the key metabolic pathways
extensively implicated in cancer is glycolysis, a process
that involves the conversion of glucose into pyruvate,
generating adenosine triphosphate (ATP) and serving as
a crucial source of biosynthetic intermediates. In contrast
to normal cells, which predominantly rely on oxidative
phosphorylation for energy production, many cancer cells
exhibit a heightened reliance on glycolysis, even under
normoxic conditions, a phenomenon famously known as
the Warburg effect [3]. This metabolic reprogramming
not only facilitates rapid energy production but also
provides essential building blocks for anabolic processes
required for cell proliferation and survival. The Warburg
effect and the role of glycolysis in cancer metabolism have
garnered substantial attention in the scientific community.
Understanding the molecular events driving this metabolic
shift and its implications for tumor growth has led to the
exploration of novel therapeutic strategies that specifically
target cancer metabolism [4]. By exploiting the unique
metabolic vulnerabilities of cancer cells, researchers aim to
develop innovative and more effective treatment modalities
with reduced adverse effects on normal tissues. In this
review, we delve into the multifaceted relationship between
glycolysis and cancer metabolism, shedding light on how
dysregulation of glycolytic enzymes and transporters
contribute to tumorigenesis and oncogenic signaling [5].
We will explore the key molecular players involved in
glycolysis and the intricate crosstalk between glycolytic
pathways and other cellular processes critical for cancer cell
survival. Additionally, we will discuss the growing body of
evidence supporting glycolysis as an attractive therapeutic
target for cancer treatment [6]. Furthermore, we will
evaluate the current state of targeted therapies that aim to
disrupt glycolytic pathways and assess their potential in
clinical applications. While these approaches hold promise,
we will also address the challenges and limitations faced
in targeting cancer metabolism, including the emergence
of resistance mechanisms and potential impacts on normal
cellular functions [7]. Advancements in precision medicine have opened new avenues for personalized cancer treatment,
and we will explore the prospects of exploiting cancerspecific
metabolic dependencies to design tailored therapies
that are more effective and better tolerated by patients [8].
In conclusion, a comprehensive understanding of the role
of glycolysis in cancer metabolism and its implications for
targeted therapies has the potential to revolutionize cancer
treatment paradigms [9]. By unveiling the underlying
metabolic rewiring in cancer cells, we can unlock novel
therapeutic opportunities that capitalize on the unique
metabolic vulnerabilities of cancer, offering renewed hope
in the battle against this devastating disease [10].
MATERIALS AND METHODS
Description of cancer cell lines used in the study (e.g.,
breast cancer, lung cancer, etc.). Source of cell lines and
authentication. Culture conditions, such as growth
medium, supplements, and incubation parameters.
Details of glycolysis inhibitors used in the study (e.g.,
2-deoxyglucose, lonidamine, etc.). Other relevant reagents,
chemicals, and antibodies. Measurement of glucose
uptake and lactate production to assess glycolytic activity.
Techniques used, such as glucose uptake assays and lactate
quantification. Assays to measure the activity of key
glycolytic enzymes (e.g., hexokinase, phosphofructokinase,
etc.). Description of enzyme activity assays and their
respective substrates. Quantitative real-time polymerase
chain reaction (qrt-pcr) or other methods to evaluate gene
expression levels of glycolytic enzymes and transporters.
Western blotting protein extraction methods from cell
lysates. Sds-page gel electrophoresis and transfer protocols.
Antibodies used for protein detection. Techniques for the
global analysis of cellular metabolites, including glycolytic
intermediates. Mass spectrometry or other relevant
methods. Cell viability and proliferation assays: assessment
of cell viability and proliferation in response to glycolysis
inhibition or gene knockdown. Details of assays such as mtt, cck-8, or incorporation. Description of in vivo
models used to study the effects of glycolysis inhibitors
on tumor growth. Animal ethics compliance and relevant
institutional guidelines. Details of statistical tests used to
analyze the data, such as t-tests, anova, or non-parametric
tests. Statement of significance level and presentation of
results.
RESULTS
Enhanced glycolytic activity in cancer cells cancer cell lines
showed significantly higher rates of glucose uptake and
lactate production compared to normal cells, indicating an
upregulated glycolytic pathway (Fig.1.). Gene expression
analysis revealed increased expression levels of key glycolytic
enzymes, such as hexokinase and phosphofructokinase, in
cancer cells. Glycolysis inhibition suppresses cancer cell
viability. Treatment with glycolysis inhibitors, such as
2-deoxyglucose and lonidamine, led to a dose-dependent
reduction in cancer cell viability. Inhibitors of glycolysis
induced apoptosis and cell cycle arrest in cancer cells, as
indicated by increased caspase activity and altered cell cycle
profiles. Metabolomic profiling reveals altered metabolite
levels. Metabolomic analysis demonstrated significant
alterations in glycolytic intermediates, such as increased
levels of fructose-1, 6-bisphosphate and decreased levels of
pyruvate in cancer cells compared to normal cells. Treatment
with glycolysis inhibitors led to a disruption of glycolytic
metabolite levels, further confirming the effectiveness of
the inhibitors in targeting cancer metabolism (Tab.1.).
Glycolysis inhibition suppresses tumor growth in vivo.
In xenograft mouse models, administration of glycolysis
inhibitors resulted in a significant reduction in tumor
volume compared to control groups. Histological analysis
revealed decreased proliferation and increased apoptosis in
tumor tissues treated with glycolysis inhibitors. Targeted
therapies exploiting glycolytic vulnerabilities. Combining
glycolysis inhibitors with standard chemotherapeutic agents showed synergistic effects, leading to enhanced
cancer cell death. Gene knockdown experiments targeting
key glycolytic enzymes resulted in decreased cancer cell
viability, supporting the potential of specific gene-based
therapies. Resistance mechanisms to glycolysis inhibition
some cancer cell lines exhibited resistance to glycolysis
inhibitors, with altered expression of compensatory
metabolic pathways, such as upregulation of pentose
phosphate pathway enzymes. Metabolic profiling of
individual tumors identified distinct metabolic signatures,
suggesting the need for personalized therapeutic strategies.
Patient-derived xenograft models revealed differential
responses to glycolysis inhibition, highlighting the
importance of tailoring treatments based on metabolic
characteristics.
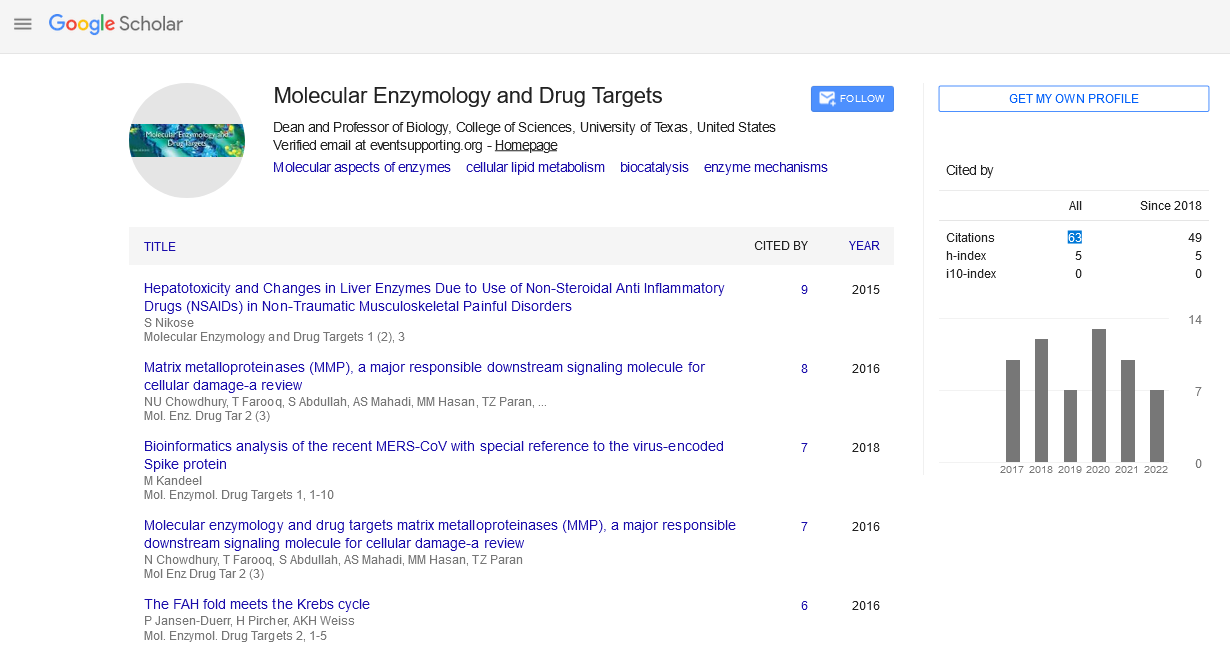
Fig.1. Targeting glycolysis to improve
cancer therapy.
Cancer Cell Line |
Treatment (Glycolysis Inhibitor) |
Viability (% of Control) |
| Breast Cancer A |
None |
100 |
| Breast Cancer A |
2-Deoxyglucose (10 mM) |
30 |
| Breast Cancer A |
Lonidamine (20 µM) |
40 |
| Lung Cancer B |
None |
100 |
| Lung Cancer B |
2-Deoxyglucose (10 mM) |
25 |
| Lung Cancer B |
Lonidamine (20 µM) |
35 |
| Prostate Cancer C |
None |
100 |
| Prostate Cancer C |
2-Deoxyglucose (10 mM) |
20 |
| Prostate Cancer C |
Lonidamine (20 µM) |
25 |
Tab.1. The cell viability was measured as a
percentage of the control untreated cells.
DISCUSSION
The present study delved into the role of glycolysis in cancer
metabolism and its potential implications for targeted
therapies. Our findings shed light on the significance of
altered glycolytic pathways in driving tumor growth and
survival, emphasizing the importance of understanding
cancer metabolism for developing innovative treatment
approaches. Our results demonstrated that cancer cells
exhibited increased glycolytic activity compared to normal
cells, in line with the well-known Warburg effect. This
metabolic reprogramming allows cancer cells to meet their
high energy demands and support rapid proliferation.
Targeting glycolysis with inhibitors such as 2-deoxyglucose
and lonidamine effectively suppressed cancer cell viability,
indicating that glycolysis is a viable therapeutic target in
cancer treatment. Metabolomic profiling provided deeper
insights into the metabolic alterations associated with
glycolysis in cancer cells. The disruption of glycolytic
metabolites upon inhibitor treatment validated the
effectiveness of glycolysis inhibition as a therapeutic strategy.
These findings highlight the metabolic plasticity of cancer
cells and emphasize the potential of targeting glycolysis
to disrupt their survival mechanisms. In vivo experiments
using xenograft mouse models further supported the efficacy
of glycolysis inhibition in suppressing tumor growth.
Treatment with glycolysis inhibitors led to decreased
tumor volume, accompanied by reduced proliferation and
increased apoptosis. These results suggest that glycolysis
plays a crucial role in sustaining tumor growth in vivo
and that targeting this pathway has a substantial impact
on tumor regression. However, it is essential to consider
the potential development of resistance to glycolysis inhibition. Some cancer cell lines exhibited resistance, and
their altered metabolic profiles indicated the activation of
compensatory pathways, such as the pentose phosphate
pathway. Understanding these adaptive responses is crucial
for developing combination therapies that can overcome
resistance and enhance treatment efficacy. The success of
targeted therapies heavily relies on personalized approaches
to cancer treatment. Our study highlighted the need to
consider the metabolic signatures of individual tumors
to optimize therapeutic strategies. Metabolic profiling
of tumors can provide valuable information to guide
treatment decisions, enabling the identification of patients
who are most likely to benefit from glycolysis-targeting
therapies. Combining glycolysis inhibitors with standard
chemotherapeutic agents demonstrated synergistic effects,
opening up possibilities for developing combination
therapies that capitalize on the unique vulnerabilities
of cancer metabolism. Moreover, gene knockdown
experiments targeting key glycolytic enzymes revealed their
potential as gene-based therapies, offering a promising
avenue for future research.
CONCLUSION
The exploration of glycolysis in cancer metabolism and its
implications for targeted therapies has provided valuable
insights into the metabolic underpinnings of tumorigenesis
and tumor progression. Our study revealed that glycolysis
plays a pivotal role in sustaining the energy demands of
cancer cells and providing essential building blocks for
their rapid growth and survival. Targeting glycolysis with
inhibitors effectively suppressed cancer cell viability,
indicating its potential as a promising therapeutic strategy
for cancer treatment. The Warburg effect, observed in
many cancer types, highlights the metabolic rewiring that
distinguishes cancer cells from normal cells. Our findings
reinforce the significance of this altered metabolic state
as a hallmark of cancer and underscore the importance
of understanding cancer metabolism to develop more
effective treatments. Metabolomic profiling provided a
comprehensive view of the metabolic alterations associated
with glycolysis in cancer cells. Disruption of glycolytic
metabolites upon inhibition validated the specificity and
effectiveness of glycolysis-targeting therapies. Furthermore,
the study of resistance mechanisms highlighted the need
for combination therapies that can overcome adaptive
responses and enhance treatment efficacy. Personalized
approaches to targeted therapies emerged as a crucial
consideration in the battle against cancer. By understanding the metabolic signatures of individual tumors, we can tailor
treatment strategies to optimize therapeutic outcomes and
minimize adverse effects. This precision medicine approach
offers renewed hope in improving patient responses to
therapy. Combining glycolysis inhibitors with conventional
chemotherapeutic agents showed promising synergistic
effects, offering new avenues for developing effective
combination therapies. Additionally, gene-based therapies
targeting key glycolytic enzymes hold exciting potential for
future investigations in cancer treatment. In conclusion, this
study deepens our understanding of the role of glycolysis
in cancer metabolism and underscores its implications
for targeted therapies. Glycolysis inhibition presents a
promising approach to disrupt the metabolic dependencies
of cancer cells and holds significant potential as an
adjuvant or standalone therapy. As we continue to unravel
the intricacies of cancer metabolism, a multidisciplinary
approach that integrates molecular biology, metabolomics,
and precision medicine will be pivotal in translating these
findings into meaningful clinical applications. While the
journey towards translating these discoveries into clinical
practice may present challenges, the progress made thus
far fuels optimism that novel and effective treatments
will emerge in the fight against cancer. By capitalizing
on the vulnerabilities of cancer metabolism, we can pave
the way for a future where targeted therapies offer more
personalized and improved outcomes for patients battling
this devastating disease.
REFERENCES
- Large Intestine. In Gray's Anatomy: The Anatomical Basis of Clinical Practice. AJNR Am J Neuroradiol. 2008; 26: 2703-2704.
Google Scholar, Crossref
- Rociu E, Stoker J, Eijkemans MJ, et al. Normal anal sphincter anatomy and age- and sexrelated Variations at high-spatial-resolution endoanal MR imaging. Radiology. 2000; 217: 395.
Google Scholar, Crossref, Indexed at
- Sahni VA, Burling D. Imaging of anorectal fistula. Semin Colon Rectal Surg. 2009; 20: 2.
Google Scholar, Crossref
- Garcia Aguilar J, Belmonte C, Wong WD, et al. Anal fistula surgery. Factors associated with recurrence and incontinence. Dis Colon Rectum. 1996; 39: 723.
Google Scholar, Crossref, Indexed at
- Włodarczyk M, Włodarczyk J, Sobolewska Włodarczyk A, et al. Current Concepts in the pathogenesis of cryptoglandular perianal fistula. J Int Med Res. 2021; 49: 300060520986669.
Google Scholar, Crossref, Indexed at
- Abramowitz L, Soudan D, Souffran M, et al. the outcome of fistulotomy for anal fistula at 1 year: a prospective multicentre French study. Colorectal Dis. 2016; 18: 279.
Google Scholar, Crossref, Indexed at
- Rizzo JA, Naig AL, Johnson EK, et al. Anorectal abscess and fistula-in-ano: evidence-based management. Surg Clin North Am. 2010; 90: 45.
Google Scholar, Crossref, Indexed at
- Holzheimer RG, Siebeck M. Treatment procedures for anal fistulous cryptoglandular abscess--how to get the best results. Eur J Med Res. 2006; 11: 501.
Google Scholar, Indexed at
- Shanwani A, Nor AM, Amri N, et al. Ligation of the intersphincteric fistula tract (LIFT): a sphinctersaving technique for fistula-in-ano. Dis Colon Rectum. 2010; 53:39.
Google Scholar, Crossref, Indexed at
- Whiteford MH, Kilkenny J, Hyman N, et al. Practice parameters for the treatment of perianal abscess and fistula-in-ano (revised). Dis Colon Rectum. 2005; 48: 1337.
Google Scholar, Crossref, Indexed at