Syed Ali Behram Subawari1*, Layba Awais1, M Waqar Afzal1, Kamran Hanif2, Ayesha Sarfraz3, Mehvish Saleem4 and Muhammad Kashif5
1College of Rehabilitation Sciences, University Lahore, Pakistan
2Department of Biostatistics, University of Lahore, Pakistan
3deMont Morency College of Dentistry, Lahore, Pakistan
4Bakhtawar Amin Dental College, Multan, Pakistan
5Bakhtawar Amin Dental College, Multan, Pakistan
- *Corresponding Author:
- Syed Ali Behram Subawari
College of Rehabilitation Sciences
University Lahore, Pakistan
Tel: +923346035054
E-mail: themedresearcher@gmail.com
Received Date: March 05, 2020; Accepted Date: March 16, 2020; Published Date: March 20, 2020
Citation: Subawari SAB, Awais L, Afzal MW, Hanif K, Sarfraz A, et al (2020) Frequency and Level of Disability among Patients Wearing Complete Dentures. Health Sci J. 14 No. 2: 703.
DOI: 10.36648/1791-809X.14.2.703
Keywords
Temporomandibular joint disorder; Complete denture; Maxillofacial injuries
Introduction
The temporomandibular joint, in which the lower jaw or mandible connects with the cranium, is located in the front of each ear [1]. Similar to knee articulation, a bicondylar articulation and ellipsoid variety of the synovial joints are formed by the right and left TMJ [2]. The common trait of the synovial joints displayed by this joint include a disk, bone, fibrous capsule, fluid, synovial membrane, and ligaments. However, the characteristics that differentiate and make this joint unique are its articular surface covered by fibrocartilage instead of hyaline cartilage. Movement is not only governed by the shape of the bones, muscles, and ligaments but also by the blockage of the teeth, since both joints are joined by a single mandible bone and cannot move independently of each other [3].
A collective terminology embracing a number of medical issues, which involve the masticatory musculature, the temporomandibular joint or both is known as temporomandibular disorder (TMD). Virtually all theories dealing with the etiology and treatments of TMD have recognized the importance of psychological elements [4]. Complete denture sufferers do no longer suffer from TMJ disturbances' is a statement typically regularly occurring by many dentists and clinicians. This declaration isn't always valid given that few dentists encompass a TMJ exam amongst habitual medical techniques for full denture patients [5]. The research network benefits from the potential to use well-described and clinically relevant traits associated with the phenotype so that it will facilitate further generalizable studies. When clinicians and researchers use the equal criteria, taxonomy, and nomenclature, then medical questions and experience may be greater without difficulty transferred into relevant research questions, and research findings are greater accessible to clinicians to higher diagnose and control their patients [6].
Epidemiological studies have shown that signs and symptoms of mandibular disorder are very common, however prosthodontists have concept that complete denture wearers are spared such complications. However, in latest reported series of patients who have sought recommendation for mandibular dysfunction complete denture wearers were blanketed. According to epidemiological records individuals with few rest of the natural teeth had extra signs and symptoms of disorder than people with most in their natural teeth, and entire denture wearers had greater symptoms of mandibular disorder than the subjects with natural teeth. Mandibular and temporomandibular joint disorder signs have a heterogeneous background; however occlusal instability is an important etiological issue. In complete denture wearers with mandibular disorder, signs regularly disappear after improvement of the occlusion [7].
Dysfunctions of temporomandibular joint are fairly commonplace occurrences and are comprehensively documented within the dental literature. Several authors maintain that inadequate dentitions and unsatisfactory occlusions are the most frequent causes of temporomandibular joint problems. Other investigators, whilst noting that hyper function may additionally deliver rise to myofascial ache, assert that temporomandibular joint disturbances are normally related to disorder of the masticatory muscles [8]. Temporomandibular joint, not like other joints within the human frame, is distinctive in phrases of its anatomy and control of illnesses [9].
The purpose of the study was to find out the frequency and the levels of disability of temporomandibular joint among patients wearing complete dentures. Like other countries, Pakistan will also face the TMD disability among complete denture wearing patients. So awareness to the patient is so important and also to educate the patients about physiotherapy role in the relief of temporomandibular joint disorders.
Methods
A cross-sectional study was conducted and non-probability convenient sampling technique was used to collect 100 complete denture wearing patients. The complete denture wearing patients aged between 40 to 85 years and willing to participate were included. While complete denture wearing patients with fractures, trauma or any other pathological conditions were excluded. Each patient was asked to fill TMD Disability Index questionnaire [10] which consists of 10 questions regarding disability in association with TMD with a total score of 40. Each question is scored from 0 to 4, increasing with severity of disability. Higher scores represent higher levels of disability. Scores 30-40 represent high disability, 20-30 moderate disability, 10 – 20 slight disability, less than 10 represented minimal disability and 0 represented no disability [11]. The data were collected from University College of medicine and dentistry Lahore, Akhtar Saeed Medical and Dental College Lahore, Punjab Dental Hospital Lahore and Islam Medical and Dental College, Sialkot, Pakistan.
Results
A total of 100 complete denture wearing patients participated in this study. Among 100 participants 50(50%) were males and 50(50%) were females. The mean age of the patients was 57.68±10.67 years. The minimum age was 43 years and maximum was 83 years as shown in Table 1.
Table 1 Descriptive statistics for demographic data.
| Gender |
Frequency |
| Male |
50 |
| Female |
50 |
| Total |
100 |
| Age |
| Mean |
57.68 |
| Std. Deviation |
10.670 |
| Minimum |
40 |
| Maximum |
83 |
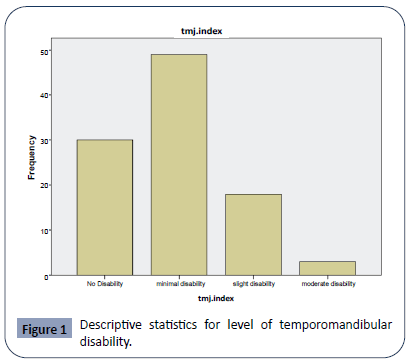
Analysis revealed that among 100 participating patients wearing complete dentures, 30(30%) faced no disability whereas 49(49%) faced minimal disability, 18(18%) faced slight disability and only 3(3%) faced moderate disability as shown in Figure 1.
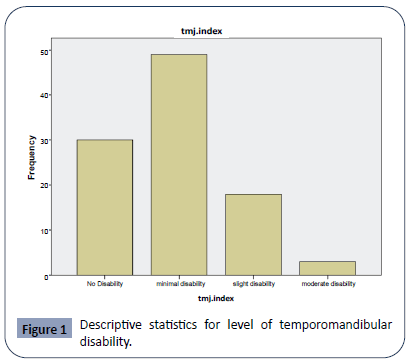
Figure 1: Descriptive statistics for level of temporomandibular disability.
As shown in Table 2, among 100 participating patients, there were 51 (51%) patients who were able to eat as much of anything without discomfort. 28(28%) showed mild pain/discomfort, 18 (18%) showed moderate pain/discomfort and couldn’t eat much of anything. 3(3%) showed severe pain/discomfort and could only eat soft food.
Table 2 Descriptive statistics for normal living activities, non-specialized jaw activities, tinnitus and ringing.
| Normal living activities (eating, chewing). |
Frequency |
Percent |
| Chew as much of anything without pain/discomfort or jaw tiredness. |
51 |
51.0 |
| Chew most anything, but it sometimes causes some discomfort and/or jaw tiredness. |
28 |
28.0 |
| Can’t eat much of anything, because it often causes discomfort, jaw tiredness. |
18 |
18.0 |
| Only eat soft foods because of discomfort, jaw fatigue and restricted opening. |
3 |
3.0 |
| Total |
100 |
100.0 |
| Non-specialized jaw activities (yawning, mouth opening and opening my mouth wide) |
Frequency |
Percent |
| Can yawn in a normal fashion, painlessly. |
68 |
68.0 |
| Can yawn and open mouth fully wide open, but sometimes there is discomfort. |
16 |
16.0 |
| Can yawn and open mouth wide, but it always causes discomfort. |
12 |
12.0 |
| Yawning and opening mouth wide are somewhat restricted by pain. |
4 |
4.0 |
| Total |
100 |
100.0 |
| Tinnitus, or ringing in the ear(s) |
Frequency |
Percent |
| Do not experience ringing in my ear(s). |
71 |
71.0 |
| Experience ringing in ear(s), but it does not interfere with sleep and ability to perform daily activities. |
14 |
14.0 |
| Experience ringing in ear(s) and it interferes with sleep and/or daily activities, but can get an acceptable sleep. |
15 |
15.0 |
| Total |
100 |
100.0 |
| Dizziness (lightheaded, spinning and/or balance disturbances) |
Frequency |
Percent |
| Do not experience dizziness. |
66 |
66.0 |
| Experience dizziness, but it does not interfere with daily activities. |
20 |
20.0 |
| Experience dizziness which interferes somewhat with daily activities. |
8 |
8.0 |
| Experience dizziness which causes a marked impairment in daily activities. |
5 |
5.0 |
| Dizziness which is incapacitating. |
1 |
1.0 |
| Total |
100 |
100.0 |
Regarding non-specialized jaw activities there were 68 (68%) patients who were able to yawn without discomfort. 16(16%) showed mild pain/discomfort while yawning, 12 (12%) showed moderate pain/discomfort while opening the mouth wide. 4(4%) showed severe pain/discomfort and had restricted mouth opening and yawning.
71(71%) patients of the total didn’t experience ringing in the ear(s). 14(14%) experienced ringing in ear(s), but it did not interfere with sleep and/or ability to perform daily activities. 15(15%) experienced ringing in ear(s) which interfered with sleep and/or daily activities.
Analysis showed that 66(66%) patients of the total didn’t experience dizziness. 20(14%) experienced dizziness, but it did not interfere with daily activities. 8(8%) experienced dizziness which interfered somewhat with daily activities. 5(5%) experienced dizziness which caused a marked impairment in the performance of daily activities. 1 (1%) experienced dizziness which was incapacitating.
Discussion
The present study was conducted to determine the frequency and level of disability among patients wearing full dentures. Among 100 participants 50 (50%) were male and 50 (50%) were female. Choy et al. conducted a research of temporomandibular joint disturbances which was executed on 160 complete denture patients A questionnaire inclusive of eighteen questions was used to check the usefulness in figuring out TMJ patients among the sample. The conclusions from this research revealed that about 15% of the complete denture patients in this pattern suffered from TMJ disturbances [5]. The present research was executed on 100 complete denture wearing patients. Each patient was asked to fill TMD Disability Index questionnaire which consists of 10 questions regarding disability in association with TMD with a total score of 40. 30(30%) faced no disability whereas 49(49%) faced minimal disability, 18(18%) faced slight disability and only 3(3%) faced moderate disability.
Prevalence of patients having difficulty in non-specialized jaw activities is 32% in which 16% showed mild pain/discomfort while yawning, 12% showed moderate pain/discomfort while opening the mouth wide. 4% showed severe pain/discomfort and had restricted mouth opening and yawning. Whereas Farrar et al. which stated that 10 of 218 patients were examined for TMJ complaints. Most of them suggested that their jaw “locked” at the same time as performing everyday jaw features which included eating, laughing, or talking or they woke up one morning and had been unable to open their jaws usually [12]. In the present research among 100 complete dentures wearing patients 14% experienced mild tinnitus and 15% experienced moderate tinnitus which interfered with their sleep whereas in a research conducted by Vernon et al. out of 1002 patients registered in the group only 69 patients had symptoms consistent with TMJ dysfunction. Regrettably, they were unable to find any single trait or set of attributes of tinnitus which exclusively indicated TMJ involvement [13].
Kurita et al. conducted a research which studied the relationship between score of chewing ability and other sign and symptoms analyzed by multiple regression analysis. Score of chewing ability correlated significantly with TMJ pain and mouth opening capacity of the patient [14]. This is similar to the present research which states that among 100 complete denture wearing patients 28(28%) showed mild pain/discomfort, 18 (18%) showed moderate pain/discomfort and couldn’t eat much of anything. 3(3%) showed severe pain/discomfort and could only eat soft food.
Wright et al. conducted a research on fifteen patients. Eight males and seven females participated in that study. Their ages ranged from 43 to 74 years, with a mean age of 57.6years. 11 out of 15 patients reported dizziness. All 15 patients met the diagnostic criteria for TMD [15]. Contrary to this in the present study, among 100 participating patients, there were 66(66%) patients who didn’t experience dizziness. 20(14%) experienced dizziness, but it did not interfere with daily activities. 8(8%) experienced dizziness which interfered somewhat with daily activities. 5(5%) experienced dizziness which caused a marked impairment in the performance of daily activities. 1 (1%) experienced dizziness which was incapacitating.
Conclusion
It is concluded that frequency and level of disability was variable from minimal to moderate among patients wearing full dentures. Many of the full denture wearing patients experienced more than one clinical symptoms of temporomandibular joint disability.
26660
References
- Burt NM, Semple D, Waterhouse K, Lovell NC (2013) Identification and interpretation of joint disease in paleopathology and forensic anthropology: Charles C Thomas Publisher.
- Saoemes R, Williams P, Bannister L, Berry M, Collins P, et al. (1999) Gray’s Anatomy in: Skeletal system. Churchill Livingstone, Edinburgh, London, pp: 555-560.
- Alomar X, Medrano J, Cabratosa J, Clavero J, Lorente M, et al. (2007) Anatomy of the temporomandibular joint. Semin Ultrasound CT MR 28: 170-183.
- Yap A, Tan K, Hoe J, Yap R, Jaffar J (2001) On‐line computerized diagnosis of pain‐related disability and psychological status of TMD patients: a pilot study. Journal of oral rehabilitation 28: 78-87.
- Choy E, Smith DE (1980) The prevalence of temporomandibular joint disturbances in complete denture patients. Journal of oral rehabilitation 7: 331-352.
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, et al. (2014) Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache 28: 6-27.
- Carlsson GE (1976) Symptoms of mandibular dysfunction in complete denture wearers. Journal of dentistry 4: 265-270.
- Patnaik V, Bala S, Singla R (2000) Anatomy of temporomandibular joint? A review. J Anat Soc India 49: 191-197.
- Mehrotra D (2013) Temporomandibular disorders. J Oral Biol Craniofac Res 3: 111.
- Steigerwald DP (1997) The Steigerwald/Maher TMD disability questionnaire. Today’s Chiropractic 26: 86-91.
- Frederikson H (2015) Intra-oral osteopathic technique for chronic temporomandibular disorders.
- Farrar WB (1972) Differentiation of temporomandibular joint dysfunction to simplify treatment. Journal of Prosthetic Dentistry 28: 629-636.
- Vernon J, Griest S, Press L (1992) Attributes of tinnitus associated with the temporomandibular joint syndrome. European archives of oto-rhino-laryngology 249: 93-94.
- Kurita H, Ohtsuka A, Kurashina Ka, Kopp S (2001) Chewing ability as a parameter for evaluating the disability of patients with temporomandibular disorders. Journal of Oral Rehabilitation 28: 463-465.
- Wright EF, Syms III CA, Bifano SL (2000) Tinnitus, dizziness, and nonotologic otalgia improvement through temporomandibular disorder therapy. Military medicine 165: 733-736.