Keywords
Gynecological lymphoma; Primary extranodal non-Hodgkin lymphoma
Abbreviations
IMRT: Intensity Modulated Radiation Therapy; VMAT: Volumetric Modulated Arc Therapy; LV10Gy: Percentage of lung volume receiving 10 Gy; MLD: Mean Lung Dose; HV10Gy: Percentage of heart volume receiving 10 Gy; MHD: Mean Heart Dose
Introduction
Hematologic malignancies and specially lymphomas can involve the female reproductive organs and breasts. Lymphomas are immune system neoplasms, which can be divided into Hodgkin and non-Hodgkin lymphomas. Lymphomas can be further divided into nodal lymphomas when they arise in lymph nodes, or extranodal lymphoma. The gastrointestinal tract and the skin are the most frequent sites for the extranodal types, up to 25% of all cases of lymphomas. Extranodal lymphomas are further classified as primary or secondary. Lymphomas of the female genital tract are uncommon, most of them being secondary tumors. They represent 1-1.5% of all cases of lymphomas. The cervix is the most frequent site of primary genital extranodal lymphoma and the ovaries are most often affected by secondary lymphomas [1]. Since lymphomas require different treatment than primary gynaecological malignancies, it is important to rely on a solid pathological diagnosis. Although rare, we here review throughout our case reports, the clinical, radiologic and pathologic features of primary extranodal female genital tract and breast non-Hodgkin lymphoma. We present two cases of primary lymphoma of genital tract (cervical and endometrial) and a case of breast MALT lymphoma.
Case Presentation
Cervical lymphoma
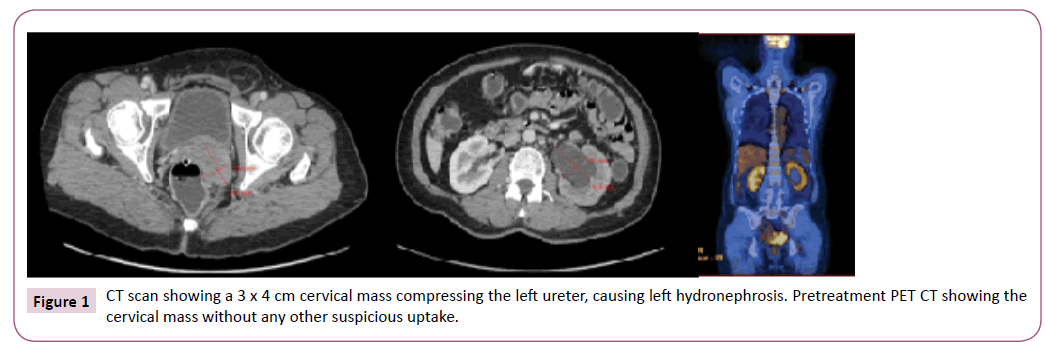
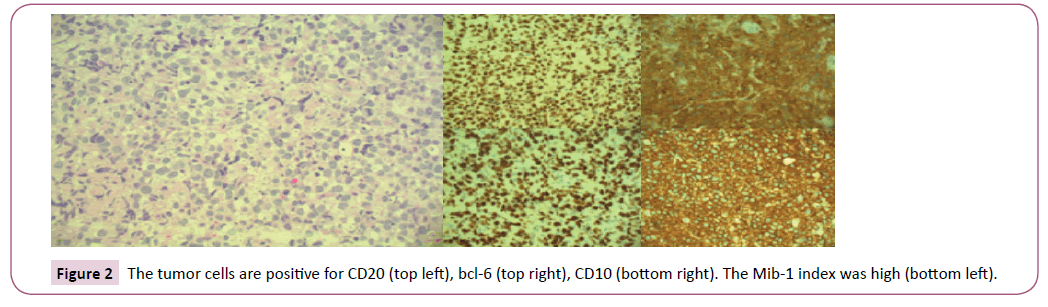
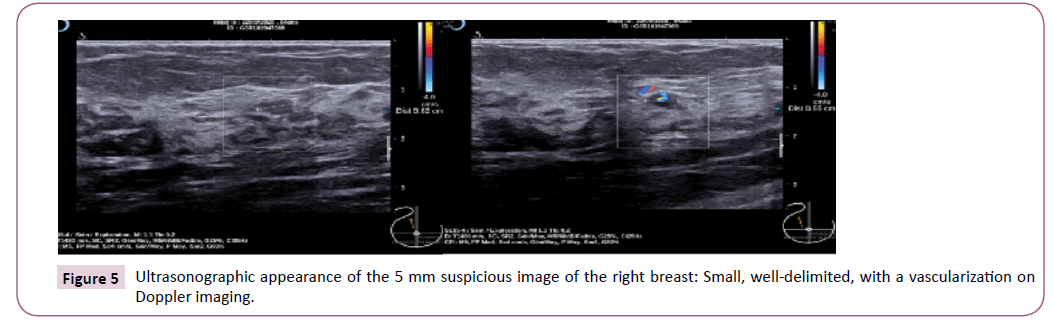
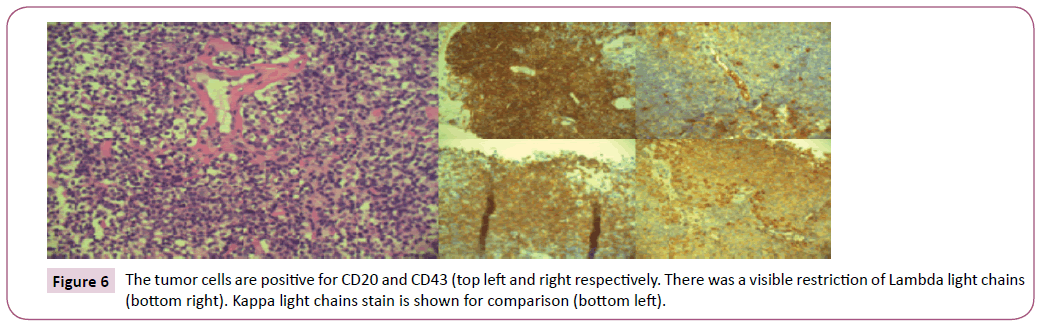
A 50-year-old postmenopausal patient presented with vaginal bleeding and dyspareunia. The gynaecological examination revealed a cervical mass with left lateral vaginal fornix invasion. A 3 x 4 cm cervical mass compressing the left ureter and grade III hydronephrosis was identified on chest/abdomen/pelvic CT. No suspicious lymph nodes were noted. The whole-body PET/ CT revealed an intense cervical FDG uptake without distant metastasis. The cervical biopsy showed a diffuse large B cell lymphoma (DLBCL). Immunohistochemistry do not reveal the coexpression of protein BCL-2 and MYC. The tumour was staged 1E with a prognostic index of 2/5. The patient underwent 6 cycles of R-CHOP and 2 cycles of rituximab with complete remission on PET CT (Figures 1 and 2).
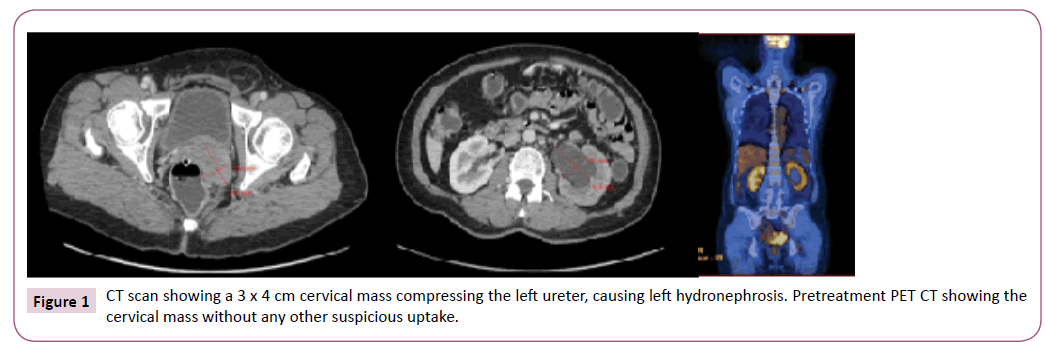
Figure 1: CT scan showing a 3 x 4 cm cervical mass compressing the left ureter, causing left hydronephrosis. Pretreatment PET CT showing the cervical mass without any other suspicious uptake.
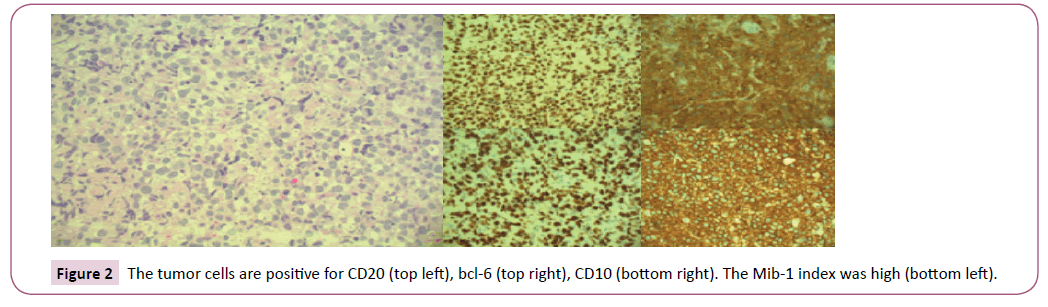
Figure 2: The tumor cells are positive for CD20 (top left), bcl-6 (top right), CD10 (bottom right). The Mib-1 index was high (bottom left).
Uterine and endometrial lymphoma
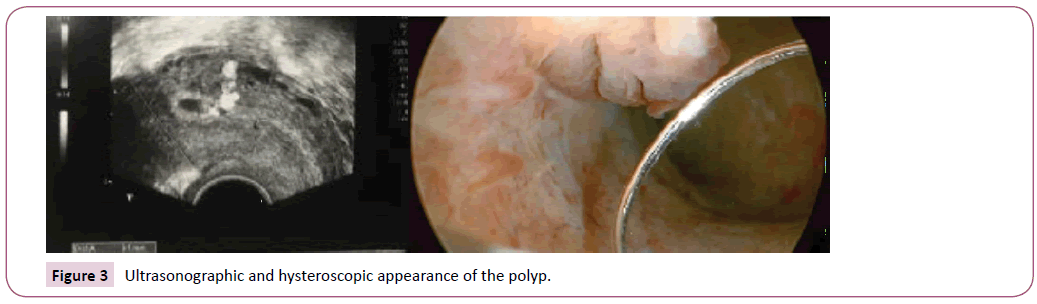
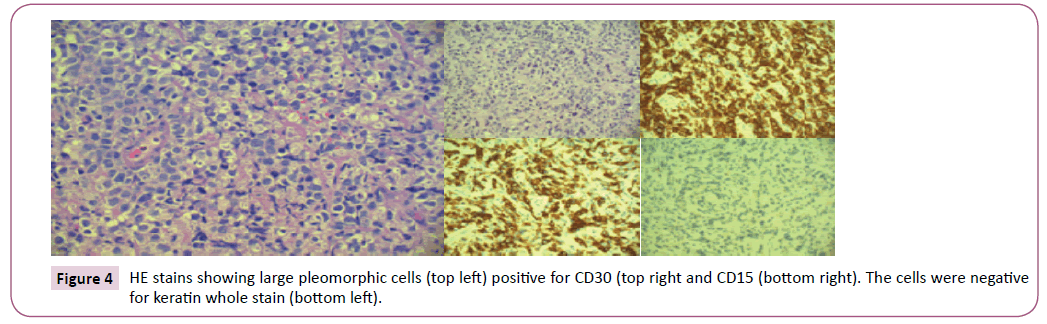
A 3G 0P 30-year-old patient presented with abnormal uterine bleeding after a spontaneous miscarriage. Transvaginal ultrasound revealed hematometra and a small endometrial polyp. Hysteroscopy confirmed a millimetric polyp, which was resected. The polyp was positive for CD15 and CD30, but negative for epithelial and trophoblastic markers. A monoclonal band IgK isolated on PCR confirmed the final diagnosis of lymphoma. A subsequent endometrial biopsy by D&C failed to identify the type of lymphoma. The chest/abdomen/pelvic CT and the peripheral blood analysis were normal. Epstein Barr virus came back negative. After multidisciplinary case discussion, clinical surveillance with a repeated hysteroscopy in 3 months was decided. Pathology obtained after repeated hysteroscopy found an endometrial polyp, without lymphoblastic cells and negative immunostaining for CD30, CD15 and p63. With this result, the patient is considered treated (Figures 3 and 4).
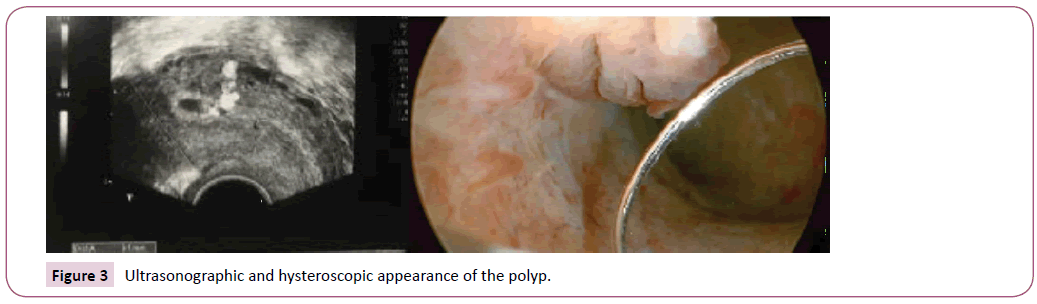
Figure 3: Ultrasonographic and hysteroscopic appearance of the polyp.
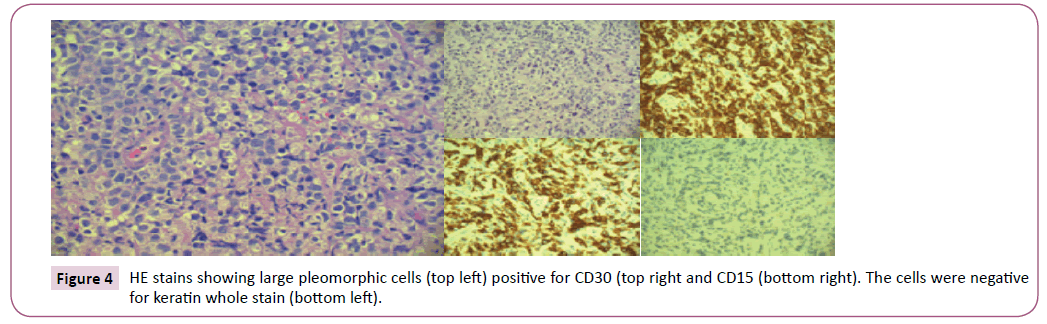
Figure 4: HE stains showing large pleomorphic cells (top left) positive for CD30 (top right and CD15 (bottom right). The cells were negative for keratin whole stain (bottom left).
Breast lymphoma
An 84-year-old patient, previously treated for a colic adenocarcinoma Dukes stage B2, consulted for a self-palpation of a lump in her left breast. She was diagnosed with left breast invasive ductal carcinoma and right breast 5 mm mucosaassociated lymphoid tissue (MALT) lymphoma. The bone marrow biopsy, the chest/abdomen CT and the gastroscopy were negative. She was treated with left breast conservative surgery, bilateral breast radiation and hormonal therapy with Tamoxifen (Figures 5 and 6).
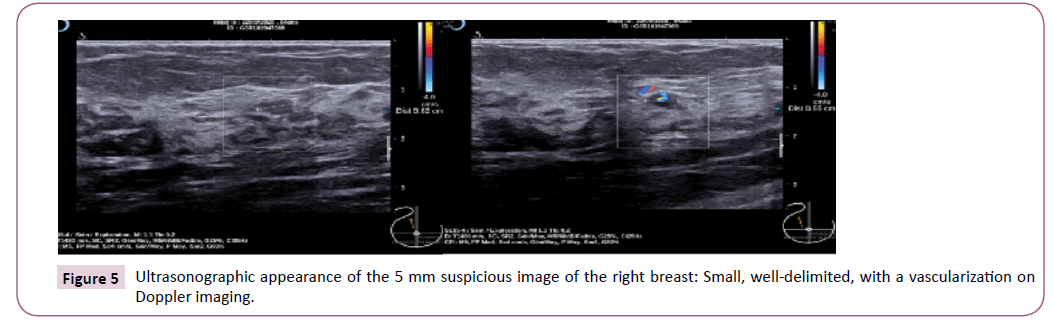
Figure 5: Ultrasonographic appearance of the 5 mm suspicious image of the right breast: Small, well-delimited, with a vascularization on Doppler imaging.
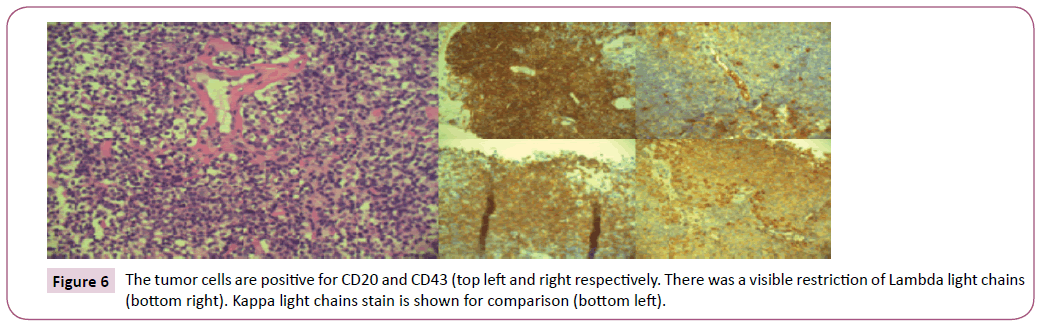
Figure 6: The tumor cells are positive for CD20 and CD43 (top left and right respectively. There was a visible restriction of Lambda light chains (bottom right). Kappa light chains stain is shown for comparison (bottom left).
Discussion
General consideration
Primary gynecological non-Hodgkin lymphomas are uncommon, reaching up to 165 cases per year in the United States [2]. Gynecological involvement is seen in only 4% of female patients presenting DLBCL [2,3], but when the female organs are involved, it is associated with lower overall survival rate. Extranodal lymphomas seem to exhibit different tumoral behavior than nodal lymphomas. Extranodal lymphomas are subdivided as “primary” and “secondary”. The following criteria are required to consider a primary genital tract non-Hodgkin lymphoma:
• The disease must be limited to a single location at diagnosis,
• The peripheral blood and bone marrow must be free of tumor cells and
• There should be no evidence of the disease elsewhere in the body months after diagnosis.
An association between chronic inflammation and some type of extra nodal lymphomas such as gastric, cervical or endometrial lymphoma is observed [2]. The definitive diagnose of lymphoma is based on immunohistochemistry, flow cytometry, cytogenetics and molecular genetic analysis. Markers like CD20 (B cell), CD3 (T cell), CD45 (leucocyte common antigen), CD10, BCL-6, BCL-2, CD5, MUM-1, Cyclin D1, IRTA1, Ki67 determine the typisation. Lagoo and Al recommend using both Ann Arbor System and FIGO classification for staging.
The International prognostic index considers patient age, stage, number of extranodal sites, performance status and LDH serum levels to assess prognosis. Some of immunochemistry markers are identified as prognostic factors. For example, the Hans algorithm using CD10, BCL-6 and MUM1 can divide with a reasonable accuracy DLBCL into germinal center-type and non-germinal center-type (or activated B cell type), both types having different gene expression profiles, prognostics and treatment options [4] (Table 1).
| Carcinoma of the Endometrium |
| IA |
Tumor confined to the uterus, no or <½ myometrial invasion |
| IB |
Tumor confined to the uterus, >½ myometrial invasion |
| II |
Cervical stromal invasion, but not beyond uterus |
| IIIA |
Tumor invades serosa or adnexa |
| IIIB |
Vaginal and/or parametrical involvement |
| IIIC1 |
Pelvic node involvement |
| IIIC2 |
Para-aortic involvement |
| IVA |
Tumor invasion bladder and/or bowel mucosa |
| IVB |
Distant metastases including abdominal metastases and/or inguinal |
| lymph nodes |
| Carcinoma of the Cervix |
| IA1 |
Confined to the cervix, diagnosed only by microscopy with invasion |
| of <3 mm in depth and lateral spread <7 mm |
| IA2 |
Confined to the cervix, diagnosed with microscopy with invasion of |
| >3 mm and <5 mm with lateral spread <7mm |
| IB1 |
Clinically visible lesion or greater than A2, <4 cm in greatest |
| Dimension |
| IB2 |
Clinically visible lesion, >4 cm in greatest dimension |
| IIA1 |
Involvement of the upper two-thirds of the vagina, without |
| Parametrical Invasion, <4 cm in Greatest Dimension |
| IIA2 |
>4 cm in greatest dimension |
| IIB |
With parametrical involvement |
| IIIA/B |
Unchanged |
| IVA/B |
Unchanged |
Table 1: Gene expression profiles, prognostics and treatment options.
Cervical lymphoma
Involvement of the cervix is more frequent than the uterine body [5] and accounts for less than 1% of extranodal lymphomas. It concerns premenopausal women in 75% of cases. Unlike systemic lymphomas, B symptoms are unusual. Genital symptoms are non-specific: vaginal bleeding or discharge, pelvic discomfort, dyspareunia or urinary retention. The median tumoral size is 4 cm, sometimes invading beyond the uterus (vagina and parametrium) [2]. Because the overlying endothelium is usually unaffected, this type of cervical stromal tumors is rarely diagnosed on PAP smear. The most common histological subtype is DLBCL. Differential diagnosis includes chronic inflammatory conditions, carcinomas and primitive neuroectodermal tumors. Microscopic features include deep extension to the wall, single or multiple well-circumscribed nodules with pushing borders, sclerosis of the exocervix, spared epithelium. Ultrasound and CT reveal a diffusely enlarged cervix, whereas MRI shows a hypo intense T1 and hyper intense T2 signal. The overlying endothelium is usually unaffected [6].
Staging has proved to be one of the most important factors predicting survival (low-stages: 5-year survival rate 67-100%, high-stages: 5 years survival rate 39%) and includes clinical examination, total blood cell count, bone marrow biopsy and imaging (CT and PET-CT) following the Ann Arbor classification for extranodal lymphomas [7,8].
Standard therapy for DLBCL is R-CHOP chemotherapy with or without radiotherapy [2,8]. Since prognosis and treatment differ completely from that of squamous cell carcinoma, lymphoma should be included in the differential diagnosis in case of unusual clinical and imaging findings.
Uterine and endometrial lymphoma
Primary uterine involvement is rare, usually being part of a disseminated disease. It frequently involves both uterus and the cervix. The median age at diagnosis is in the fifth to sixth decades and bleeding is the most frequent symptom [2]. It has also been associated with chronic endometritis or long standing intra-uterine device. Uterine involvement may consist of a diffuse infiltration or a focal mass, polyp-like, thus endometrial. On ultrasound, in the diffuse infiltration pattern, the enlarged uterus appears hypoechogenic and homogenous, with preservation of the endometrium. Low signal on T1 sequences and high signal on T2 sequences are to be seen on the MRI. The diffuse enlargement with no distinct mass may help differentiation from carcinoma.
The most common subtype is DLBCL. It infiltrates all layers of the uterus without disrupting the junctional zone. Uterine involvement is associated with a higher frequency of secondary central nervous system involvement and thus requires a specific brain staging and protection [9]. Staging is the same as for cervical lymphoma and treatment consists of chemotherapy and or radiotherapy.
Breast lymphoma
Primary breast lymphomas represent less than 0.1% of breast malignancies and less than 1% of all non-Hodgkin lymphomas [10]. It usually presents as a breast mass and affects postmenopausal women, 10% have bilateral involvement and up to 30% of patients present axillary lymph node involvement [11]. Imaging is unspecific or might even show more benign features than carcinoma, as for example non-calcified breast mass on mammogram, or a hypoechogenic well-circumsed solid round mass on ultrasound. On MRI, lesions appear with low or iso- signal on T1 and high signal on T2 sequences. Calcifications, speculated lesions, architectural distorsion and nipple retraction are rarely encountered [12].
Diabetic mastopathy is a differential histological diagnosis. This benign pathology encountered among long standing type 1 diabetes women is characterized by lymphocytic mastitis with B cells surrounding the ducts and vessels and dense stromal fibrosis, which might sometimes be mislabeled as lymphoma.
Staging comprises bone marrow biopsy and CT scan. Treatment includes radiotherapy for local control with or without chemotherapy. Chemotherapy reduces relapse rate, but with no effect on overall survival so far. Primary MALT breast lymphomas have a better prognosis than DLBCL [13,14].
Ovarian lymphoma
Ovarian involvement is the most common gynecological location in the case secondary extranodal lymphoma. They tend be bilateral with peritoneal involvement and occasional supradiaphragmatic lymph nodes involvement. As for ovarian cancer, symptoms are vague and nonspecific.
Differential diagnosis includes primary epithelial tumors, sarcomas, fibromas, thecomas and Brenner tumors and finally ovarian metastasis.
On ultrasound, ovarian lymphoma appears as a well-defined, solid, homogenous mass, frequently bilateral, without ascites. There is usually no invasion of the surrounding structures and the architecture of the ovary tends to remain preserved. MRI shows a homogenous low signal on T1 weighted sequences and an intermediate to high signal on T2 sequences [15]. The FDG uptake on PET-CT is dependent on the subtype and serves as a tool to assess response to treatment.
Ann Arbor staging system has a better sensitivity than FIGO as a prognostic indicator since it differentiates unilateral or bilateral ovarian involvement. Favorable prognostic factors include unilateral involvement, smaller tumor size, early stage at presentation, DLBCL and follicular lymphoma. Treatment consists in combined chemotherapy.
Conclusion
Although primary extranodal gynaecological lymphomas are rare but differentiating them from gynaecological malignancies is crucial since they require different staging and treatment. So even it represents one case in a gynaecologist’s career, it is of diagnostic and therapeutic importance in order to avoid unnecessary surgical treatment. Cervix is the most frequent location of primary gynaecological lymphoma, whereas ovaries are the most frequent location in case of secondary gynaecological involvement. DLBCL accounts for most cases. An association with chronic inflammation has been reported for cases of cervical and uterine lymphomas. Younger age and large homogenous masses should raise attention.
Surgery should serve only to establish diagnosis if biopsy is insufficient. Staging, using FIGO and Ann Arbor System, is also an important prognostic factor. Treatment consists of chemotherapy and/or radiotherapy
Acknowledgement
Dr Daniela Padron Fragnière, Gynaecology Department, for attentive English correction.
23711
References
- Hanley K, Tadros T, Briones A, Birdsong G, Mosunjac M (2008) Hematologic malignancies of the female genital tract diagnosed on liquid-based Pap test: Cytomorphologic features and review of differential diagnosis. Diagnostic Cytopathology 37: 61-67.
- Lagoo A, Robboy S (2006) Lymphoma of the female genital tract: Current status. International Journal of Gynecological Pathology 25: 1-21.
- Rush R, Saltman A, Prica A, Breiner A, Detsky A (2017) Connecting the dots. NEJM 378: 1854.
- Hans CP (2004) Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103: 275-282.
- Salem U, Menias C, Shaaban A, Bhosale P, Youssef A, et al. (2014) Hematopoietic tumors of the female genital system: Imagining features with pathologic correlation. Abdominal Imaging 39: 922-934.
- Viera AM, Cunha T (2014) Primary lymphomas of the female genital tract: Imaging findings. Diagn Interv Radiol 20: 110-115.
- Cubo AM, Soto ZM, Cruz MÃÂÃÂÃÂâÂÂÃÂâ â≢ÃÂÃÂââ¬Ã
¡ÃÂâÂÂÃÂÃÂ, Doyague MJ, Sancho V, et al. (2017) Primary diffuse large B cell lymphoma of the uterine cervix successfully treated by combined chemotherapy alone: A case report. Medicine (Baltimore) 96: e6846.
- Kosari F, Daneshbod Y, Parwaresch R, Krams M, Wacker H (2005) Lymphomas of the female genital tract, a study of 186 cases and review of the literature. Am J Sur Pathol 29: 1512-1520.
- El-Galaly (2016) Uterine, but not ovarian, female reproductive organ involvement at presentation by diffuse large B-cell lymphoma is associated with poor outcomes and a high frequency of CNS involvement. British Journal of Haematology 175: 876-883.
- Ghetu D, Membrez V, Bregy A, Vees AG, Hottelier D (2011) Expect the unexpected: Primary breast MALT lymphoma. Arch Gynecol Obstet 264: 1323-1324.
- Wadhwa A, Senebouttarath K (2018) Primary lymphoma of the breast: A case series. Radiol Case Rep 13: 815-821.
- Avenia N (2010) Primary breast lymphomas: A multicentric experience. World J Surg Oncol 28: 53.
- Jeanneret-Sozzi (2008) Primary breast lymphoma: Patient profile, outcome and prognostic factors: A multicentre rare cancer network study. BMC Cancer 8: 86.
- Slominsky E, Korach J, Perri T, Apter S, Inbar Y (2018) Gynecological lymphoma: A case series and review of the literature. J Comput Assist Tomogr 42: 435-440.