Review Article - (2022) Volume 0, Issue 0
Gianotti Crosti Syndrome and Its Relationship with Acral Rash- Pediatric Approach
Yalisa Consuegra Montes,
Freddy Fernando Fonseca Lopez,
Catherine Rosero Morales and
Laura Andrea Martinez Puello
General Physician, Universidad de los Andes, Bogotá, Colombia, Colombia
General Physician, Fundacion Universitaria Sanitas, Bogoto, Colombia
General Physician, Universidad Simón Bolívar, Barranquilla, Colombia
General Physician, Universidad del Norte, Barranquilla, Colombia
General Physician, Universidad Cooperativa de, Medellin, Colombia
General Physician, Fundacion Universitaria Sanitas, Bogota, Colombia
General Physician, Universidad Militar Nueva Granada, Bogota, Colombia
General Physician, Universidad de Ciencias Aplicadas y Ambientales, Bogota, Colombia
General Physician, Universidad del Sinu, Cartagena, Colombia
*Correspondence:
Laura Camila Garcia Medina, General Physician, Universidad de los Andes, Bogotá, Colombia,
Colombia,
Email:
Received: 11-Mar-2022, Manuscript No. Iphsj-22-12661;
Editor assigned: 13-Mar-2022, Pre QC No. Preqc No. Iphsj-22-12661(PQ);
Reviewed: 27-Mar-2022, QC No. QC No. Iphsj-22-12660;
Revised: 01-Apr-2022, Manuscript No. Iphsj-22-12661(R);
Published:
09-Apr-2022, DOI: 10.36648/1791-809X.16.S6.926
Abstract
The Gianotti-Crosti syndrome, also known as popular acrodermatitis of childhood, is a secondary to, especially viral or after immunization of the host immune response against infections frequently little dermatosis. Usually appear in the Pediatric population because these patients usually are brought to your paediatrician is critical knowledge of the characteristics of this syndrome and the close relationship it has with the acral rash, to the point where authors have proposed to use the term Gianotti�Crosti, regardless of their cause and presentation to describe all eruptive dermatosis location of acral syndrome. However, it is essential recognition of both concepts individually, their differences and similarities to perform a correct diagnosis and appropriate treatment applied as appropriate.
Keywords
Acropapulosis syndrome, Gianotti Crosti, Rash, Pediatrics, Dermatosis
Introduction
The Gianotti-Crosti syndrome (Sx GC), also known as Acropapulosis childhood or acrodermatitis child popular, is a rare and self-limited dermatosis presence of monomorphic skin lesions affecting children regardless of sex, from the six months to 12 years of age, although some authors propose intervals ranging from 3 months to 15 years old, but after studies confirm a global and significantly higher incidence between the first and sixth year of life, on the contrary, its appearance in adults is much more rare, with few cases reported in the literature. [1, 2]. Such pathology was first described by Fernando Gianotti and Agostino Crosti in Milan, Italy, in 1955, however, from that time until today, and with all the advances in the field of medicine pathogenesis remains unknown, although it has related to viral and bacterial infections, as well as immunization, in fact, initially the disease described as secondary to infection by hepatitis B; However, in recent years, other viral and bacterial agents and vaccine antigens, have been associated with this dermatosis as shown in Table 1 [3] .Actualmente, numerous studies confirm that VEB is the most common cause SGC, is therefore the most common cause of this dermatosis is considered viral additionally other viruses have been associated with the SGC, including hepatitis a, cytomegalovirus, herpes virus 6, coxsackie, rotavirus, parvovirus B19, molluscum contagious, HIV, respiratory syncytial virus, mumps virus and Para influenza virus 1 and 2. Bacteria as Bartonella henselae, Mycoplasma pneumonia, Streptococcus β hemolytic and Borrelia burgdorferi, have also been reported as potential causative agents in spite that there are few reported cases. In addition, also it described later SGC immunization with vaccines diphtheria, polio enter virus, tetanus, pertussis, hepatitis A and B, and anti-viral association measles, mumps and rubella, included in MMR [4, 5] (Table 1).
| Virus |
Bacterium |
| Epstein-Barr virus |
Bartonella henselae |
| Hepatitis A, B and C viruses |
Estreptococo β-hemolítico |
| Cytomegalovirus |
Borrelia burgdorferi |
| Herpes virus 6 |
Mycoplasma pneumoniae |
| Coxsackie A16, B4 and B5 |
- |
| Rotavirus |
- |
| Parvovirus B19 |
- |
| Molluscum contagiosum |
- |
| Respiratory syncytial virus |
- |
| Echo virus |
- |
| Para influenza |
- |
| HIV |
- |
Table 1. Aetiological infectious agents of infantile papular acrodermatitis.
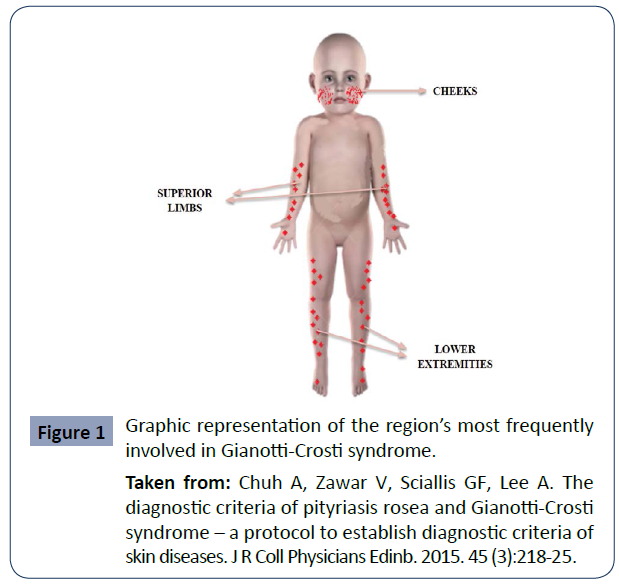
Like the pathogenesis, which is not completely precise, the pathophysiology of the syndrome, the incidence and prevalence are unknown even knowing that it has a worldwide distribution, however, there is underreporting, which makes it difficult to estimate its real prevalence and incidence. Although it is known that it is pathology without predilection for ethnicity or gender. However, given that patients can be diagnosed with a nonspecific viral exanthema, it is probably underdiagnosed. In fact, it is well known that this syndrome is somewhat difficult to diagnose due to poor knowledge. For this reason, authors have proposed criteria such as those observed in Table 2 and knowing that these patients are usually taken to their paediatrician, it is important that the clinician knows the fundamental characteristics of the syndrome; therefore, the clinical picture presents characteristics that are undoubtedly very valuable when giving the diagnosis. diagnosis, among these characteristics are low fever, asymptomatic and self-limited papulo-vesicular reaction with a symmetrical distribution on the face, more specifically on the cheeks, buttocks and extensor surfaces of the extremities as seen in Figure 1, forming plaques or remaining isolated, it rarely involves the palms, soles, flexor areas, and mucosa. The trunk is generally spared and the lesions are usually not pruritic [5-7] (Table 2).
| Inclusión signs for diagnosis |
Clinical signs of exclusión of the diagnosis |
| A- Of the rash |
B- From the skin biopsy (if it has been performed) |
A- Of the elementary lesions of the rash and its extensión |
B- Medical criteria or clinical judgment |
| 1. It should consist of monomorphic,brownish-pink papules or papulovesicles, with a flat surface, with a diameter of one to 10mm. |
1.Must offer compatible histopathology |
1.They should not be flaky |
1. You should not consider any of the differential diagnoses of CGS as more likely. |
| 2. It must affect at least three of the locations: cheeks, buttocks, dorsal aspect of the forearm, anterior aspect of the legs |
- |
2. They should not cover large areas of the trunk. |
- |
| 3.It must be symmetrical and have evolved in the 10 days |
- |
- |
- |
| Diagnostic criteria for CGS |
| I |
The patient, on at least one occasion, must meet all the clinical signs of inclusión, defined by a doctor. |
| II |
The histopathology, if a biopsy has been performed, must be compatible with SGC. |
| III |
The patient should never develop any of the exclusión signs, defined by a doctor |
| IV |
Medical criteria should not consider any of the GCS differential diagnoses as more likely. |
Table 2. Diagnostic criteria for Gianotti-Crosti syndrome or papular acrodermatitis of infancy, modified translation of Chuh A.
According to the literature, these lesions are pink or brown in color, where edematous pustular lesions or the previously mentioned papulovesicular lesions are usually interspersed, which generally measure from 1 to 10 mm in diameter, although other authors propose ranges that go from 1 to 5 mm and that, in addition, , they can stay for at least ten days with the possibility of presenting the positive Koebner phenomenon that consists of the early stage of the disease, where patients can present a transient rash on the back, chest or abdomen and desquamation [8,9]. Currently, CGS has been considered a delayed hypersensitivity reaction against certain antigens, especially those caused by certain viral infections such as those mentioned above [10, 11]. (Figure 1).
Figure 1 Graphic representation of the region’s most frequently involved in Gianotti-Crosti syndrome.
Taken from: Chuh A, Zawar V, Sciallis GF, Lee A. The diagnostic criteria of pityriasis rosea and Gianotti-Crosti syndrome – a protocol to establish diagnostic criteria of skin diseases. J R Coll Physicians Edinb. 2015. 45 (3):218-25.
However it is necessary to recognize the relationship between this Gianotti Crosti syndrome and acral exanthema, the latter being known as an acute and extensive rash of the skin, usually with spontaneous cutaneous resolution, of a pinkish color that generally appears as a consequence of some Infectious diseases, which may be accompanied by fever and dermatological manifestations located in peripheral areas, are known by the term "acral". As can be analyzed, both the syndrome in question and the acral exanthema have certain similarities, as can be seen in Table 2, such as, for example, the fact that they appear after infections that may well be viral or bacterial, as well as the possibility of appearing after immunizations, to manifest fever and pinkish or reddish skin lesions located on the extremities [12]. In fact, it has been proposed to use the term Gianotti-Crosti syndrome, regardless of its cause and form of presentation to describe all eruptive dermatoses of acral location [13]. However, it must be recognized that, although they are very similar and easily confused, Gianotti syndrome does not encompass all types of lesions as well as acral rashes if they involve a wide range of macular, popular, purulent, vesiculopapular, erythematous lesions, etc. , therefore, this is a point to take into account for the differential diagnosis, in addition to considering the negative clinical aspects of SGC that help the diagnosis, such as the absence of lesions on the trunk and the presentation of scaly lesions, additionally, The presentation of a febrile episode of low intensity, some 7-10 days before, accompanied by catarrhal manifestations of the upper respiratory tract cannot be ignored [14,15] (Table 3).
F
| Characteristic |
Gianotti Crosti syndrome |
Acral rash |
| Colour |
Pink or Brown |
Red or pinkish |
| |
They are mainly papulo-vesicular or edematous pustular |
Wide range (erythematous or purpuric, macular, papular, vesicular |
| |
|
and pustular |
| Injury |
|
and so on) |
| Self-limitation |
Yes |
Yes |
| |
On the cheeks, buttocks, and extensor surfaces of the extremities, it is rarely observed on the trunk, palms, soles, flexor areas, and mucous membranes. |
limbs, may occupy palms and soles of the feet |
| Location |
|
|
| Fever |
Yes (Low) |
Yes |
| Size |
Generally 1 to 10 millimeters in diameter |
It depends on the type of injury |
| Frequency |
Higher in children (from one to 6 years) |
Higher in children (Less than 1 year of age) |
| Cause |
Infection, often of viral origin (Epstein Barr virus) |
Infections or atopic dermatitis |
| Pathophysiology |
Not known |
Variable |
| Duration |
3-5 weeks |
It depends on the type of injury |
Table 3. Comparative table of Gianotti syndrome and acral rash.
Materials and Methods
A detailed bibliographic search of the most relevant published information is carried out in the databases PubMed, scielo, Medline, national and international libraries specialized in the topics covered in this review article. The following descriptors were used: Acropapulosis, Syndrome, Gianotti Crosti, Rash, Pediatrics, Dermatoses. The data obtained range between 5 and 30 records after the use of the different keywords. The search for articles was conducted in Spanish and English, limited by year of publication, and studies published from 2011 to the present were used.
Results
Gianotti-Crosti syndrome (GCS) is primarily a disease of early childhood; it is most common in children between 1 and 6 years of age. Characterized by an acute onset of a papular or papulovesicular rash with a symmetrical distribution, found predominantly on the cheeks, extensor surfaces of the extremities, and buttocks, sparing the antecubital and popliteal fossae, as well as the palms, plants and mucosal surfaces. With the advent of more universal vaccination against hepatitis B virus, the Epstein-Barr virus has become the most common etiologic agent of Gianotti-Crosti syndrome [15]. The pathophysiology is unknown. A delayed hypersensitivity reaction of the dermis to various pathogens and possibly to vaccines is assumed. The most likely process is a type IV local hypersensitivity reaction to the causative antigen. However, immunohistochemistry and electron microscopy findings are nonspecific and do not demonstrate the presence of viral particles or antigens in skin lesions, suggesting that lesion development does not involve a direct local interaction between viral antigens and immune cells. of the skin There may be prodromes such as pharyngitis, upper respiratory tract infection and diarrhoea. Lymphadenopathy is observed in 25-35% of cases [16, 17]. This is observed in the presentation of a case of a 22-month-old male patient who, on dermatological examination, observed blisters and vesicles of different sizes, isolated and grouped, located mainly on the face and upper and lower limbs, with some on the trunk. With positive serological tests for Epstein-Barr virus [18]. Likewise, the literature reports a case of a child diagnosed with this syndrome after vaccination against diphtheria, tetanus and pertussis and the live varicella virus vaccine [19]. GCS is diagnosed clinically by the presence of a characteristic rash and its distribution, with differential diagnoses including erythema multiform, lichen planus, popular urticaria, scabies, and atopic dermatitis, as in the case of Llanora et al. from a four-year-old boy presenting with characteristic reddish-brown, partially flat-topped papules on the extensor surface of the lower limbs [17]. Situation similar to the report by Escobar et al. from a four-year-old male patient with multiple papulovesicular lesions, some of which were normal skin color and others erythematous, monomorphic, 3-5 mm in diameter, firm, grouped, forming welldefined plaques with irregular edges, symmetrically distributed in the distal region upper and lower extremities, especially on the extensor surface of the hands (Figure 2) [20].
Figure 2 Erythematous plaques with irregular, well-defined borders with some vesicles and scaling on their surface distributed symmetrically on the dorsum of the feet.
Taken from Escobar, A. M., et al. "Síndrome de GianottiCrosti: diagnóstico a considerar en pacientes pediátricos con exantemas acrales." Revista argentina de dermatología 102.1 (2021): 21-30.
The classic presentation is that of a symmetric exanthema with an acral distribution, which, as it is a nonspecific viral exanthema, is usually underdiagnosed. Gianotti considered that these patients presented clinically different from infantile acrodermatitis pustular, and described acrolocalized papulovesicular syndromes [21]. Recent studies have reported viral rashes with a possible association with COVID-19 in Pediatric patients. They described a 10-month-old boy with Gianotti-Crosti syndrome in the setting of a recent positive RT-PCR test for SARS-CoV-2 to add to the collection of cutaneous manifestations of COVID-19. In particular, chilblains on acral surfaces are thought to occur frequently in children and young adults with COVID-19 [22]. Once again, a case report confirms the symmetrical acral appearance that characterizes GCS, therefore, it remains a clinical diagnosis of exclusion. The diagnosis is often made after the child has not been successfully treated for a more common cause of acral rash (eg, scabies), as there are no pathognomonic laboratory or histopathology findings [23]
Discussion
Gianotti-Crosti syndrome is a benign rash that presents in childhood and rarely in adulthood; is it associated with multiple viral, bacterial and vaccine diseases. It manifests as a popular eruption of acral distribution with associated systemic symptoms. Our results are similar to those of Neves et al, with respect to the age range in which it appears and the location of the lesions. The presentation of his case of a 2-year-old boy who, on physical examination, showed a papulovesicular exanthema predominantly on the extremities, legs and feet, buttocks and face; some crusty lesions on palms and soles [24]. Likewise, other authors guarantee that the vaccines are the main triggers of this condition, as in the case of a 6-year-old boy who, after receiving the second doses against measles-rubella with live attenuated viruses, started a skin rash, where skin-colored to erythematous, flat-topped papules <1.0 cm in diameter were seen symmetrically distributed on the extremities. Above the knees, several lesions had fused into plaques. In addition to these popular lesions, typical target lesions, comprising central discs of erythema, raised edematous intermediate rings, and red outer rings, <2 cm in diameter, were symmetrically scattered over the dorsal aspect of the ankles and feet [25] .The case Ion et al. agree with our results that a broad group of viruses can be associated with this syndrome, as in the case of a 3-year-old, 8-month-old girl with a generalized maculoerythematous rash associated with positive serologies for Epstein Barr, Echovirus, and Coxsackie viruses that raise suspicion of Gianotti-Crosti syndrome [26]. Although most cases occur in the Pediatric population, the literature also reports a case of an adolescent, which is important for the clinician not to rule out the possibility that the adult population is also affected while The distribution of lesions may vary, as in the case of an 18-year-old female patient who presented with acute skin lesions on the upper extremities, which later spread to the face, neck, torso, abdomen, and lower extremities, and on examination dermatology showed multiple normochromic and monomorphic papules, some of which formed crusts, distributed symmetrically [27]. This syndrome, in addition to its high link with parvovirus [28]. Is also associated with other entities such as atopic dermatitis and molluscum contagiosum [29].
Conclusion
Gianotti Crosti Syndrome is closely related to acral rash. This syndrome is characterized by an acral papular eruption with a symmetric distribution. It is a benign and self-limited disease present mainly in the Pediatric population due to infections and vaccinations. However, it is important that the clinician has knowledge of the characteristics of the lesions for their correct evaluation and management.
REFERENCES
- López-Cepeda, Larissa Dorina (2020) Síndrome de Gianotti-Crosti o acrodermatitis papular de la infancia. Rev Cent Dermatol Pascua 29: 20-25.
Indexed at, Google Scholar, Crossref
- Chuh A, Zawar V, Sciallis GF, Lee A (2015) Los criterios de diagnóstico de la pitiriasis rosada y el síndrome de Gianotti â? Crosti: un protocolo para establecer los criterios de diagnóstico de las enfermedades de la piel. JR Coll Médicos Edinb 45: 218â?225.
- Di Lernia V, Mansouri Y (2013) Epstein-Barr virus and skin manifestations in childhood. Int J Dermatol 52:1177-84.
Indexed at, Google Scholar, Crossref
- Niklitschek S, Romero W, Zegpi MS (2011) Síndrome de Gianotti-Crosti: reporte de dos casos y revisión de la literatura. Rev Ped Elec 8.
Indexed at, Google Scholar
- Admani S, Jinna S, Friedlander SF, Sloan B (2015) Cutaneous infectious diseases: Kids are not just little people. ClinDermatol. 1 de noviembre de 33:657-71.
Indexed at, Google Scholar, Crossref
- Aznar SL, Cemeli Cano M, Amiguet Biain MR (2019) Acrodermatitis papulosa infantil tras infección por virus de Epstein-Barr. Rev Pediatr Aten Primaria 21:81.
Google Scholar
- Silva JC, Torres MC (2014) Diagnóstico diferencial de los exantemas. Pediatría Integral 18:22-36.
Indexed at, Google Scholar
- Wells L, Mahil S (2018) Rash on extensor surfaces of a child. BMJ 360:5547.
Indexed at, Google Scholar, Crossref
- Knöpfel N, Noguera-Morel L, Latour I, Torrelo A (2019).Viral exanthems in children: A great imitator. Clin Dermatol 37:213-26.
Indexed at, Google Scholar, Crossref
- Hall LD, Eminger LA, Hesterman KS, Heymann WR (2015) Epstein-Barr virus: dermatologic associations and implications: part I. Mucocutaneous manifestations of Epstein-Barr virus and nonmalignant disorders. J Am Acad Dermatol. enero de 72:1-19.
Indexed at, Google Scholar, Crossref
- Caccavale S, Ruocco E (2017) Acral manifestations of systemic diseases: Drug-induced and infectious diseases. ClinDermatol 35:55-63.
Indexed at, Google Scholar, Crossref
- Coronel-Carvajal, Carlos (2021) Síndrome de Gianotti-Crosti o acrodermatitis papular de la infancia: presentación de un caso. Archivo Médico Camagüey 25:471-478.
Indexed at, Google Scholar
- Escalante-Jibaja, Emma y col (2018) Exantemas virales. dermatología peruana 28:167-184.
Google Scholar
- Someshwar S, Jerajani H. A (2014) case of Gianotti-Crosti syndrome. Muller J Med Sci Res.
Indexed at, Google Scholar
- Leung AKC, Sergi CM, Lam JM, Leong K F (2019) Gianotti-Crosti syndrome (papular acrodermatitis of childhood) in the era of a viral recrudescence and vaccine opposition. World J Pediatr 15:521-527.
Indexed at, Google Scholar, Crossref
- Leal SBC, Balconi SN, Cafrune FE (2021) Gianotti-Crosti syndrome and yellow fever vaccine: unprecedented reaction Int J Dermatol 60:e227-e228.
Indexed at, Google Scholar, Crossref
- Llanora, Genevieve Villablanca, Clifton Ming Tay, and Hugo PS van Beve (2012) Gianotti-Crosti syndrome: case report of a pruritic acral exanthema in a child. Asia Pacific Allergy 2:223-226.
Indexed at, Google Scholar, Crossref
- Marcassi AP, Piazza CAD, Seize MBMP, Cestari SDCP (2018) Atypical Gianotti-Crosti syndrome. An Bras Dermatol 93:265-267
Indexed at, Google Scholar, Crossref
- Retrouvey M, Koch LH, Williams JV (2013) Gianotti-Crosti syndrome following childhood vaccinations. Pediatr Dermatol 30:137-8.
Indexed at, Google Scholar, Crossref
- Escobar A M (2021) Síndrome de GianottiCrosti: diagnóstico a considerar en pacientes pediátricos con exantemas acrales. Revista argentina de dermatología 102:21-30.
Google Scholar
- Soto, AD Novelo (2017) Gianotti-Crosti Syndrome in Adult Patient Following Enterovirus Infection: Case Report. Dermatología Cosmética, Médica y Quirúrgica 15:99-102.
Google Scholar
- Swali Ritu N, Erica B Lee, Jennifer L Adams (2021) Gianottiâ?crosti syndrome in the setting of recent coronavirus diseaseâ?19 infection. Pediatric dermatology 38:629-631.
Indexed at Google Scholar, Crossref
- Sears W, Hodge B, Jones B, Thompson M, Vidwan N (2014) Visual diagnosis: 12-month-old boy with persistent rash and lymphadenopathy. Pediatr Rev 35:452-455.
Indexed at, Google Scholar, Crossref
- Neves IM, Nogueira MV, Patraquim C, Alves MC (2021) Gianotti-Crosti syndrome: a frequent but underdiagnosed rash. BMJ Case Rep14:e244988.
Indexed at, Google Scholar, Crossref
- Oka M (2021) Simultaneous Development of Gianotti-Crosti Syndrome and Erythema Multiforme Following Second Dose of Measles-rubella Vaccine. Acta Derm Venereol.
Indexed at, Google Scholar, Crossref
- Ion, Laura-Mihaela (2021) SYND"GIANOTTI-CROSTI ROME." Romanian J Pediat Rics 70:156.
- Pedreira RL, Leal JM, Silvestre KJ, Lisboa AP, Gripp AC (2016) Gianotti-Crosti syndrome: a case report of a teenager. An Bras Dermatol 91:163-165.
Indexed at, Google Scholar, Crossref
- Chuh A, Zawar V, Lee A, Sciallis G (2016) Is Gianotti-Crosti Syndrome Associated with Atopy? A Case-Control Study and a Postulation on the Intrinsic Host Factors in Gianotti-Crosti Syndrome. Pediatr Dermatol. 33:488-92.
Indexed at, Google Scholar, Crossref
- Estébanez A, Silva E, Guillen S, García A, Martín JM (2020) Síndrome de Gianotti-Crosti-like secundario a Molluscum contagiosum [Gianotti-Crosti syndrome-like reaction secondary to Molluscum contagiosum] An Pediatr 93:49-50.
Indexed at, Google Scholar, Crossref
Citation: Citation: Garcia Medina LC, Romero Diaz YL, Sanchez Silvera ZM, Montes YC, Gómez Patiño J, et al. (2022) Gianotti Crosti Syndrome and Its Relationship with Acral Rash- Pediatric Approach. Health Sci J. Vol. 16 No. S6: 926.