Keywords
Quality of life, hospitalization, ADL, elderly people, resident assessment instrument
Introduction
In health care, quality of life (QoL) has come to be an important concept and outcome measure as well as one of the main goals in medical care (Nordenfelt, 1991). It is agreed to be a broad framework which includes physical, social, psychological/emotional and spiritual life (Muldoon, Barger, Flory, & Manuck, 1998). Health?related quality of life is said to be a worldwide picture of health and well?being from a particular person’s perspective. The term “quality of life”, like health, has various meanings and no distinct definition (Sullivan, Karlsson, & Taft, 2002). An important quality of life component from elderly people’s perspective is functional independence (Hellström & Hallberg, 2004). Functional status has been used to describe motor function, ability to perform ADL (activities of daily living) and the ability to perform IADL (instrumental activities of daily living) (Knight, 2000). As people grow old they may experience that their health deteriorates and that being old often involves functional decline (Bank, 1995). Quality of life and its relationship to basic and instrumental ADL decline in elderly populations with medical illnesses has been described in various studies. Hoffman, Mc Kenna, Cooke, and Tooth (2003) concluded that elderly stroke patients had poorer IADL and poorer QoL than young stroke patients. One study from the Netherlands reported that declined ADL and IADL were predictors of low quality of life in elderly patients with cardiac diseases (van Jaarsveld, Sanderman, Miedema, Ranchor, & Kempen, 2001).
Acute illnesses requiring hospitalization are common in elderly people. Predictors for decline in physical performance during hospitalization are incontinence, impaired vision, weight change, cognitive impairment, unsteadiness, delirium and mobility impairment (Winograd et al.,1997; Mahoney, Sager, & Jalaluddin; 1999; Marcantonio, Flacker, Michaels, & Resnick, 2000; Bo et al., 2003; Lindenberger et al., 2003). Elderly people’s inability to perform basic ADL activities also increases the risk of hospital readmission, nursing?home admission, deteriorating quality of life and death (Sager et al., 1996; Covinsky et al., 1998; van Jaarsveld et al., 2001; Chuang et al., 2003; Hoffman et al., 2003). Additionally, Bo et al. (2003) presented evidence that the prognosis of elderly patients hospitalized in medical care units depends not only on acute physiological impairments, but also on loss of functional independence. Sager et al. (1996) conducted a prospective study of 448 elderly patients to identify the risk of developing new inability to perform ADL activities after acute medical ailments and hospitalization. They identified three patient characteristics as independent predictors of functional decline: increasing age, low Mini?Mental Status Exam admission scores, and low preadmission IADL function.
Predictors of decline in IADL among elderly people have been sparsely studied. Shinkai et al. (2003) have described a history of hospitalization during the last year before the decline, poor chewing ability and advanced age as predictors. Other significant predictors of decline in IADL during hospitalization are poor hand?grip strength, poor intellectual activities and limited social roles (Ishizaki, Watanabe, Suzuki, Shibata, & Haga, 2000). A Swedish study highlighted that people in older age groups needed more help with IADL with regard to cleaning, financial matters, personal hygiene, and outdoor mobility compared with younger age groups. This need for assistance with IADLs was also associated with poor quality of life in elderly people (Hellström & Hallberg, 2004). In a longitudinal follow?up study, Keller and Potter (1994) evaluated an outpatient geriatric population. The authors found that IADL was the strongest predictor of survival.
During the first 48 hours of acute care Jónsson et al., (2006) reported that only about half of all information on functional status was documented. Since nurses provide a majority of the care required by elderly people in acute care settings, nurses need to understand more about elderly people’s functional issues. Data are needed to identify the occurrence of functional status in this patient population and how it relates with baseline function as well as subsequent function.
The overall aim of this study was to describe the functional status or the ability to perform ADL activities of the persons aged 75 and above who had been hospitalized in acute care and to investigate differences, if any, in the quality of life of those who performed ADL fully one year after hospitalization and those who did not. The following questions guided the data analysis:
What was the level of the performance of ADLs at baseline, admission, discharge and one year after discharge from hospital?
What was the level of the performance of IADLs at baseline, admission, discharge and one year after discharge from hospital?
Was there a significant difference in the quality of life of those who were able to perform ADLs and IADLs fully one year after discharge from hospital and those who were not?
Method
This study formed part of a larger Nordic study of identification of comorbidity and functional limitations in the elderly in acute care (Jónsson et al., 2006).
Sample
The sample of this study was 158 randomly selected patients, 75 years or older, admitted to a medical clinic in a hospital in the north of Sweden. Excluded were patients admitted for less than 24 hours, patients admitted to Intensive Care Units and patients who were critically ill or unstable at the time of the assessment. Out of the 158 patients, 75 consented to further participation and follow?up after one year. Forty?three of the158 patients (27 %) declined. Thirty?eight out of the 158, (24 %) died during the study. They did not differ from the others regarding age, sex, civil status or living conditions. Two patients could not be contacted for follow?up. Thus, the final sample consisted of 75 patients.
Data collection and measures
Initial assessment
The data were collected from May 2001 to January 2003. The patients were selected randomly from a numbered admission list the morning after admission to hospital. The patients were assessed by the Resident Assessment Instrument ? Acute Care (RAI?AC) (Carpenter et al., 2001). The overall goal of the RAI?AC is to measure physical function (ADLs and IADLs), cognition, bladder/bowel continence, communication/sensory pattern, pain, nutrition and oral status. Sociodemographics are also determined. We asked the participants about their dependence in eight basic ADLs: mobility in bed, transfer, locomotion, dressing, eating, toilet use, personal hygiene and bathing. To assess IADLs, participants were asked whether they had any difficulty to do their shopping and their housework, to manage money and medicine, to use the telephone, to prepare their own meals, and to go to places out of walking distance. Dependence in ADL and IADL was defined as the subject’s needing help from someone else or being unable to perform the activity. The patients assessed the RAI?AC instrument at hospital on three occasions; baseline (the 30 days prior to the acute incident), admission (the 24 hrs prior to admission to the unit), discharge (day 7 or 24 hrs prior to discharge). The evaluation takes about 30 to 45 minutes to make. The RAI?AC is tested empirically and reliability testing of the instrument has previously shown an overall agreement of 83% for the pre?hospitalization assessment items and 79% for the in?hospital assessment items. Average inter?assessor reliability Kappa values for the pre?hospital period items were 0.57 and 0.58 for the in?hospital period items (Carpenter et al., 2001).
Follow?up assessment
One year after discharge from hospital, information was once again obtained by means of the RAI?AC instrument. At this follow?up, quality of life was also assessed with the Short form Health Survey (SF?36). This is a health?related quality of life instrument, which was developed in the USA. It has been used in a number of countries (Ware & Sherbourne, 1992). The SF?36 is organized into two main dimensions of health: the Physical Health Dimension (SF?36 physical component summary (PCS)) and the Mental Health Dimension (SF?36 mental component summary (MCS)). These two main dimensions comprise eight sub?divisions representing eight aspects of health: Physical Functioning, Role?Physical, Bodily Pain, General Health, Vitality, Social Functioning, Role?Emotional and Mental Health. The first four make up the Physical Health sum index and the last four make up the Mental Health sum index. The scores in each area (PCS, MCS) are standardized to range between 0 (lowest QoL) and 100 (highest QoL). The SF?36 is a 36?item Likert type scale, which has been translated and tested on a general Swedish population.
Reliability values for internal consistency, as measured by Cronbach’s alpha, have ranged from 0.79 to 0.93 (Sullivan, Karlsson, & Ware, 1995). The follow?up interview was mainly performed in the respondent’s home. Information was obtained by the same interviewer
Ethics
The study was approved by the Ethics Committee of the Medical Faculty, Umeå University (No.01?072).
Data Analyses
Data were analysed by means of the Statistical Package for Social Sciences (SPSS; version 11, 5). Information elicited by the RAI?AC and the SF 36 assessment tool was examined by means of descriptive statistics (eg. frequencies and percentages). Function (ADLs and IADLs) responses were dichotomized into independent function and dependent function for the analysis. To determine differences in selected variables between those who had attained independent function and those who had not, the T?test was used. The total scores of PCS 36 and MCS 36 were used and divided into quartiles. The first quartile indicated low quality of life (PCS36: 26.4; MCS36: 52.2).
Participants’ clinical and sociodemographic characteristics were analysed descriptively with regard to frequency and percentage for categorical data and means, medians, standard deviation and confidence intervals for continuous data. A p?value of < 0.05 was considered statistically significant.
Results
Demographic and Clinical Characteristics
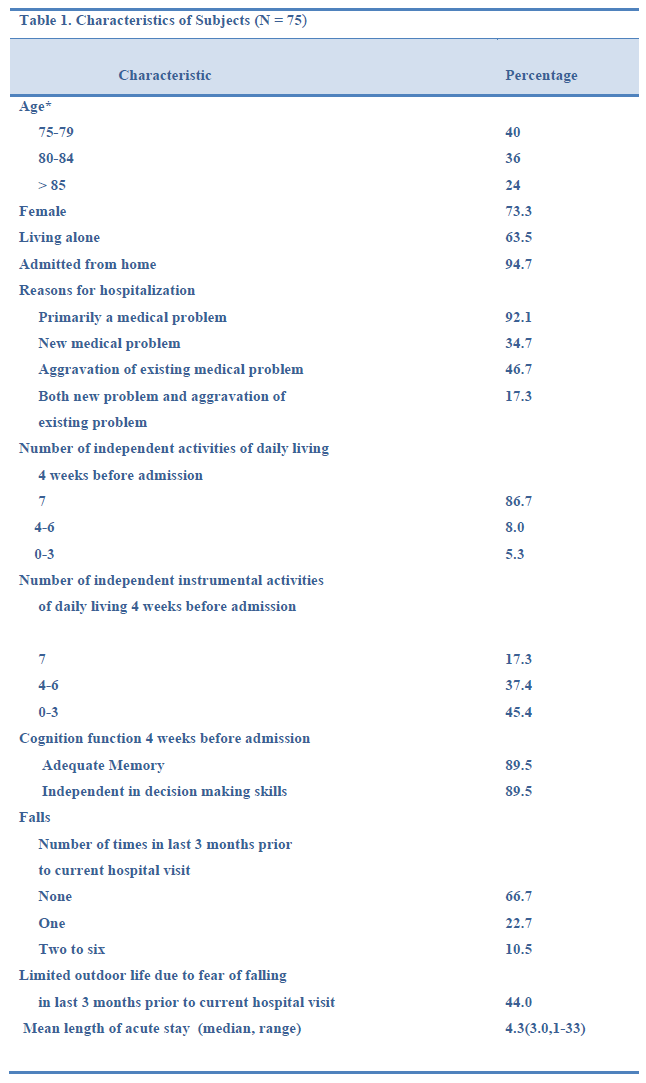
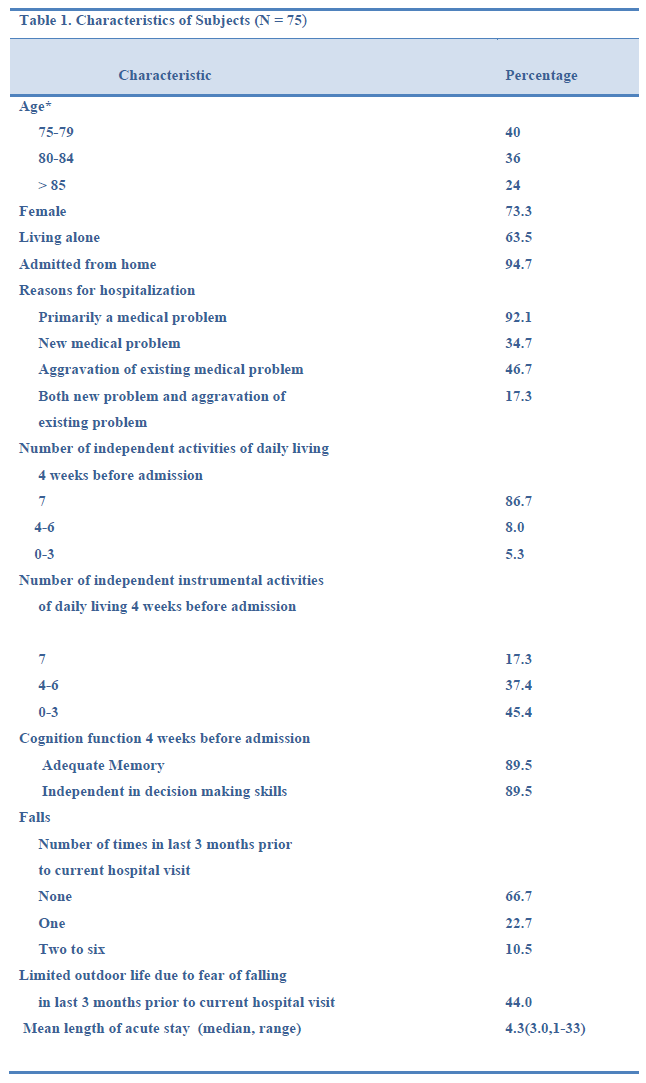
Seventy?five patients were included in this study. As shown in Table I, 73 per cent of them were women. Most of the patients were admitted to hospital from home and a majority (63.5%) of them lived alone. The reasons for hospitalization were primarily medical problems such as chest pain, a heart condition, angina pectoris, dizziness or urinary infection. The mean age of the patients was 81.5 (± 4.3 SD) years (range: 75?94) and the mean length of stay at hospital was 4.3 days.
Level of ADL Performance at Baseline, Admission, Discharge and one year after Discharge from Hospital
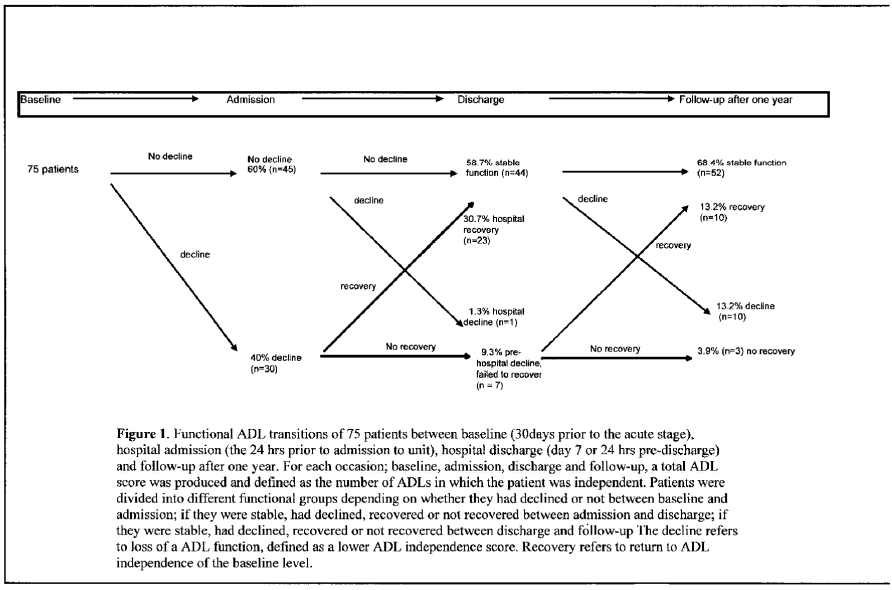
Between the baseline assessment (30 days before admission to hospital) and the assessment made after admission to hospital, 60 % of the 75 patients did not decline in ADL function. Still, 40 % of the patients declined between baseline and admission (independent in fewer ADLs on admission than at baseline). During hospitalisation, 31 % of the patients improved in ADL function. However, 9 % of the patients failed to recover in hospital (Figure 1).
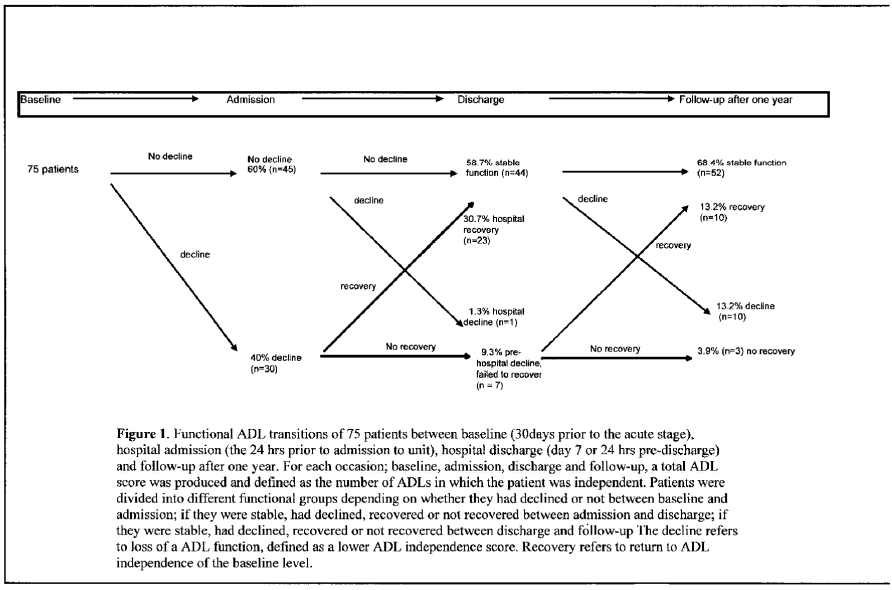
Figure 1: Functional ADL transitions of 75 patients between baseline (30days proirtothe acute stage), hospital admission (the 24 hrs proir to admission to unit), hospital discharge (day 7 or 24 hrs pre-discharge) and follow-up after one year. For each occasion; baseline, admission, discharge and folloe-up, a totlal ADl score was produced and defined as the number of ADLs in which the patient was independent. Patients were divided into different functional groups depending on whetherthey had declined or not between baseline and admission; if they were stable, had declined, recovered or not recovered between discharge and follow-up The decline refers to loss of a ADL function, defined as a lower ADl independence score. Recovery refers to return to ADL independence of the baseline level.
At the one?year follow?up, 68 % (n = 44) were stable in ADL function (return to ADL independence at baseline level). Some of the patients had declined in ADL function (13 %). Ten of the patients (13 %) reported recovery in ADL function. At the follow?up most of the patients reported that they were stable in ADL function (68%) (Figure 1).
Level of IADL Performance at Baseline, Admission, Discharge and one year after Discharge from Hospital
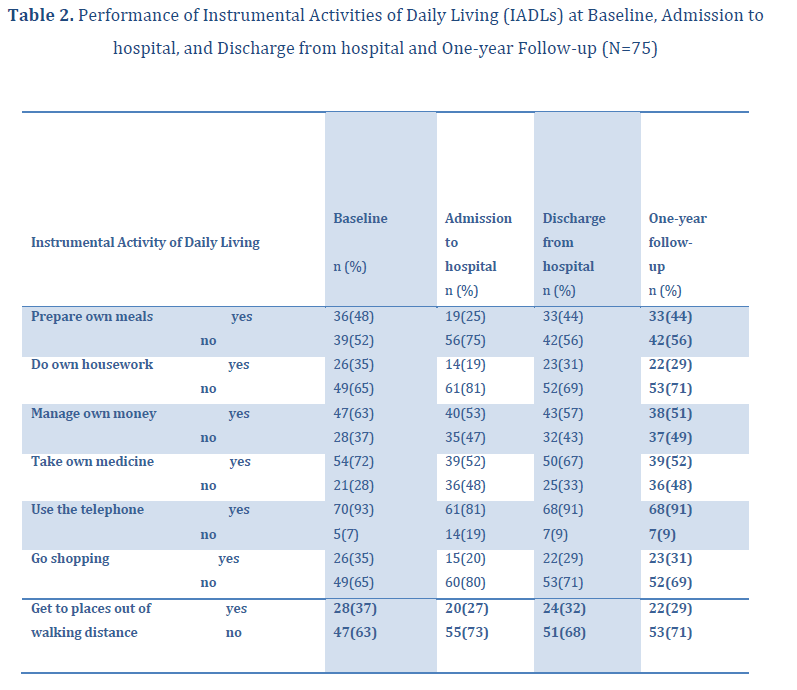
Only 17 % of the patients were completely independent in IADL four weeks before admission to hospital (Table 1). At admission to hospital, many of the patients had difficulties in performing many IADL activities on their own, i.e. do their own housework, go shopping, go to places out of walking distance and prepare their own meals (Table 2). At discharge from hospital, some of the patients had improved in IADL functions, for instance preparing their own meals, and doing their own housework. Many of them reported however, that many IADL activities were troublesome to manage without help. Seventy?one per cent (n = 53) could not go shopping independently, and 69 % (n = 52) could not do their own house work. Forty?two of them (56%) could not prepare their own meals and 32 (43 %) of them could not manage their own money at discharge from hospital.
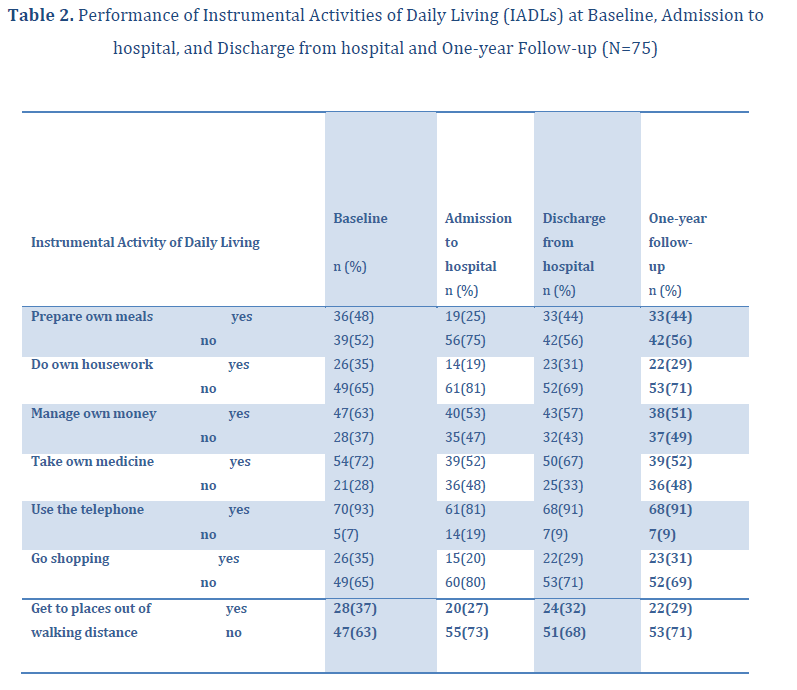
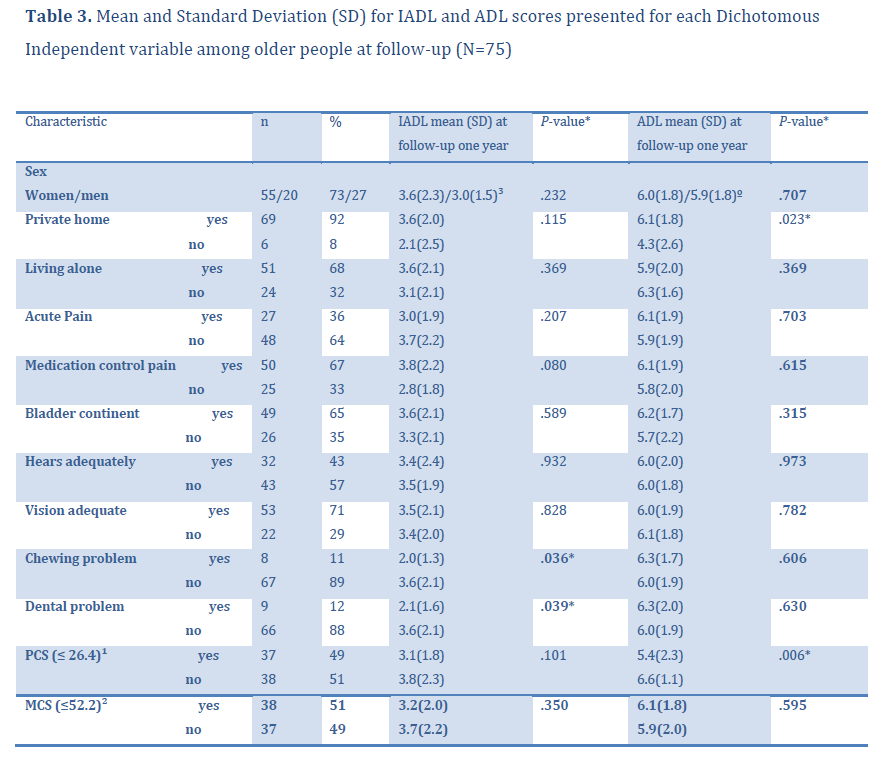
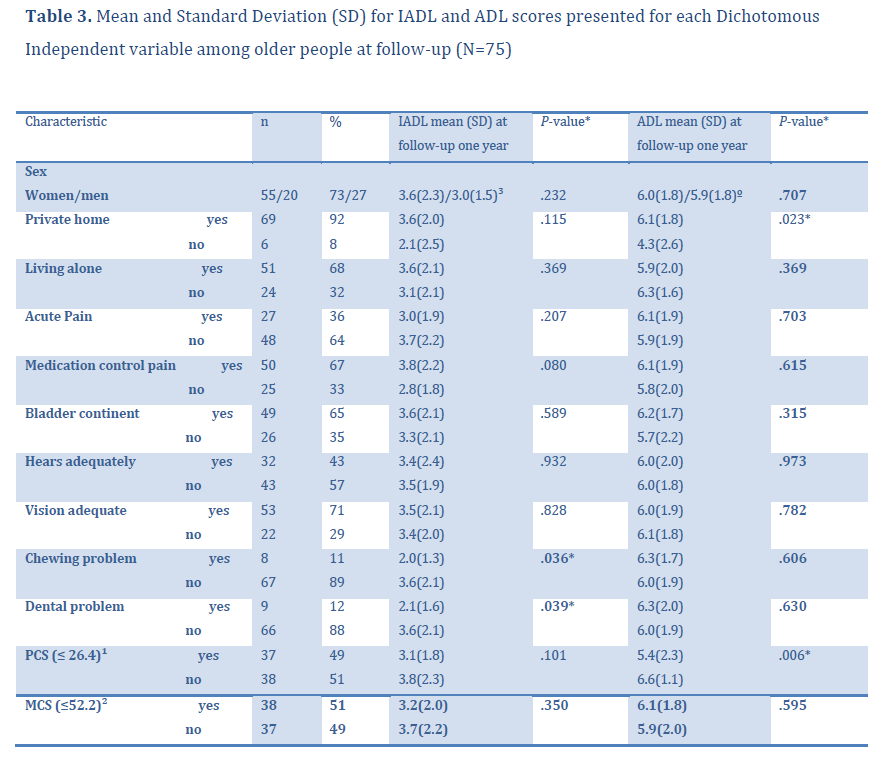
At the follow?up, a majority of the patients (71%) needed help with their housework and 53 % (n = 53) could not go to places out of walking distance without help. Furthermore, 69 % (n = 52) could not go for shopping without help (Table 2). At the one?year follow?up, patients with chewing problems reported a significantly lower IADL mean (2.0 vs 3.6 no chewing problem, p < 0.036) and patients with dental problems scored a lower IADL mean (2.1 vs 3.6 no dental problem, p < 0.039) (Table 3).
ADL Function and IADL Function one year after Discharge from Hospital and their relationship to Quality of Life
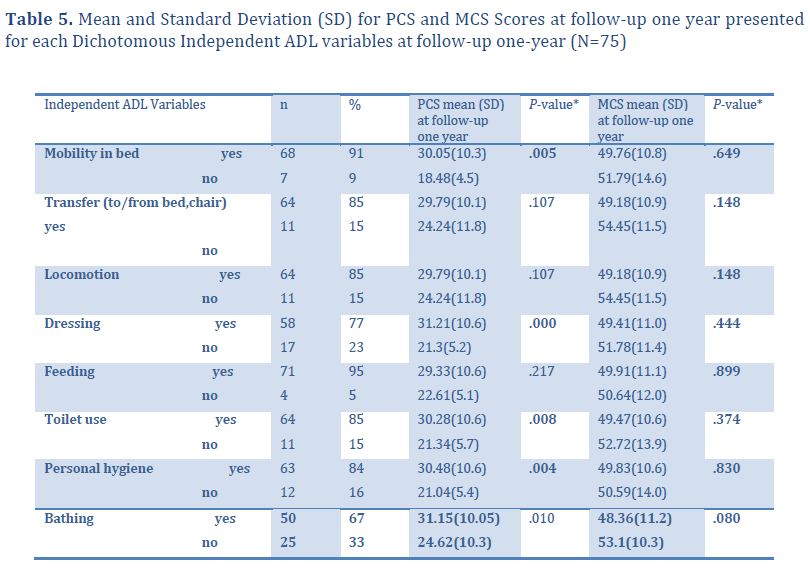
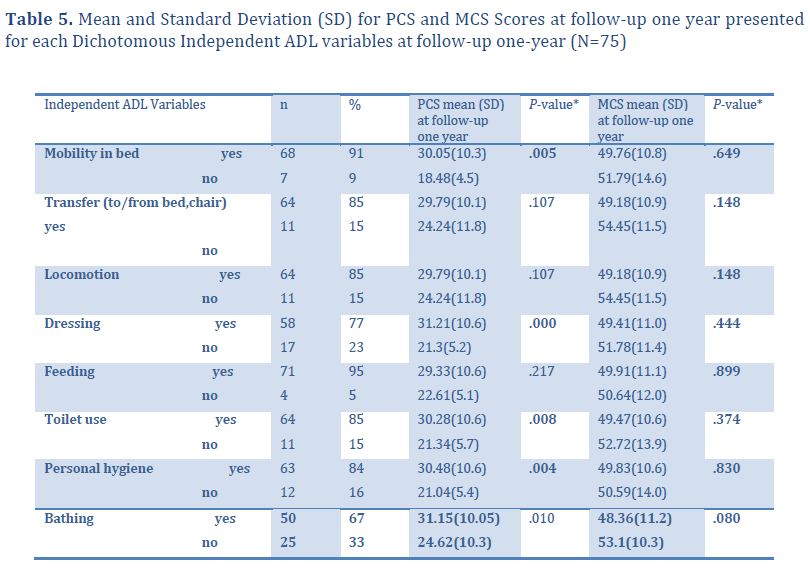
The ADL mean was 6.0 for women and 5.9 for men respectively at the follow?up. The respondent who reported a lower ADL mean (5.4 vs 6.6, p< 0.006) had a significantly lower physical health summary (PCS) (Table 3). The participant who reported a significantly lower PCS than the independent person (p<0.005 and p<0.000) were dependent in ADL activities such as mobility in bed and dressing. Dependency in toilet use, personal hygiene, and bathing was also significantly associated to low physical health summery. We found no significant differences between independence/dependence in ADL related to mental health summery (MCS). (Table 5).
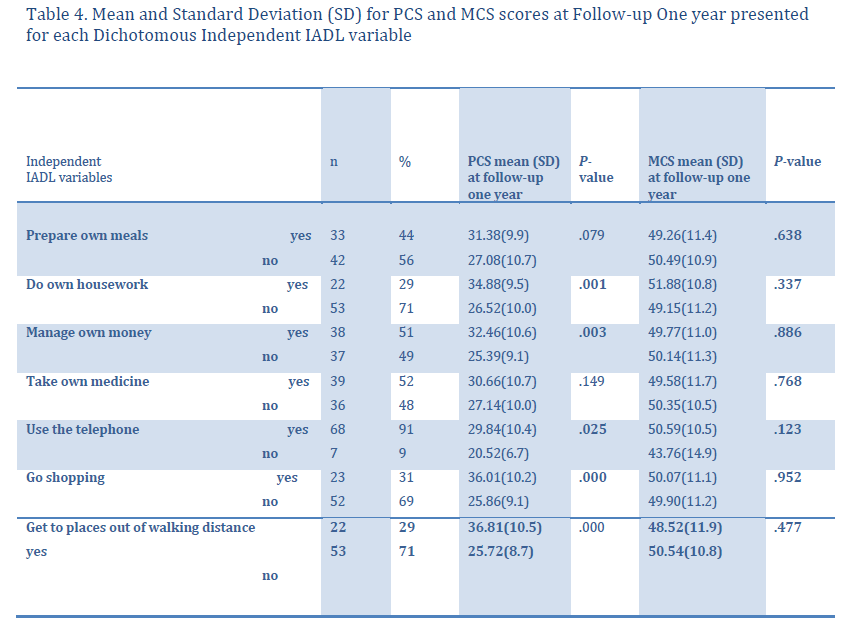
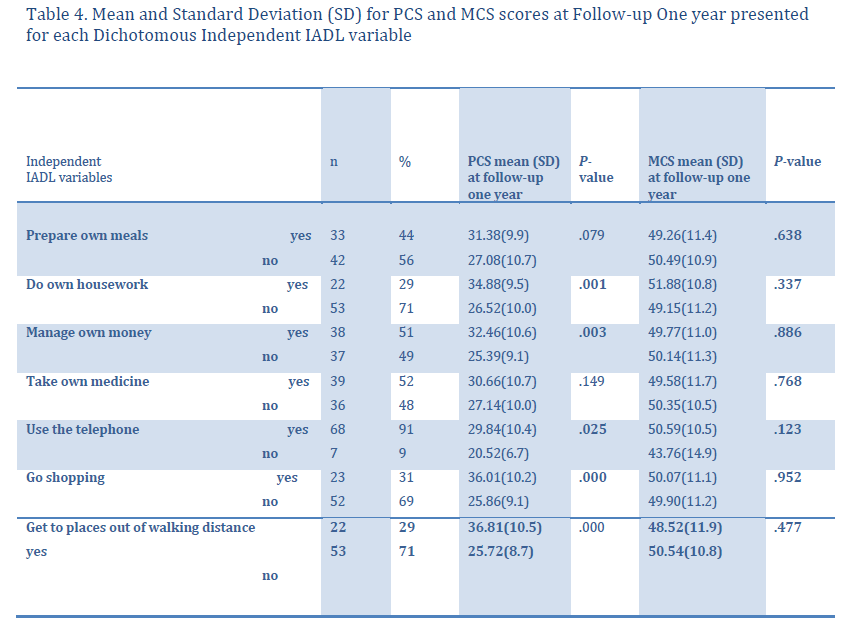
The IADL mean was 3.6 for women and 3.0 for men at the follow?up (Table 3). Patients who were dependent in IADL activities, for example to prepare their own meals and to do their own housework scored significantly lower in PCS than independent elderly patients (p<0.001 and p<0.003) (Table 4). Patients who reported that they were not able to go shopping or go to places out of walking distance reported a significantly lower PCS mean than independent patient. We found no significant differences between independence/dependence in IADL that related to the MCS (Table 4).
At the one?year follow?up, 69 (92 %) of the respondents lived in private homes and 51 (68%) lived alone. Respondents living in private homes reported a significantly higher ADL mean (6.1 vs 4.3, p<0.023) than patients who did not live in private homes. The IADL mean was 3.6 for those who lived in private homes compared to 2.1 for those who did not live in private homes, but no statistically significant difference was found. Thirty?six percent (n= 27) of the 75 elderly adults reported acute pain at follow?up and 33 % had no medication to control pain. Bladder incontinence problems were reported by 35 % of them (Table 3).
The mean physical health summary score (PCS) was 28.97(SD ± 10.53) at the follow?up one year after hospitalization. The mean mental health summary score (MCS) was 49.95 (SD ± 11.12).
Discussion
Functional ability is the ability to perform basic ADL activities without support. It is the key to overall independence and quality of life. Elderly adults may undergo substantial changes in function when hospitalized for acute medical illness. Changes in function, either improvement or deterioration, commonly occur during hospitalization. When caring for elderly adults it must be a primary task and a key role for nurses to improve function (Manandhar, 1995; Grill, Stucki, Boldt, Joisten & Swoboda, 2005). Data suggest that 31 % of the patients improved in ADL function during hospitalization. This result could be understood in terms of good hospital care; the nursing care provided at the medical ward was positive for the elderly since his/her ADL function improved and almost certainly enhanced his/her functional health status at the discharge from hospital.
However, caring for elderly people during hospitalization also includes observation of patients IADL functions. Our result disclosed that, at discharge from hospital many IADL activities were troublesome to manage, and the participant’s ability to perform many daily activities was reduced. One explanation could be the short length of stay in the hospital. In our study, the mean length of stay was only 4.3 days. Short hospitalization makes demands on nurses’ care planning. Many previous studies have identified a great deal of problems must be considered in the planning for the elderly people’s discharge from the hospital (Marks, 1994; Bull & Roberts, 2001). Elderly people hospitalised on acute care wards reported that they had not been asked about their home situation or how they should cope after leaving hospital. Many of the elderly were also unclear about what activities they could engage in, or what they should avoid (Marks, 1994; Bull & Roberts, 2001). We believe that the specific discharge planning process described by Bull & Roberts (2001) might be useful when elderly people’s discharge is planned. This process is characterized by four stages: getting to know the patient; initial plans for the discharge date; patient getting ready to go home and making the transition. In the first stage, the health care professionals asked questions about elderly person’s function, home environment and social support. The second stage included active involvement of the multidisciplinary team (MDT), for instance district nurses and health care professionals in the community. The third and fourth stages were characterized by ongoing involvement of the MDT team and the building of relationships with members of the community team. This type of discharge planning might have been useful for our patients in order to identify functional impairments during the short hospital stay. Several authors have suggested that good nursing care planning has several objectives; to identify specific patient problems, help the patient return to his best state of health, and evaluate the patient’s need for activity (Fuerst & Wolff, 1969; Björvell, Wredling, & Thorell?Ekstrand, 2002).
Another explanation for the reduction in functional activities at discharge could be the rehabilitation care in hospital. Grill et al., (2005) propose that the outcome of an acute medical illness depends not only on appropriate medical care but also on the recognition of the patient’s need for rehabilitation. Nurses play an important role in the recognition of patients’ rehabilitation needs since nurses meet the patient early in the acute care setting. Results from the Stucki, Stier?Jarmer, Grill, & Melvin study (2005) showed that it was very important to address elderly patients’ function early in the acute care setting because early recognition of rehabilitation needs can reduce healthcare costs and patient’s dependence.
The findings of this study showed that the IADL functions of the elderly were as troublesome at the one?year follow?up as at discharge from hospital. More than half of them (71 %) could not manage their own housework or go out to places out of walking distance by themselves. Inability to perform these tasks poses a threat to independent living. When linking IADL function to physical health (an indicator of quality of life) we found that the elderly who were dependent in IADL activities scored significantly lower in the physical health summary (PCS) than the independent elderly people. It is well known that the ability to move around in one’s own environment is a basic human function vital to independence and ADL activities. Other studies have shown that loss of mobility is a principal cause of limited quality of life and increases dependence in elderly people. Furthermore, independent personal care activities and self?care is of great importance to elderly people’s lives; it supports health, well?being and feelings of autonomy and dignity (Windle & Burholt, 2003, Sacco?Peterson & Borell, 2004).
The strengths and weakness of our study should be recognized. The strengths of our study include a diverse sample of hospitalized elderly patients who have been followed for one year. We have used validated questionnaires to assess functional status and quality of life. The data collection was made by the RAI?AC instrument which is built on self?reporting and comparison of data over time which gave a longitudinal picture of the patients’ functional status. We used trained registered nurses to collect the data. One limitation was that the SF 36 instrument was filled in only at the follow?up. The study would have been more complete if we had also followed up the patients’ quality of life over time instead of making this evaluation only at the follow?up. Another limitation of this study was the baseline assessment before admission to hospital. The baseline assessment was a recall. This may be a critical weakness of this study. Neither did the researchers control for all extraneous variables such as individual medication regimes, level of social support and disease complications that might influence the QoL.
The result showed significant associations between dependent ADL and IADL status and poor quality of life at one year. There is a reason to believe same is true on discharge. It is important that those who work with elderly people are aware of the negative effects dependent ADL and IADL status may have on the quality of life as it indicates how important it is to help them to reduce their dependence in functional status. The first step is recognition, the second would be action based on best evidence, either with rehabilitation or by putting supportive measures in.
Special thanks to:
Inter RAI for allowing us to use the RAI?AC instrument: www.InterRAI.org
The Nordic Council of Ministers for support to NordRAI, a Nordic network of professionals working with InterRAI instruments. We are also grateful to Britt?Inger Norberg, Ulla Britt Johansson and Mitzie Nordh, who where actively involved in the data collection.
3696
References
- Bank, S.P. (1995). Before the last leaves fall: sibling connections among the elderly. Journal of GeriatricnPsychiatry, 28, 183‐195.
- Björvell, C., Wredling, R., & Thorell‐Ekstrand., I (2002). Long‐term increase in quality of nursing documentation:neffects of a comprehensive intervention. Scandinavian Journal of Science, 16, 34‐42.
- Bo, M., Massaia, M., Raspo, S., Bosco, F., Cena, P., Molaschi, M., & Fabris, F. (2003). Predictive factors of inhospitalnmortality in older patients admitted to a medical intensive care unit. Journal of the American Geriatrics
- Bull, M.J., & Roberts, J. (2001). Components of a proper hospital discharge for elders. Journal of AdvancednNursing, 35(4), 571‐581.
- Carpenter, GI., Teare, GF., Steel, K., Berg, K., Murphy, K., Bjornson, J., Jonsson, PV., & Hirdes, JP. (2001). A newnassessment for elders admitted to acute care: reliability of the MDS‐AC. Aging‐Clinical & ExperimentalnResearch, 13(4), 316‐30.
- Chuang, KH., Covinsky, KE.,Sands, LP., Fortinsky, RH., Palmer, RM., & Landefeld, CS. (2003). Diagnosis‐relatedngroup‐adjusted hospital costs are higher in older medical patients with lower functional status. Journal of thenAmerican Geriatrics Society, 51(12), 1729‐34.
- Covinsky, KE., Palmer, RM., Kresevic, DM., Kahana, E., Counsell, SR., Fortinsky, RH., & Landefeld,‐C‐S. (1998).nImproving functional outcomes in older patients: lessons from an acute care for elders unit. Joint‐Commissionjournal‐ on‐quality‐improvement, Feb; 24(2), 63‐76.
- Fuerst, EV., & Wolff, L. (1969). Fundamentals of Nursing. 4th ed. Philadelphia, J.B. Lippincott Company.
- Grill, E., Stucki, G., Boldt, C., Joisten, S., & Swoboda, W. (2005). Identification of relevant ICF categories byngeriatric patients in an early post‐acute rehabilitation facility. Disability and Rehabilitation, 27(7/8), 467‐473.
- Hellström, Y. & Hallberg, I. (2004). Determinants and characteristics of help provision for elderly people livingnat home and in relation to quality of life. Scandinavian Journal of Caring Sciences, 18, 387‐395.
- Hoffman, T., Mc Kenna, K., Cooke, D. & Tooth, L. (2003). Outcomes after stroke: Basic and instrumentalnactivities of daily living, community reintegration and generic health status. Australian Occupational TherapynJournal, 225‐233.
- Ishizaki, T., Watanabe, S., Suzuki, T., Shibata, H,. & Haga, H. (2000). Predictors for functional decline among nondisablednolder Japanese living in a community during a 3 year follow‐up. Journal of the American Geriatrics
- van Jaarsveld, CHM., Sanderman, R., Miedema, I., Ranchor, AV., & Kempen, GIJM. (2001). Changes in healthnrelated quality of life in older patients with acute myocardial infarction or congestive heart failure. Journal of the American Geriatrics Society, 49 (8), 1052‐1058.
- Jónsson PV, Finne‐Soveri, H., Jensdóttir A.B., Ljunggren, G., Bucht, G., Grue E.V., Noro, A., Björnson, J., Jonsén, E., & Schroll, M. (2006). Co‐morbidity and functional limitation in older patients underreported in medical recordsnin Nordic Acute Care Hospitals when compared with the MDS‐AC instrument. Age and Ageing, 35(4), 434‐438.
- Keller, BK., & Potter, JF. (1994). Predictors of mortality in outpatient geriatric evaluation and management ofnclinic patients. Journal of Gerontology, Nov; 49(6), 246‐251.
- Knight, M M. (2000). Cognitive ability and functional status. Journal of Advanced Nursing, 31(6), 1459‐1469.
- Lindenberger, EC., Landefeld, CS., Sands, LP., Counsell, SR., Fortinsky, RH., Palmer, RM., Kresevic, DM& Covinsky, KE. (2003). Unsteadiness reported by older hospitalized patients predicts functional decline. Journalnof the American Geriatrics Society, May;51(5), 621‐626.
- Mahoney, JE., Sager, MA., & Jalaluddin, M. (1999).Use of an ambulation assistive device predicts functionalndecline associated with hospitalization. Journals of Gerontology A Biological Sciences and Medical Sciences, Feb;54(2),83‐88.
- Manandhar, MC. (1995). Functional ability and nutritional status of free‐living elderly people. Proceedings ofnthe Nutrition Society, 54, 677‐691.
- Marcantonio, ER., Flacker, JM., Michaels, M., & Resnick, NM. (2000). Delirium is independently associated withnpoor functional recovery after hip fracture. Journal of the American Geriatrics Society, Jun;48(6),618‐624.
- Marks, L. (1994). Seamless Care or Patchwork Quilt? Discharging Patients from Acute Hospital Care. London;nKing´s Fund Institute.
- Muldoon, M F., Barger, S D., Flory, J D., & Manuck, S B. (1998). What are quality of life measurementsnmeasuring? British Medical Journal, 316, 542‐545.
- Nordenfelt, L. (1991). Livskvalitet och hälsa. Teori och kritik. [Quality of life and Health. Theory and Criticism].nStockholm; Almquist & Wiksell. [In Swedish].
- Sacco‐Peterson, M & Borell, L. (2004). Struggles for autonomy in self‐care: the impact of the physical and socioculturalnenvironment in a long‐term care setting. Scandinavian Journal of Caring Sciences, 18(4), 376‐386.
- Sager, MA., Rudberg, MA., Jalaluddin, M., Franke, T., Inouye, SK., Landefeld, CS., Siebens, H,. & Winograd, CH.n(1996). Hospital admission risk profile (HARP): identifying older patients at risk for functional decline following acute medical illness and hospitalization. Journal of the American Geriatrics Society, Mar;44(3), 251‐ 257.
- Shinkai, S., Kumagai, S., Fujiwara, Y., Amano, H., Yoshida, Y., Watanabe, S., Ishizaki, T.,Suzuki, T., & Shibata, H.n(2003). Predictors for the onset of functional decline among initially non‐disabled older people living in a community during a 6‐years follow‐up. Geriatrics and Gerontology International, 3, 31‐39.
- Stucki, G., Stier‐Jarmer, M., Grill, E., & Melvin, J. (2005). Rationale and principles of early rehabilitation care afternan acute injury or illness. Disability and Rehabilitation, 27(7/8), 353‐359.
- Sullivan, M., Karlsson, J., & Ware, J. E., Jr. (1995). The Swedish SF‐36 health survey –Evaluation of data quality,nscaling assumptions, reliability and construct validity across general populations in Sweden. Social Science& Medicine, 41(10), 1349–1358.
- Sullivan, M., Karlsson, J. & Taft, C. (2002). SF 36 Hälsoenkät. Svensk manual och tolkningsguide.( SF36 Healthnquestionnaire. Swedish manual and interpretation guide)[In Swedish]. Health Care Research Unit, MedicalnFaculty, Göteborg; University and Sahlgrenska University Hospital, Göteborg, Sweden.
- Ware, J. E., JR., & Sherbourn, E. C. D. (1992). The MOS 36‐item short‐form health survey (SF‐36). Conceptualnframework and item selection. Medical Care, 30(6), 473–483.
- Windle, G., & Burholt, V. (2003).Older people in Wales, their transport and mobility: a literature review. Qualitynin Aging, 4(2), 28‐35.
- Winograd, CH., Lindenberger, EC., Chavez, CM., Mauricio, MP., Shi, H. & Bloch, DA. (1997). Identifyingnhospitalized older patients at varying risk for physical performance decline: a new approach. Journal of the American Geriatrics Society, May;45(5), 604‐609.