Fotos V Nikolaos1*, Elefsiniotis S Ioannis1, Giakoumidakis Konstantinos2, Argyropoulos Evangelos3, Patris Vasileios4 and Brokalaki Hero1
1Faculty of Nursing, National and Kapodistrian University of Athens, Greece
2Cardiac Surgery Intensive Care Unit, “Evangelismos” General Hospital of Athens, Greece
3Pathologist, “Agioi Anargyroi” General Oncology Hospital of Athens, Greece
4Cardiac Surgeon, Cardiothoracic department, Liverpool Heart And Chest Hospital, Liverpool, United Kingdom
- *Corresponding Author:
- Nikolaos V. Fotos RN, MSc, PhD.
Lecturer, Faculty of Nursing
National and Kapodistrian University of Athens
Greece, 123 Papadiamantopoulou Street
Goudi, 115.27, Athens, Greece
Tel: 0030-210-7461454
Fax: 0030-210-7461476
E-mail: nikfotos@nurs.uoa.gr
Keywords
HBV; HCV; Hepatocellular carcinoma; Predisposing factors; Viral Hepatitis
Introduction
Chronic viral hepatitis is a major health problem worldwide. It is a chronic inflammation of the liver parenchyma caused by hepatitis B virus (HBV) or hepatitis C virus (HCV). Almost two billion people are infected with HBV worldwide, while the number of virus vectors is estimated at over 360 million. Infection with HBV is the tenth leading cause of death worldwide and causes more than 600,000 deaths each year [1]. Prevalence of chronic HBV infection in Greece ranges from 0.41% to 0.85% in voluntary blood donors and reaches 22% in immigrants from Albania [2].
It is also estimated that 170-200 million people worldwide are infected with HCV, while each year 3-4 million people are newly diagnosed while HCV is responsible for 350,000 deaths per year [3] In Greece the exact prevalence of HCV infection is unknown and it is believed that 2% of the general population suffers from chronic HCV infection, with a geographical distribution of 0.5% to 7.5%. [4].
Chronic viral hepatitis is a major causative factor for the development of hepatocellular carcinoma (HCC), the fifth most common cancer worldwide and the second most common cause of death from neoplasmic disease. Specifically, each year 250,000 to 1,000,000 deaths are caused by HCC worldwide [5]. Chronic hepatitis B (CHB) accounts for 50% of all HCC cases and chronic hepatitis C (CHC) for 25% of them [6]. Literature suggests that male subjects, chronic alcohol consumption, obesity, and diabetes mellitus (DM) are among the main predisposing factors of HCC [7-20].
In a country with poor epidemiological registry, the purpose of the present study was to estimate the frequency of HCC in patients with chronic viral hepatitis, and separately in patients with CHB and in those with CHC. Also, we attempted to highlight the predisposing factors of HCC in these patients. The importance of this study lies in the fact that in Greece there are significant deficits in epidemiological data that will allow the design and implementation of a long-term strategy to prevent HCC, especially in patients with chronic viral hepatitis.
Methods
Study design and participants
A retrospective descriptive epidemiological study was conducted. The inclusion criteria were: age ≥ 18 years old and certified diagnosis of infection (detection of antibodies against HBV or HCV, determination of HBV-DNA or HCV-RNA). Patients with HBV/HCV co-infection and/or co-infection with the human immunodeficiency virus (HIV) were excluded from the study, because in those patients it is difficult to correlate the development of hepatocellular carcinoma with the presence of HBV or HCV.
Our study population consisted of 574 patients with chronic viral hepatitis (CHB or CHC), who were examined over a seven year period (from 1 January 2007 to 31 September 2013) in the Hepatology outpatient unit of a General Hospital of Athens - Greece. Five hundred and forty nine out of 574 (95.6%) patients met the inclusion criteria and constituted our final study sample.
Data collection
Data collection was conducted in January 2013 by a single member of the research team, who obtained the data based on patient records review, using a short data collection form which was created by the research team specifically for the needs of the present study.
Ethical issues
The present study was approved by the medical ethics committee of the hospital. The study complied with all ethical principles set by the Declaration of Helsinki. The methods of the study were restricted to recording and analysing patient data related to our study aim.
Statistical analysis
All variables were categorical and are presented as absolute and relative frequencies. After descriptive statistical analysis, followed bivariate statistical analysis (Pearson’s chi-square test) to identify the differences between categorical variables and the presence of HCC. P values of less than 0.05 were considered significant. Analysis was performed using the PASW Statistics software.
Results
The study reviewed 549 patient files with chronic viral hepatitis. Almost half, 253 (46%) patients were diagnosed with chronic HBV infection, while 296 (54%) with chronic HCV infection.
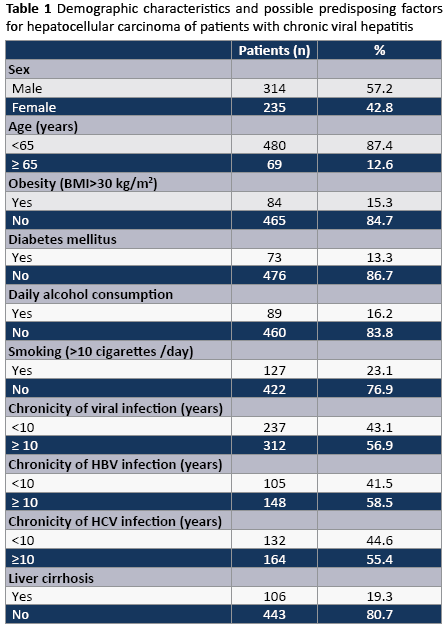
Table 1 provides the demographic patient characteristics and the frequency of possible risk factors for HCC. There were more men than women (57.2% vs. 42.8%), while the majority of study participants (87.4%) were aged less than 65 years. The 15.3 % of patients were obese (BMI>30 kg/m2) and 73 (13.3%) were diagnosed with DM. The daily intake of alcohol was reported by 89 (16.2%) patients, while one out of four (23.1%) smoked more than ten cigarettes per day. More than half (312, 56.9%) were diagnosed with chronic viral hepatitis for more than 10 years. Of these, 148 and 164 patients had CHB and CHC respectively. Also, 106 (19.3%) patients were diagnosed with cirrhosis of the liver.
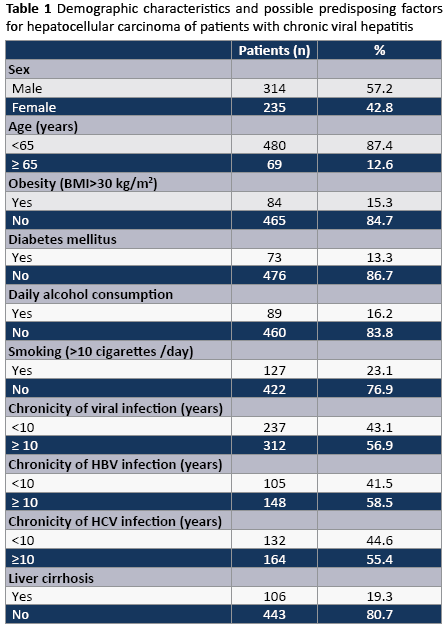
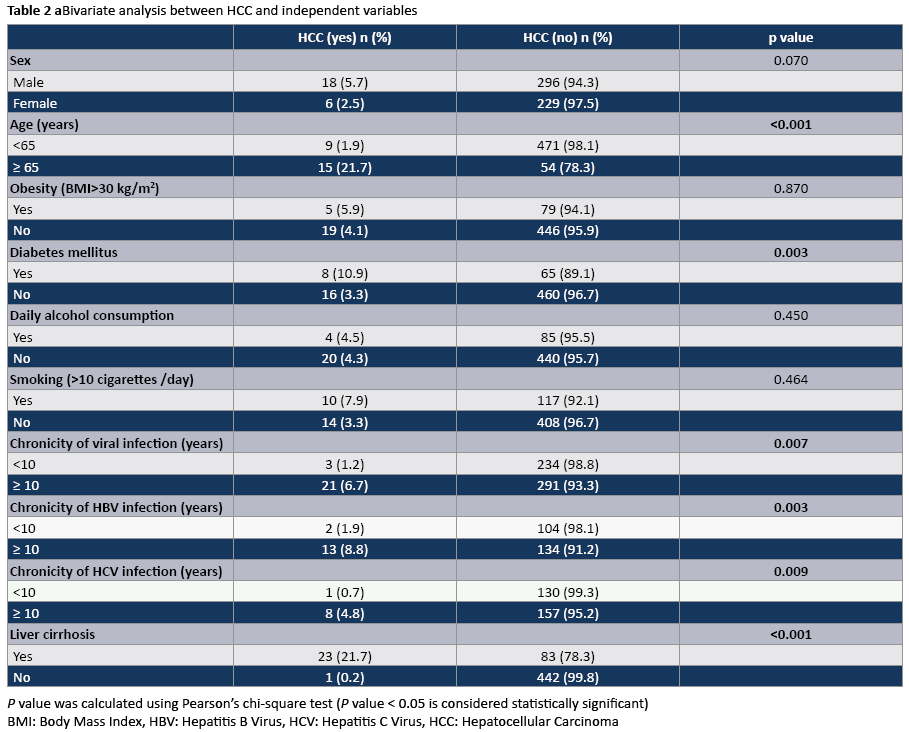
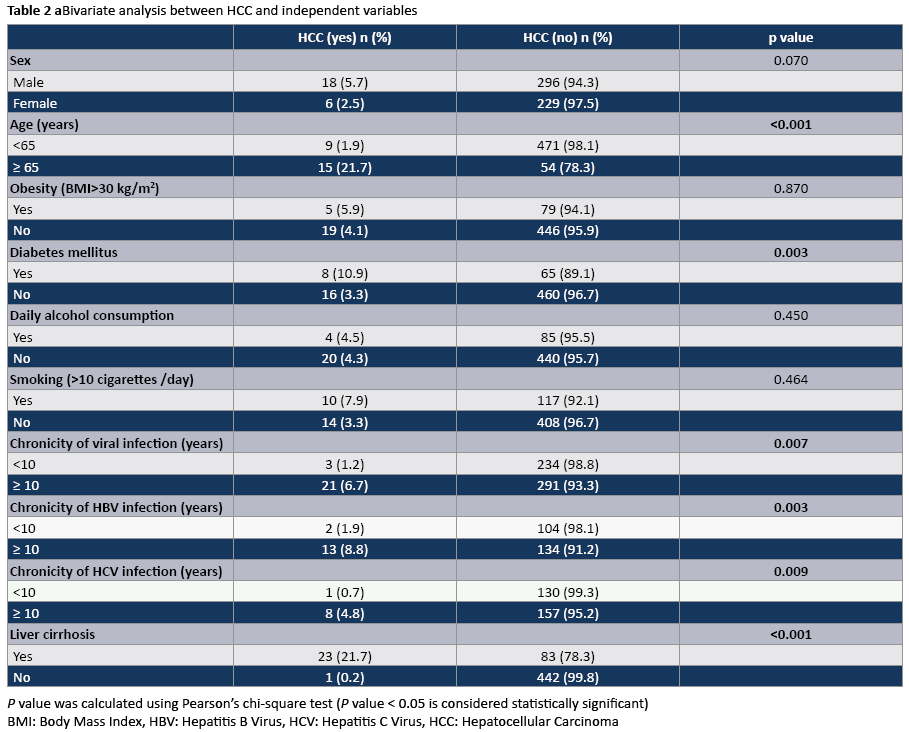
Table 2 summarizes the results of the statistical bivariate analysis between variables of Table 1 (independent variables) and the occurrence of HCC to patients of the study. HCC found to be more frequent in patients with age ≥ 65 years (P<0.001), patients with diabetes mellitus (P=0.003), those with chronicity of viral infection ≥ 10 years (P=0.007) and those with liver cirrhosis (P<0.001). Also HCC was more frequent in males, obese patients (BMI>30 kg/m2), those with daily alcohol consumption and the cigarette smokers, but not with statistical significancy.
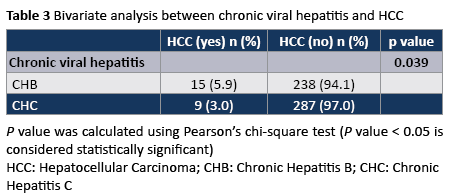
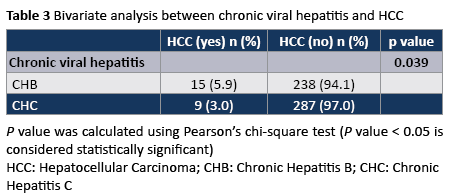
HCC was detected in 24 of 549 patients (4.4%). As shown in Table 3, 15 of the 253 patients with CHB (5.9%) and nine of 296 patients with CHC (3.0%) developed HCC (P=0.039).
Discussion
HCC is a major health problem worldwide. The relationship of chronic viral hepatitis with the pathophysiology of HCC is well known. However, according to the international literature, there are factors other than the infection by HBV and HCV, which have been associated with the occurrence of HCC [7,20]. Our study was conducted in order to detect these factors. We found that age ≥ 65 years, presence of DM, chronicity (≥ 10 years) of infection and liver cirrhosis were associated with the occurrence of HCC in patients with chronic viral hepatitis.
In addition, our data analysis confirmed the significantly higher prevalence of HCC among CHB patients compared to patients suffered from CHC. This association indicates the strong mutagenic activity of HBV in the liver. HBV is a DNA-virus, whose genome is combined with DNA of hepatic cells during the long stay of the virus in liver parenchyma, leading to various mutations in the genetic material of infected hepatic cells [21,22]. Moreover, the perinatal transmission of HBV is more common than that of HCV, resulting in the existence of HBV on liver parenchyma for more years [22]. In our study, this finding was verified, and a higher proportion of CHB patients had the disease for more than ten years than those who suffered from CHC (58.5% vs. 55.4%).
The age of patients proved to be a strong predisposing factor for the development of HCC in the present study. This obviously relates with the greater length of time the virus (HBV or HCV) stays inside liver parenchyma in people older than 65 years against younger individuals. As highlighted by Walter et al., [7] in their study the incidence of HCC is significantly increasing over the years, with a higher incidence between the ages of 60-70 years.
Moreover, El-Serag et al., [15] indicated a strong association between DM and HCC, regardless of the existence of other predisposing factors. A meta-analysis by Yang et al., [16] suggested that individuals with DM not only suffer frequently from HCC, but they have a higher mortality from HCC, compared with individuals who do not have DM. Wang et al. [19] in a systematic review and meta-analysis found a high prevalence of HCC in individuals with DM and also indicated the effect of antidiabetic medication in the development of HCC. More specifically, they found that metformin has a potential protective action while the sulphonylureas and insulin associated with the occurrence of HCC. In contrast, Singh et al., [17] found no relationship between antidiabetic agents and the occurrence of HCC.
Chronicity of viral infection by HBV or HCV was another predisposing factor for the development of HCC in patients of this study. For both total population and subpopulations of patients with CHB and CHC, patients with known infection for more than ten years had a higher prevalence of HCC, compared with those who have the disease for less than ten years. As in the case of the older age (≥ 65 years), HB and HC viruses causes significant damage to the liver parenchyma over the years, which may gradually lead to the development of HCC. It is well known that liver carcinogenesis in individuals with chronic viral hepatitis requires long stay of viruses in liver parenchyma [22].
Liver cirrhosis has proved to be a predisposing factor for the development of HCC, according to the results of our study. It is noteworthy that one in five patients (21.7%) with liver cirrhosis developed HCC compared to only one patient (0.2%) without liver cirrhosis. Many other researchers are in line with this finding. Walter et al., [7] in their research found that liver cirrhosis is the strongest predisposing factor for development of HCC. Also, results found by the studies of Yu et al., [23] and Chu et al., [24] demonstrated the association between liver cirrhosis and HCC.
Finally, in contrary to the findings of our study chronic alcohol consumption has been strongly associated with the occurrence of HCC [7,10,14]. In addition, several studies have highlighted the causal relationship between smoking and HCC [25-27].
Limitations
Our study included only patients with chronic viral hepatitis who were examined at a single Hepatology outpatient unit of a General Hospital of Athens-Greece. The sample size (n=549) was rather small for a period of 7 years and does not allow us to generalize the results of this study to the general population of Greece. Also, our study was retrospective and based on the records of one Hepatology outpatient unit in Athens. We recommend the future conduction of a prospective multicenter study, which will allow the collection of data from a larger population. The data collection from many centers, some of them out of Athens, will allow the generalization of study results for the Greek population.
Conclusions
This study was conducted in a population of patients with chronic viral hepatitis, aiming to indicate the prevalence of HCC among them and to highlight the predisposing factors for HCC. Age ≥ 65 years, DM, chronicity of infection and liver cirrhosis are the main predisposing factors of HCC in these patients. The health professionals, who are involved in the prevention of HCC, should consider these factors. Early diagnosis of DM and the successful regulation of blood glucose levels, mainly through non-medication measures could contribute on reducing the incidence of HCC. Also, both early diagnosis of viral hepatitis and the application of appropriate therapy could reduce the long-term effect of virus on liver parenchyma, which causes the generation of HCC.
3802
References
- Franco E, Bagnato B, Marino MG, Meleleo C, Serino L, et al. (2012) Hepatitis B: Epidemiology and prevention in developing countries. World J Hepatol 4: 74-80.
- Stefos A, Gatselis N, Zachou K, Rigopoulou E, Hadjichristodoulou C, et al. (2009) Descriptive epidemiology of chronic hepatitis B by using data from a hepatitis registry in Central Greece. Eur J Intern Med 20: 35-43.
- Zaltron S, Spinetti A, Biasi L, Baiguera C, Castelli F (2012) Chronic HCV infection: epidemiological and clinical relevance. BMC Infect Dis 12 Suppl 2: S2.
- Raptopoulou M, Touloumi G, Tzourmakliotis D, Nikolopoulou G, Dimopoulou M, et al. (2011) Significant epidemiological changes in chronic hepatitis C infection: results of the nationwide HEPNET-GREECE cohort study. Hippokratia 15: 26-31.
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61: 69-90.
- Sanyal AJ, Yoon SK, Lencioni R (2010) The etiology of hepatocellular carcinoma and consequences for treatment. Oncologist 15 Suppl 4: 14-22.
- Walter SR, Thein HH, Gidding HF, Amin J, Law MG, et al. (2011) Risk factors for hepatocellular carcinoma in a cohort infected with hepatitis B or C. J Gastroenterol Hepatol 26: 1757-1764.
- Huang YT, Jen CL, Yang HI, Lee MH, Su J, et al. (2011) Lifetime risk and sex difference of hepatocellular carcinoma among patients with chronic hepatitis B and C. J Clin Oncol 29: 3643-3650.
- Yeh SH, Chen PJ (2010) Gender disparity of hepatocellular carcinoma: the roles of sex hormones. Oncology 78 Suppl 1: 172-179.
- Yang JD, Harmsen WS, Slettedahl SW, Chaiteerakij R, Enders FT, et al. (2011) Factors that affect risk for hepatocellular carcinoma and effects of surveillance. Clin Gastroenterol Hepatol 9: 617-623.
- Polesel J, Zucchetto A, Montella M, Dal Maso L, Crispo A, et al. (2009) The impact of obesity and diabetes mellitus on the risk of hepatocellular carcinoma. Ann Oncol 20: 353-357.
- Ohki T, Tateishi R, Sato T, Masuzaki R, Imamura J, et al. (2008) Obesity is an independent risk factor for hepatocellular carcinoma development in chronic hepatitis C patients. Clin Gastroenterol Hepatol 6: 459-464.
- Saunders D, Seidel D, Allison M, Lyratzopoulos G (2010) Systematic review: the association between obesity and hepatocellular carcinoma - epidemiological evidence. Aliment Pharmacol Ther 31: 1051-1063.
- Loomba R, Yang HI, Su J, Brenner D, Barrett-Connor E, et al. (2013) Synergism between obesity and alcohol in increasing the risk of hepatocellular carcinoma: a prospective cohort study. Am J Epidemiol 177: 333-342.
- El-Serag HB, Tran T, Everhart JE (2004) Diabetes increases the risk of chronic liver disease and hepatocellular carcinoma. Gastroenterology 126: 460-468.
- Yang WS, Va P, Bray F, Gao S, Gao J, et al. (2011) The role of pre-existing diabetes mellitus on hepatocellular carcinoma occurrence and prognosis: a meta-analysis of prospective cohort studies. PLoS One 6: e27326.
- Singh S, Singh PP, Singh AG, Murad MH, Sanchez W (2013) Anti-diabetic medications and the risk of hepatocellular cancer: a systematic review and meta-analysis. Am J Gastroenterol 108: 881-891.
- Arase Y, Kobayashi M, Suzuki F, Suzuki Y, Kawamura Y, et al. (2013) Effect of type 2 diabetes on risk for malignancies includes hepatocellular carcinoma in chronic hepatitis C. Hepatology 57: 964-973.
- Wang P, Kang D, Cao W, Wang Y, Liu Z (2012) Diabetes mellitus and risk of hepatocellular carcinoma: a systematic review and meta-analysis. Diabetes Metab Res Rev 28: 109-122.
- Wang C, Wang X, Gong G, Ben Q, Qiu W, et al. (2012) Increased risk of hepatocellular carcinoma in patients with diabetes mellitus: a systematic review and meta-analysis of cohort studies. Int J Cancer 130: 1639-1648.
- Lee JH, Han KH, Lee JM, Park JH, Kim HS (2011) Impact of hepatitis B virus (HBV) x gene mutations on hepatocellular carcinoma development in chronic HBV infection. Clin Vaccine Immunol 18: 914-921.
- Thomas HC, Lok ASF, Locarnini SA, Zuckerman AJ (2013) Viral hepatitis. (4thedn), John Wiley & Sons, USA.
- Yu MW, Hsu FC, Sheen IS, Chu CM, Lin DY, et al. (1997) Prospective study of hepatocellular carcinoma and liver cirrhosis in asymptomatic chronic hepatitis B virus carriers. Am J Epidemiol 145: 1039-1047.
- Chu CM (2000) Natural history of chronic hepatitis B virus infection in adults with emphasis on the occurrence of cirrhosis and hepatocellular carcinoma. J Gastroenterol Hepatol 15 Suppl: E25-30.
- Hassan MM, Spitz MR, Thomas MB, El-Deeb AS, Glover KY, et al. (2008) Effect of different types of smoking and synergism with hepatitis C virus on risk of hepatocellular carcinoma in American men and women: case-control study. Int J Cancer 123: 1883-1891.
- Sherman M, Llovet JM (2011) Smoking, hepatitis B virus infection, and development of hepatocellular carcinoma. J Natl Cancer Inst 103: 1642-1643.
- Koh WP, Robien K, Wang R, Govindarajan S, Yuan JM, et al. (2011) Smoking as an independent risk factor for hepatocellular carcinoma: the Singapore Chinese Health Study. Br J Cancer 105: 1430-1435.