Case Report - (2023) Volume 15, Issue 6
Giant congenital paraovarian cyst presenting with dyspeptic symptoms
Tulay Dilara Deniray*
Department of Internal Medicine, University of Health Sciences, Bursa Şehir Training & Research Hospital, Bursa, Turkey
*Correspondence:
Tulay Dilara Deniray, Department of Internal Medicine, University of Health Sciences, Bursa Şehir Training & Research Hospital, Bursa,
Turkey,
Tel: + 90 5358857979,
Email:
Received: 01-Nov-2023, Manuscript No. ipaom-23-14284;
Editor assigned: 03-Nov-2023, Pre QC No. P-14284;
Reviewed: 15-Nov-2023, QC No. Q-14284;
Revised: 21-Nov-2023, Manuscript No. R-14284;
Published:
28-Nov-2023
Abstract
Paraovarian cysts are benign lesions arising from paramesonephric
or mesonephric canal remnants. They are thin-walled, nonvascularized,
contain homogeneous serous fluid without septation,
and most commonly occur in the fourth or fifth decades of life.
Paraovarian cysts are usually asymptomatic and range in size from
2 to 20 cm. These cysts, which are typically modest in diameter, can
become symptomatic when they reach a large diameter. We present
the management of a 30 × 24 cm paraovarian cyst in an 18-yearold
nulligravid patient who presented to the outpatient clinic with
complaints of dyspepsia, nausea, vomiting, loss of appetite, and
abdominal pain discomfort in this case report.
Keywords
Paraovarian cysts; Dyspepsia; Adolescent
Introduction
Intraabdominal cysts may have various causes,
including congenital or acquired conditions. They can be
benign or malignant and range from small to large. Some
common types of intraabdominal cysts include ovarian
cysts, pancreatic cysts, hydatid cysts, and splenic cysts.
The development mechanism of paraovarian cysts has
yet to be fully understood. However, some theories suggest
that they may form from remnants of embryonic cells left
behind after the development of the reproductive system.
These cells can grow into cysts that are surrounded by a
fluid-filled sac. Other theories suggest that paraovarian
cysts may develop due to an obstruction in the fallopian
tubes or an abnormal fluid accumulation in the area
surrounding the ovaries [1].
Changes in hormone levels during the menstrual
cycle may contribute to the forming paraovarian cysts.
Endometriosis, a disorder in which tissue comparable to
the uterine lining grows outside the uterus, may be linked
to certain cysts. This tissue can also produce cysts in the
vicinity of the ovaries [2].
It is important to note that not all paraovarian cysts
are the same, and their development mechanism may
vary based on the type of cyst. Further studies are needed
to understand better the exact mechanisms behind the
development of paraovarian cysts. Paraovarian cysts
are benign cysts that develop in the tissue surrounding
the ovaries. They are also known as "paraovarian" or
"infundibulopelvic" cysts. These cysts are found in the
broad ligament and can originate from either neoplastic
or non-neoplastic origins and can occur in women of all
ages, but they are most common in women of childbearing
age [3-5]. These cysts constitute 3% to 20% of all adnexal
masses [6] and are primarily benign and usually arise from
paramesonephric and mesonephric remnants [4]. The
true epidemiology of these cysts is challenging to evaluate
because they are frequently diagnosed in asymptomatic
patients [7]. Clinical signs and symptoms arise due to the
pressure effect on neighboring organs or complications.
The literature reported that paraovarian cysts' diameter
varies between 2 and 20 cm.
In this case report, an 18-year-old woman with
dyspepsia was found to have a massive (30 × 24 cm) rightsided
paraovarian cyst that had been extending from her
pelvis to her epigastric region. The cyst was successfully
removed by surgery.
Case Presentation
An 18-year-old post-pubertal female with no history
of chronic illness was admitted to the internal medicine
outpatient clinic with gradually increased complaints of
dyspepsia, nausea, appetite and weight loss, abdominal
tenderness, and swelling for the last two months. A wellcircumscribed
tender with deep palpation mass from the
right lower quadrant to the epigastric region was observed
on the physical examination. Laboratory results reveal
that she is not pregnant, and sexual hormone (FSH,
LH, Progesterone, and Estradiol) levels were within
normal limits. Complete blood counts, liver (AST, ALT,
ALP, GGT, Bilirubin), kidney (BUN, Creatinine) tests,
electrolytes (Na+, K+, Ca2+, Mg2+, Cl-), and inflammation
parameters (ESR, CRP) were average. Echinococcal
indirect hemagglutination test was negative. Urinalysis was
non-significant, and tumor markers (CEA, CA-19.9, CA-
15.3, CA-125, AFP) were negative.
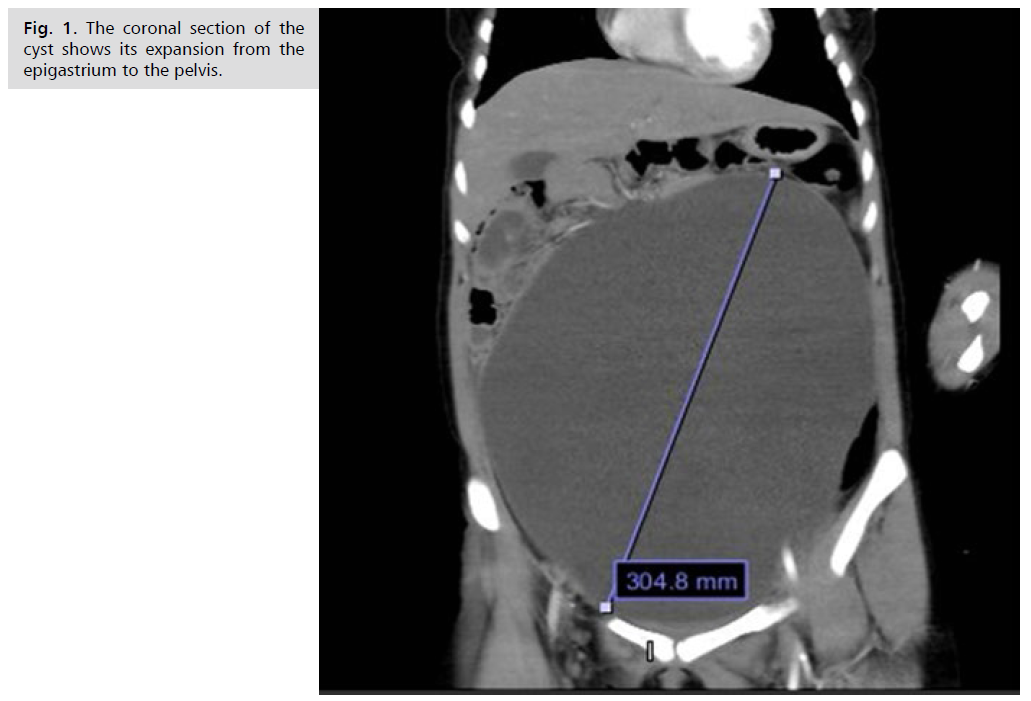
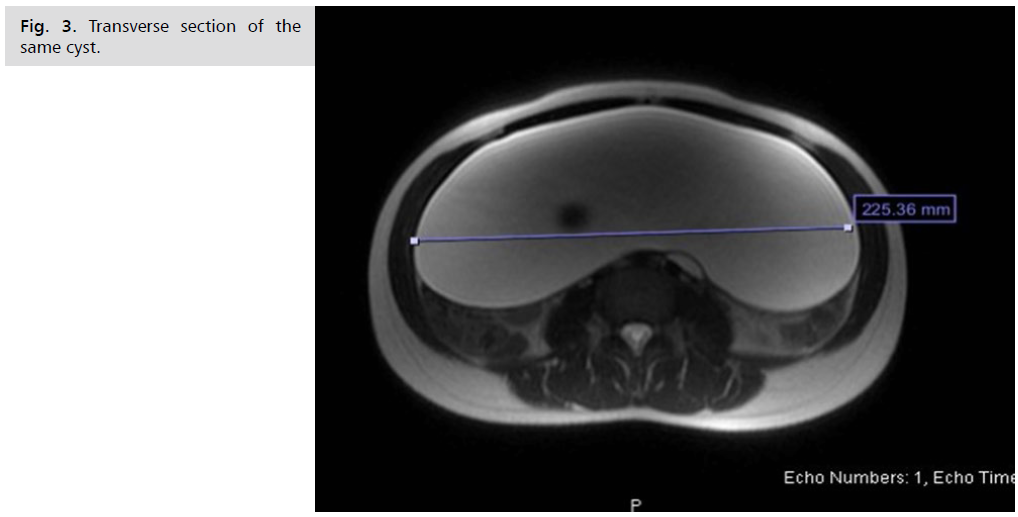
Magnetic resonance imaging revealed a cystic mass
with dimensions of 30 × 22 × 7.5 cm that extends from
the anterior abdomen's epigastric area to the pelvis's upper
section of the bladder. The bladder’s filling and shape are
both consistent. In the lumen, there was no discernible
pattern or appearance of mass. The uterus was anteverted
and deviated to the right. A 20 mm diameter follicle was
observed in the right ovary. The left ovary was normal (Fig. 1.-Fig. 3.).
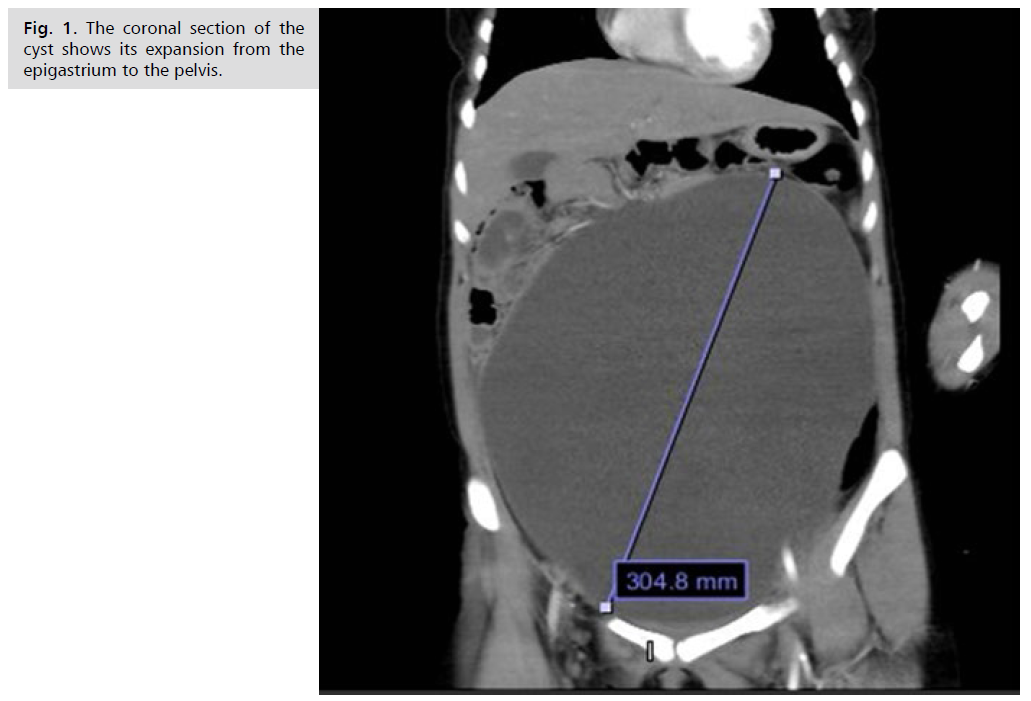
Fig. 1. The coronal section of the cyst shows its expansion from the epigastrium to the pelvis.

Fig. 2. Sagittal section from the same MRI of this particular cyst shows a deviated uterus.
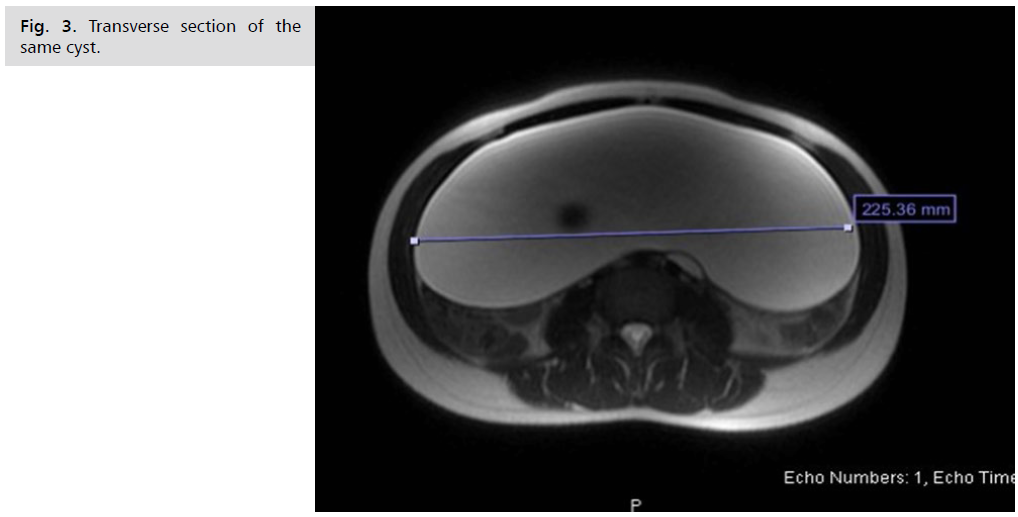
Fig. 3. Transverse section of the same cyst.
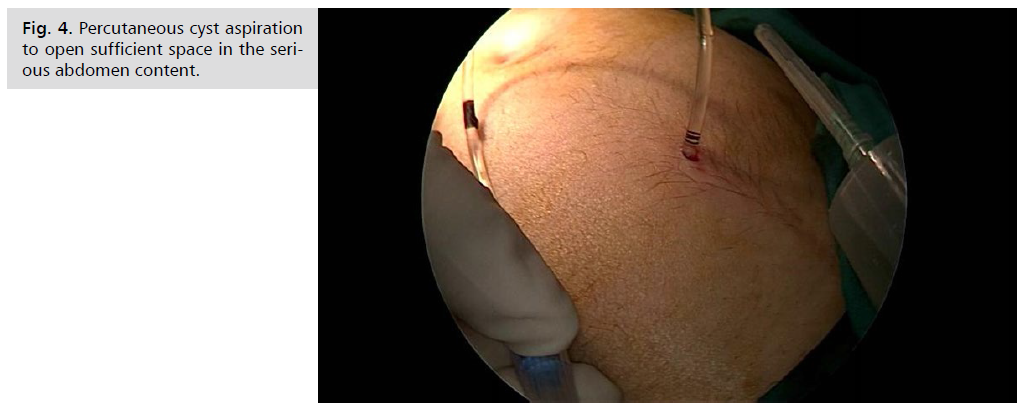
The pediatric surgery department consulted the
patient since it was anticipated that a mesenteric cyst, a
congenital urachus cyst, or an omental cyst might cause
the cyst suppressing the intestinal logs. Under general
anesthesia with intubation, a 10F cystostomy catheter was
inserted into the cyst under ultrasound guidance. Almost
seven liters of serous cyst fluid was aspirated. Then, a 13
mmHg pneumoperitoneum was created by inserting a
Veress needle from the umbilicus, and a 10 mm camera
port was placed. Under direct vision, 5 mm working ports
were placed in the left iliac region and just to the left of
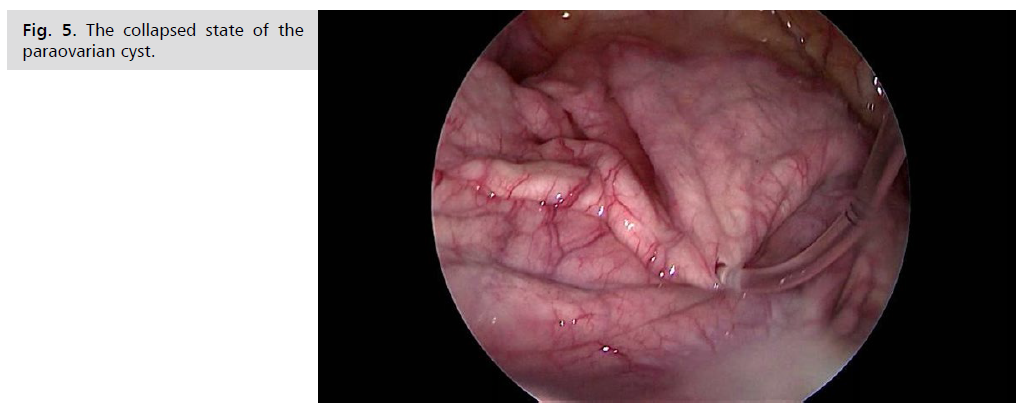
the umbilicus. Laparoscopy revealed a typical appearance
of ovaries, uterus, and collapsed paraovarian cyst in the left
tubal mesentery. The cyst was excised by blunt dissection
without opening the capsule. It was too large to fit into the
endobag and was removed through the umbilical incision.
Hemorrhage control, pelvis irrigation, and aspiration were
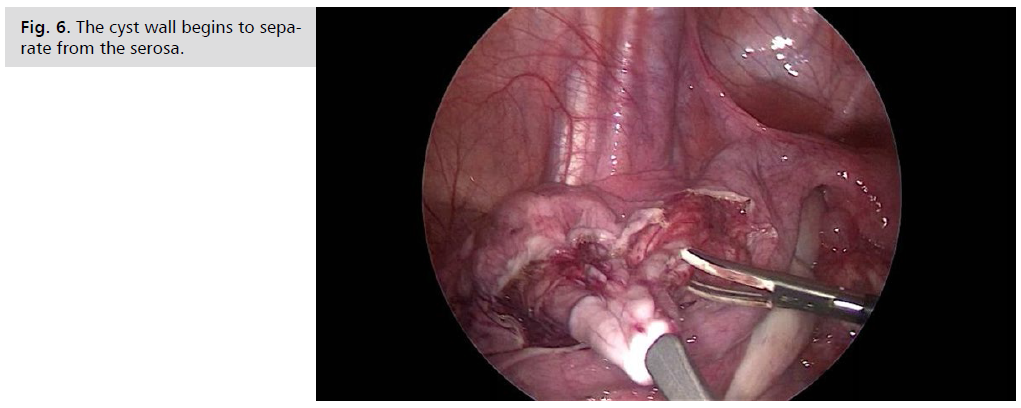
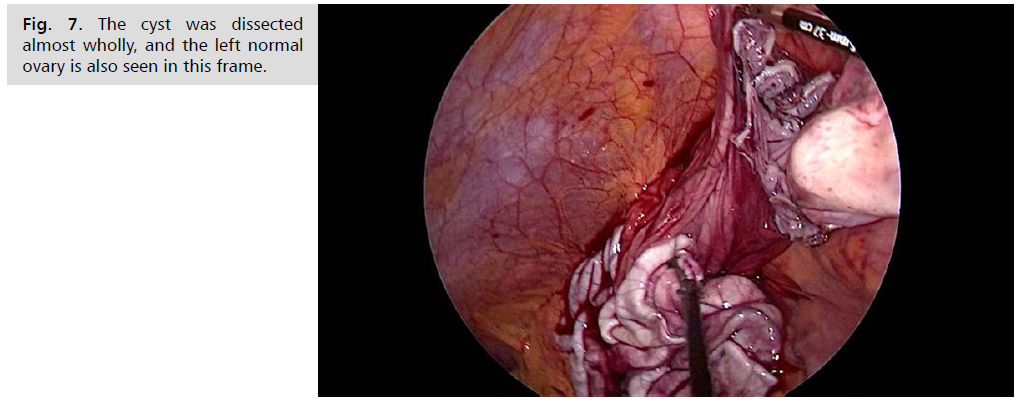
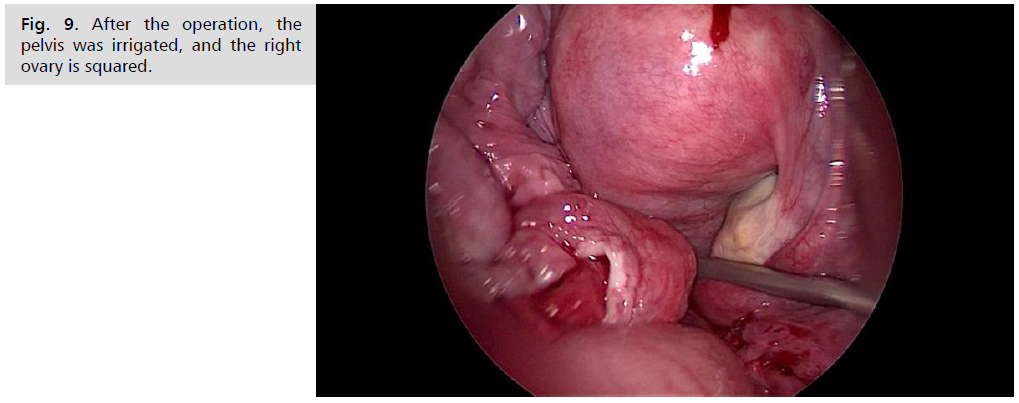
performed, and no drain was placed (Fig. 4.-Fig. 9.).
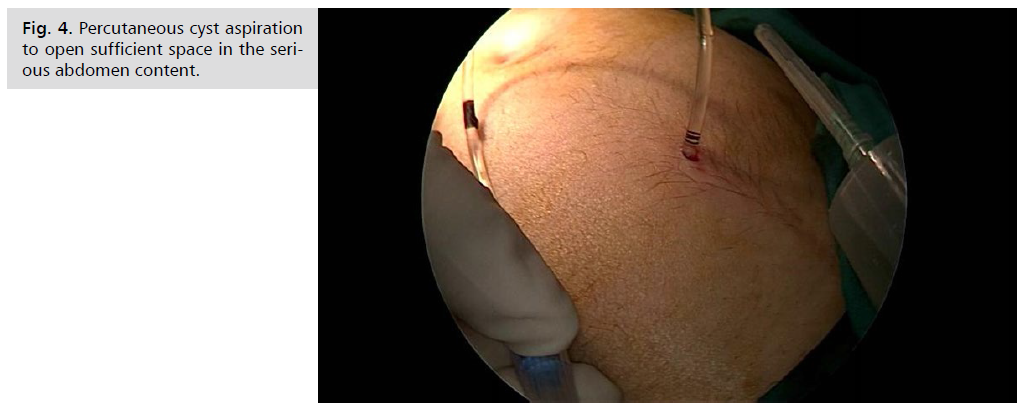
Fig. 4. Percutaneous cyst aspiration to open sufficient space in the serious abdomen content.
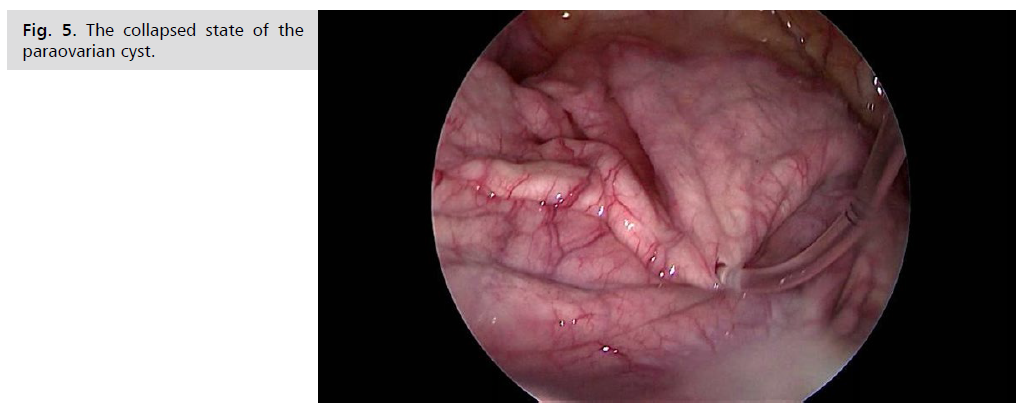
Fig. 5. The collapsed state of the paraovarian cyst.
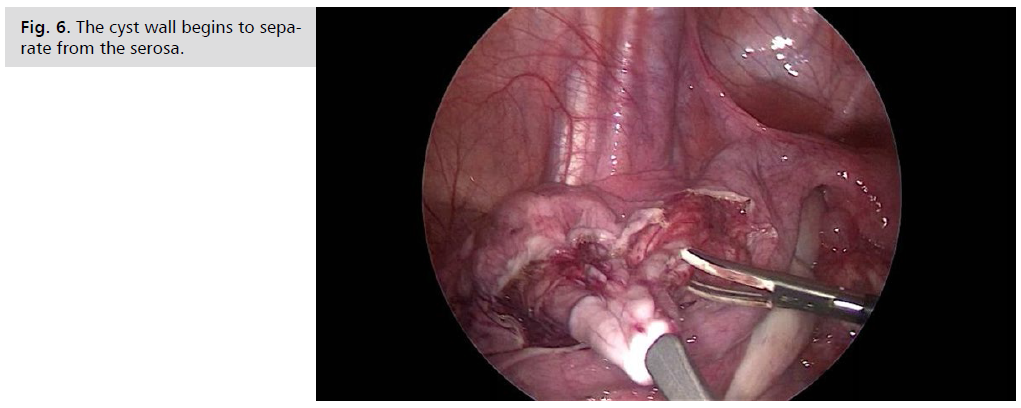
Fig. 6. The cyst wall begins to separate from the serosa.
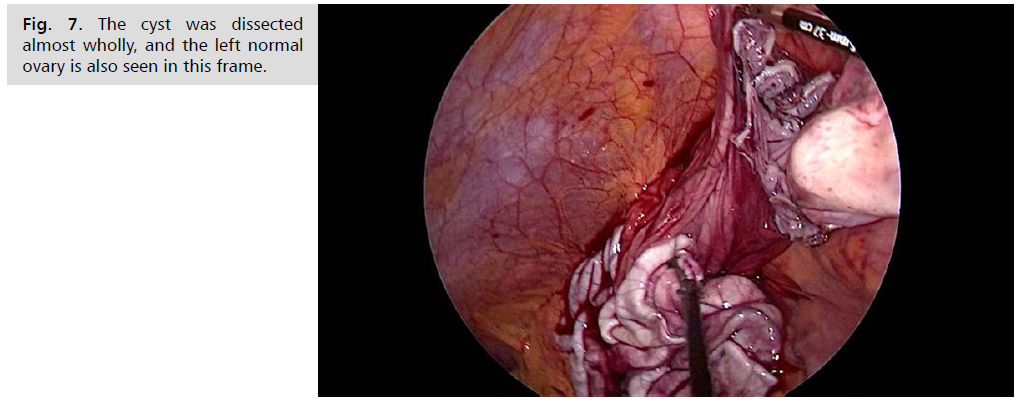
Fig. 7. The cyst was dissected almost wholly, and the left normal ovary is also seen in this frame.

Fig. 8. Removal of the cyst wall from the umbilicus.
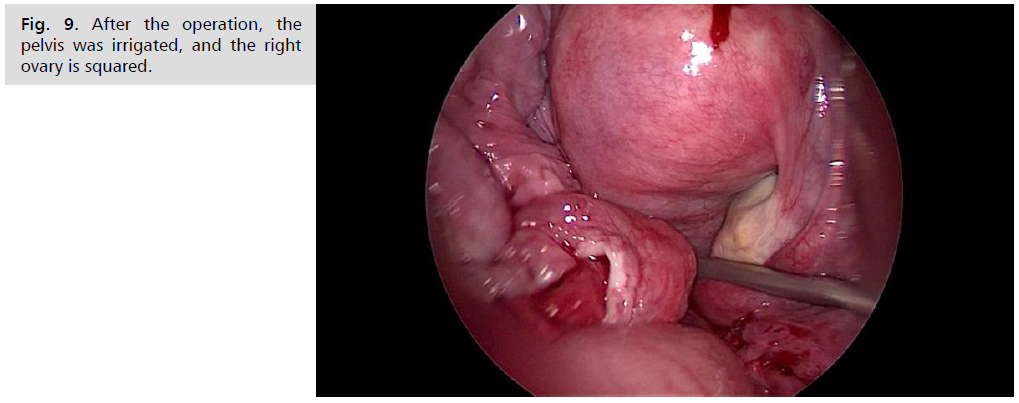
Fig. 9. After the operation, the pelvis was irrigated, and the right ovary is squared.
Discussion
Potential causes for premenstrual ovarian masses
include cysts, torsion, benign and malignant tumors,
ovarian leukemia, lymphoma, and spreading malignancies
[8]. Juvenile ovarian cysts are infrequent, and most are not
cancerous [9]. The prevalence of epithelial malignancies in
children rises with age, with the majority occurring after
menarche. Since most instances (65%) are around 17-yearolds,
it is thought that hormones may induce ovarian
epithelial cysts [10]. These patients are typically postpubertal
teens, and paraovarian cysts with high diameters
are more common in this group.
Symptoms are caused mainly by subileus, which can
result from compression effects. Patients were advised to
contact emergency services when experiencing abdominal pain, bloating, nausea, or vomiting [11]. Paraovarian cysts
can cause adnexal torsion in some people. However, this is
extremely rare [12]. Our patient was already asymptomatic
for about two months since gradually increased abdominal
diameter was noticed. The first admission symptom was
dyspepsia due to the pressure of a giant cyst in the stomach.
The absence of high fever, sweating, and severe abdominal
pain suggested a chronic process more than an acute
disease. A well-defined formation on the abdominal wall,
from the pubis to the epigastric region, was detected on
physical examination.
Higher expertise and precision are expected for
ultrasonographic diagnosis of paraovarian cysts [13].
Ultrasound findings include a well-defined oval or round
cyst that is close but separated from the ipsilateral ovary,
the absence of a surrounding follicle, and the appearance of
the split sign, which is the slight oscillatory movement of
the cyst and ovary while being pressed by the endovaginal
probe. Ovarian cysts, hydrosalpinxes, and peritoneal
inclusion cysts can all be distinguished with ultrasound.
Ultrasound characterization of the cyst aids in determining
a simple from a malignant paraovarian cyst. Our patient's
ultrasonography reported no definitive findings except
a 30 × 22 × 7.5 cm dimension homogeneous cyst. On MRI, a paraovarian cyst presents as a homogeneous
mass between the uterus and the epigastrium, but no
comments were available for the origin of the mass. The
major challenge in the current case was determining which
organ or tissue gave rise to the current cystic formation.
When considering the formations that may have occurred
between the starting point and the endpoint on imaging,
we can list them as follows: massive mass originating
from congenital mesonephric canal residue, renal cystic
formation, tubovarian cysts, or abscess, epidermoid cysts,
intra-abdominal adnexal mass-related malignancy, hydatid
cysts caused by Echinococcus granulosus infection or a
malignancy arising from the bladder wall.
The imaging showed that the cyst was homogenous
and did not contain hemorrhagic components and
septation, and no accompanying signs of malignancy
were accompanying. Laboratory evaluation shows no
signs of inflammation, and tumor markers were within
normal limits. Due to their location, adnexal masses and
mesonephric canal residues were the most emphasized
diagnoses. Clinically, post-pubertal mesonephric cystic adenocarcinoma cases in mesonephric canal residues have
been observed in the literature. It has been determined that
it does not fit our instance owing to the presentation of this
issue before it reaches such a massive size and the frequent
torsion in adnexal structures. The cyst was considered noninflammatory
and benign when the clinical and laboratory
findings and imaging were evaluated.
In such circumstances, diagnostic surgery should
be conducted regardless of the preliminary diagnosis for
a conclusive diagnosis. Inspection during surgery will
be critical in determining the exact location of the mass
and its connection to the surrounding organs and tissues.
The patient benefits from surgery in both diagnostic and
therapeutic aspects. A definitive patient diagnosis was
made by pathological examination of the excised material
as a paraovarian cyst.
Paraovarian cysts are benign lesions that arise from
paramesonephric or mesonephric canal remnants and are most common in women in their forties and fifties
[14,15]. Adolescent paraovarian cysts, such as the Gartner
cyst, are most frequently congenital [16]. Gartner cysts
are paraovarian cysts that can sometimes grow to the
renal regions, even though they are most commonly
detected in the top wall of the vagina [16-18]. Due to
the paramesonephric and mesonephric tract residues,
concomitant metanephric urinary system abnormalities
can occur.
Conclusion
In particular, ectopic ureter, ureter duplication, or
ectopic kidney anomalies may be noticed; therefore, a
thorough evaluation and magnetic resonance imaging
should be scheduled before the operation regarding
the cyst's interaction with surrounding tissues and any
associated organ anomalies. Surgical dissection should be
performed during cyst excision, and ureter damage may
occur during surgery regarding this unusual ureter trace.
Surgery should be planned electively by examining for renal
anomalies in such cases. Our patient had no renal or ureteral
abnormalities. Since these instances can be confused with
adnexal diseases, the ovaries' ultrasonographic vision and
the cyst wall expansion along a line above the ovary should
be closely studied.
Conflict of Interest
The authors declared that there are no potential conflicts
of interest concerning this article's research, authorship,
and/or publication.
References
- Stefanopol IA, Baroiu L, Neagu AI, et al. Clinical, imaging, histological and surgical aspects regarding giant paraovarian cysts: A systematic review. Ther Clin Risk Manag. 2022;29:513-522.
Google Scholar, Crossref, Indexed at
- Tzur T, Tzur Y, Baruch S, et al. Clinical presentation of paraovarian cysts. Isr Med Assoc J. 2022;24(1):15-19.
Google Scholar, Indexed at
- Skaff B, Zoorob D, El Assaad R, et al. Minimally invasive excision of a giant paratubal cyst: Case report and management review. Case Rep Obstet Gynecol. 2019;23.
Google Scholar, Crossref, Indexed at
- Durairaj A, Gandhiraman K. Complications and management of paraovarian cyst: A retrospective analysis. J Obstet Gynaecol India. 2019;69:180-184.
Google Scholar, Crossref, Indexed at
- Genadry R, Parmley T, Woodruff JD, et al. The origin and clinical behavior of the parovarian tumor. Am J Obstet Gynecol. 1977;129(8):873-880.
Google Scholar, Crossref, Indexed at
- Samaha M, Woodruff JD. Paratubal cysts: Frequency, histogenesis, and associated clinical features. Obstet Gynecol. 1985 May 1;65(5):691-694.
Google Scholar, Indexed at
- Honore LH, O'hara KE. Serous papillary neoplasms arising in paramesonephric parovarian cysts: A report of eight cases. Acta Obstet Gynecol Scand. 1980;59(6):525-528.
Google Scholar, Crossref, Indexed at
- Flotho C, Rückauer K, Duffner U, et al. Mucinous cystadenoma of the ovary in a 15-year-old girl. J Pediatr Surg. 2001;36(6):1-3.
Google Scholar, Crossref, Indexed at
- Karaman A, Azılı MN, Boduroğlu EC, et al. A huge ovarian mucinous cystadenoma in a 14-year-old premenarchal girl: Review on ovarian mucinous tumor in premenarchal girls. J Pediatr Adolesc Gynecol. 2008 Feb 1;21(1):41-44.
Google Scholar, Crossref, Indexed at
- Grapsa D, Kairi-Vassilatou E, Kleanthis C, et al. Epithelial ovarian tumors in adolescents: A retrospective pathologic study and a critical review of the literature. J Pediatr Adolesc Gynecol. 2011;24(6):386-388.
Google Scholar, Crossref, Indexed at
- Kostov M, Mijović Ž, Mihailović D et al. Giant paraovarian cyst in a child complicated with torsion. Vojnosanit Pregl. 2008;65(11):843-846.
Google Scholar, Crossref, Indexed at
- Macarthur M, Mahomed AA. Laparoscopy in the diagnosis and management of a complicated paraovarian cyst. Surg Endosc. 2003;17:1676-1677.
Google Scholar, Crossref, Indexed at
- Sokalska A, Timmerman D, Testa AC, et al. Diagnostic accuracy of transvaginal ultrasound examination for assigning a specific diagnosis to adnexal masses. Ultrasound Obstet Gynecol. 2009;34(4):462-470.
Google Scholar, Crossref, Indexed at
- Stenbäck F, Kauppila A. Development and classification of parovarian cysts. An ultrastructural study. Gynecol Obstet Invest. 1981;12(1):1-0.
Google Scholar, Crossref, Indexed at
- Damle LF, Gomez-Lobo V. Giant paraovarian cysts in young adolescents: A report of three cases. J Reprod Med. 2012;57(1-2):65-67.
Google Scholar, Indexed at
- Letizia MJ, Kelly JV. Case report: Gartner's duct cyst. Emerg Med News. 2011;33(5):35.
Google Scholar, Crossref, Indexed at
- Lee MJ, Yoder IC, Papanicolaou N, et al. Large Gartner duct cyst associated with a solitary crossed ectopic kidney: Imaging features. J Comput Assist Tomogr. 1991;15(1):149-151.
Google Scholar, Crossref, Indexed at
- Arumugam AV, Kumar G, Si LK, et al. Gartner duct cyst in pregnancy presenting as a prolapsing pelvic mass. Biomed Imaging Interv J. 2007;3(4).
Google Scholar, Crossref, Indexed at