Keywords
Oral and esophageal cancers; Tobacco-Specific Nitrosamines (TSNA); pH determination; Smokeless tobacco
Introduction
Tobacco is a leading preventable cause of death killing eight million people worldwide every year [1]. Smokeless Tobacco (SLT) consumption is an important health issue responsible for cardiovascular diseases, oral and esophageal cancers with a significant impact on quality of life [2]. Tobacco is consumed by approximately 275 million Indians resulting in over one million deaths annually. According to a national representative household survey, 75% of these 275 million people were SLT users and the remaining 25% were combined users of smoking and smokeless tobacco products. Prevalence of SLT use was twice as compared to cigarettes and other smoking products such as bidis, and were available in many forms including gutkha, panmasala, mishri, and khaini with the latter being the most common in India [3]. As per the National Family Health Survey (NFHS) by the Government of India, the use of all tobacco forms were higher in rural areas than in urban areas while smoking was more common in urban areas. Within lower socio-economic populations with low literacy levels including the scheduled castes and scheduled tribes, tobacco consumption was significantly high and was even higher for age groups above 50. The prevalence of smoking and chewing varied widely between different states and had a strong association with socio-cultural practices as well as traditional beliefs. The Global Adult Tobacco Survey (GATS) 2017 survey showed that the initiation of tobacco consumption began a year earlier as compared to GATS 2010 [4]. However, seven years gap between NFHS-3 and NFHS-2 recorded that the prevalence of tobacco consumption increase was the highest for age group 15-24 with annual growth rate of tobacco consumption between 2%-3% [5].
Disease burden
SLTs were characterized with 30 different carcinogens including cadmium, chromium, Tobacco-Specific Nitrosamines (TSNA), nickel, beryllium, benzo[a]pyrene, and other Polycyclic Aromatic Hydrocarbons (PAHs) which were resulting in high cancer rates [6].
Globally, cancers of the mouth, pharynx and esophagus attributed to SLT consumption caused a loss of more than 1.7 million Disability-Adjusted Life Years (DALYs) with more than 62 K deaths with India accounting for almost two-third of this burden. Tobacco is an important risk factor for the burden of non-communicable diseases in India and was expected to increase from 40% to 75% by 2030. The prevalence of oral cancer was the highest in India and 90% of oral cancers were caused due to tobacco consumption [7-9]. Additionally, SLT consumption causes tooth loss and decay, gum diseases and leukoplakia which results in formation of white or gray patches inside the mouth leading to cancer.
A global study on disease burden due to smokeless tobacco use in more than 100 countries concluded 4.7 million DALYs and 204 K deaths from ischaemic heart disease in addition to 62 K deaths due to cancers of the mouth, pharynx and esophagus with South-East Asia accounting for more than 85% of this burden [6]. According to the Environmental Protection Agency (US), Smokeless tobacco contains radioactive substances such as lead-210 and polonium-210 causing lung damage and contributing to lung cancer. SLT which is primarily consumed for nicotine dependence is associated with behavioral impairments including memory, attention and learning deficit. Women were more vulnerable from tobacco consumption due to increased risk of infertility, premature birth, pregnancy complication and low birth weight of infants. Other diseases like rheumatoid arthritis, diabetes, cataracts and osteoporosis were also associated with tobacco. Further, tobacco consumption was associated with problems in digestion, bone metabolism, reproductive health and overall immune system [10,11].
Oral cancer was the 11th most common cancer in the world and ranked top three in India [12]. Ninety percent of oral cancers in India were caused due to tobacco consumption given the popularity of pan-tobacco – a combination of lime, betel leaf, sun cured tobacco and areca nut. The International agency for research on cancer in 2004 classified areca nut as a human carcinogen group which mixed with tobacco increased the product risk nearly 15 times [13]. In low to middle income countries, tobacco related oral cancer contributed abundantly to lost productivity from premature deaths. Risk of developing oral cancer was reported five times higher in tobacco users as compared to non-users [14]. Several studies have confirmed that the use of tobacco and alcohol are considered as the major risk for oral cancers with the International Agency for Research on Cancer confirming that SLT consumption can lead to cancer. Chewing tobacco 10 or more times a day increased the risk of oral cancer 9.2 times [15,16] whereas products including gutka and supari increased the risk by 7.3 and 4 respectively [17]. Yet, given the immense health burden of oral cancer and one of the highest prevalence globally, India still lacks the infrastructure to accurately record the cause of deaths in a central database. The authors could only find a recent national repository providing prevalence of cancers of mouth, pharynx, esophagus, bronchial airways and lungs as a database jointly established by the Indian Council of Medical Research, Public Health Foundation of India and the Institute of Health Metrics and Evaluation [18].
Socio-demographic and geographic factors
Smoking in public is stigmatized for Indian women. However, the use of SLT is substantial [4] with the main types of SLT products including mishri, gutkha, pan with tobacco and chewing tobacco mixed with Jaggery. Prevalence of SLT in women increased with age [2] and is highest in the age group of 25-44 yrs. According to a global adult tobacco survey for Maharashtra, the fraction of urban women consuming SLT was 8.3% with 1.4% reportedly using it on a non-daily basis and 3% using two or more forms of SLT. One of the primary reasons for women using SLTs was the belief that these provide relief from bowel and abdominal problems, reduce stress and anxiety. Female laborers consumed SLTs as there was a belief that SLTs increased energy for daily workload and suppressed hunger [9]. Earlier studies reported that women do not change the amount and the frequency of SLT use during pregnancy because they believe that the teeth and gum weakening occurring during pregnancy can be prevented by consumption of SLTs [19]. The misconception that SLTs are characterized by medicinal properties result in wide use among Indian women. In 2016, the global adult tobacco survey [3] estimated the prevalence of smokeless and smoked tobacco use in India among those aged ≥ 15 years was 21.4% and 10.7%, respectively. India is one of the four countries that shared more than 50% of the 6.3 million deaths and 155 million DALYs attributable to tobacco use worldwide [20]. Approximately one person out of ten between 13 and 15 years consumed tobacco with half of them starting tobacco consumption before age 10. Another study found that lack of knowledge and awareness on tobacco health risks is highly significant making them the main target groups for tobacco companies. According to a National sample survey organized by the Indian government, 5500 new users were added daily as SLT consumers leading to 2 million new users every year [21]. Global youth tobacco survey [22] revealed high prevalence of tobacco consumption in Bihar and North Eastern states and a low prevalence in Haryana, Delhi, Himachal Pradesh, Andhra Pradesh, Karnataka, Tamil Nadu Delhi, Goa, Haryana and Punjab. Reported factors for initiation of tobacco use in children include friends (61.69%), creating social impression and reputation (5.19%), parents (11.03%), hobbies (14.30%) and siblings (7.79%) [23].
Several factors including traditional values, urbanization, affordability and resulting disease burden from consumption of SLTs are discussed in this study. The objectives of this study are a) analyzing state level data on lung and oral cancer deaths in India, and b) evaluating causation between tobacco use and cancer deaths by analyzing data on chemical characterization of popular tobacco products available in India.
Materials and Methods
Chemicals
TSNAs were analyzed by using Kentucky Reference cigarettes (KY2R4F) and Reference Tobacco Product (CRP 2.1) obtained from Kentucky Tobacco Research and Development Center (Lexington, KY) and used as received. The N-Nitrosopiperidine (NPIP) and N-Mitrosomorpholine (NMOR) were purchased from Sigma Aldrich with 99.5% and 100% purity respectively. High Performance Liquid Chromatography (HPLC) grade Nnitrosodimethylamine (NDMA) (92.62% purity; Synzeal) and Nnitrosopyrrolidine (NPYR) (98.05% purity; Clearsynth Research Centre) were purchased and stored appropriately. And the mobile phase and diluent such as formic acid, water (Avantor, India) and methanol (Biosolve, India) HPLC grade from Sigma Aldrich was purchased for analysis. Five varieties of SLT products were obtained from three different locations including Mumbai, Hyderabad and Surat. These were procured from the open market in India. Analytical weighing balance from Shimadzu was used for weighing of samples and other purposes as required.
Sample preparation
Measurement of total moisture content and product pH: For total moisture determination, 1 gm of each SLT sample was weighed and subjected to Oven evaporation/volatilization method [24]. Pre-weighed SLT samples are heated in an oven at 100?C for three hours. Followed by the sample allowed to cool in a desiccator for at least thirty minutes and these samples were assessed for reweighting to check the amount of mass loss as OV %. To determine the pH of SLT products, 1 gm of each sample were ground and mixed with milli-Q water then degassed using a magnetic stir. The supernatant is collected in beaker for pH determination [24], before performing the pH electrode calibrated using three different pH buffers (4.1, 7.4 and 9.0). The pH and moisture were determined in duplicates for all the SLT products.
Quantification of tobacco-specific N-nitrosamines: All these reference standards and SLT products were dissolved in citratephosphate buffered L-ascorbic acid (Sigma, MO) preparation by keeping 60 minutes agitation. Then the aqueous portion of extract eluted by using solid phase liquid elution column by passing through a column with 150 mL dichloromethane and collected the eluent. Each eluent subjected to Gas chromatography-thermal energy analysis (GC-TEA) (Health Canada T-111) for analysis of TSNAs including Nnitrosonornicotine (NNN), 4-[methylnitrosamino]-1-[3- pyridyl]-1-butanone (NNK), N-nitrosoanatabine (NAT) and Nnitrosoanabasine (NAB) [25]. GC maintained a maximum temperature of 220?C and TEC interface maintained at 240?C. All the samples were injected to the GC-TEA system with 1.5 μ l. All the nitrosamine constituents analyzed were performed in duplicates on each SLT product and reference standards. The data was processed in R language for visualization using several packages including gg plot 2, stamen maps and tidy verse and more which are included in the references.
Results and Discussion
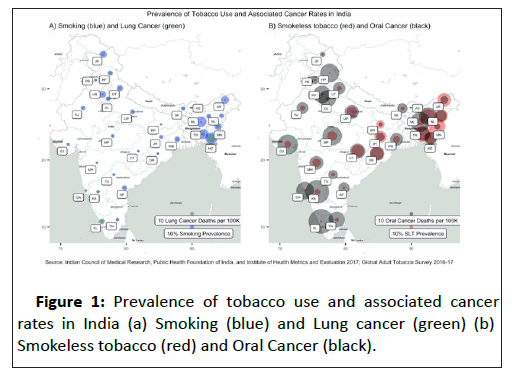
Historical data on the prevalence of a) smoking and lung cancer, and b) smokeless tobacco and oral cancer are illustrated in Figure 1 with either tobacco use closely associated with occurrence of cancer.
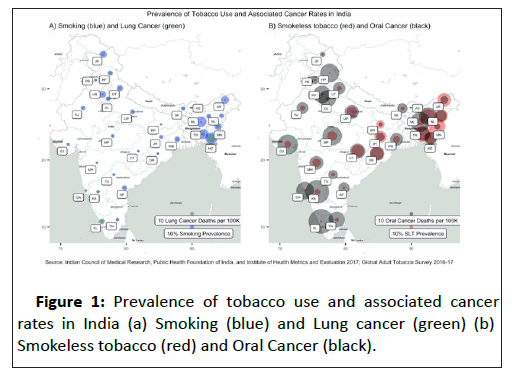
Figure 1: Prevalence of tobacco use and associated cancer rates in India (a) Smoking (blue) and Lung cancer (green) (b) Smokeless tobacco (red) and Oral Cancer (black).
The descriptive statistics for oral cancer (including pharyngeal cancer) and lung cancer (including bronchial cancer) are illustrated in Table 1.
| |
Min |
Max |
Mean |
SD |
Skew |
kurtosis |
SE |
| SLT prevalence% |
3.10 |
48.50 |
21.72 |
14.42 |
0.39 |
-1.32 |
2.63 |
| Smoking prevalence% |
3.80 |
34.40 |
13.84 |
7.79 |
1.00 |
0.30 |
1.42 |
| Lung cancers per 100 K |
3.77 |
24.81 |
7.52 |
4.06 |
2.82 |
8.71 |
0.74 |
| Oral cancers per 100 K |
10.80 |
74.01 |
40.56 |
15.91 |
0.11 |
-0.71 |
2.90 |
| Moisture% |
5.92 |
46.00 |
18.50 |
15.96 |
0.64 |
-1.58 |
4.61 |
| NAB (ng/g) |
0.00 |
3712.00 |
525.92 |
1033.66 |
2.38 |
4.55 |
298.39 |
| NAT (ng/g) |
0.00 |
21062.00 |
2805.67 |
5893.20 |
2.43 |
4.70 |
1701.22 |
| NIC (µg/g) |
2514.00 |
24836.00 |
6876.42 |
5908.35 |
2.26 |
4.16 |
1705.59 |
| NNK (ng/g) |
0.00 |
10448.00 |
1268.08 |
2990.39 |
2.36 |
4.42 |
863.25 |
| NNN (ng/g) |
0.00 |
35603.00 |
5559.92 |
9759.59 |
2.37 |
4.51 |
2817.35 |
| pH |
6.48 |
10.60 |
8.80 |
1.21 |
-0.67 |
-0.72 |
035 |
Table 1: Descriptive statistics including range, mean, Standard Deviation (SD), skewness, kurtosis and Standard Error (SE) for tobacco use, lung and oral cancers rates across India along with nitrosamines, Nicotine (NIC) and pH levels for tested products.
Prevalence (rate) of lung and oral cancers for India range between 25 and 4 per 100 K for Mizoram (MZ) and Jharkhand (JH), and 74 and 10 for Kerala (KL) and Bihar (BR), respectively. Whereas, prevalence (%) of smoking and SLT use are between 35 and 4% for MZ and Maharashtra (MH), and 49% and 3% for Tripura (TR) and Himachal Pradesh (HP), respectively. Although the prevalence of tobacco use is low for South-western states of Goa (GA), KL and Karnataka (KA), oral cancer rate is significantly high, requiring further analysis of underlying factors including alcohol use. This discrepancy may also be due to better disease data recorded in state registries as compared to the Northern and Eastern states as this is one of the earliest attempts to establish centralized data registries for disease and substance use across Indian states.
There is sufficient consensus [26,27] that TSNAs are primarily responsible for harm caused by tobacco products associated with high causality of cancers of the mouth, pharynx, esophagus and respiratory system. The highest total TSNA levels (NAB+NAT+NNN+NNK) were observed for Mishri products with a maximum of 70.4 mg/g with the lowest level for Paan-tobacco mixture at 0.06 μg/g. Snus, which is a popular harm reduction alternative, was characterized by 5.4 μg/g while gutkha and khaini products contained approximately 4.7 μg/g and 2.5 μg/g, respectively. The highest nicotine content was observed for Snus at 27500 μg/g with a range between 3000 and 8400 μg/g for all other products tested. Similarly moisture content was also highest for Snus at 23.3% and between 18.5 to 19.8 for Khaini products. Whereas moisture content for all other products was in the range of 3% to 7%. The lowest and highest pH values were observed for Mishri products at 6.48 (MMH) and 10.6 (HMH) while the values for Snus and all other products were observed to be within 7.8 and 9.6.
Although nitrosamines are present in most food products primarily a byproduct of preservatives and additives, the level is usually significantly lower as compared to tobacco products. TSNAs including NAB, NAT, NNN and NNK are declared carcinogenic by expert toxicologists. The level of TSNAs can provide guidance on the risk factor associated with specific tobacco products (Figure 2).

Figure 2: Relative product variability of Tobacco-Speci ic NNitrosamines (TSNAs), Nicotine (NIC), pH and moisture content (%) reported for 11 popular SLT brands representing 4 types of smokeless chewing tobacco products and Snus commercially available on the Indian market and, NNK and NNN levels in ng/g for all products tested in this study.
The results show a smoking rate was higher for Northern and North-East states of India while SLT use is higher in the northeast, central and western states. Although the south-west region including GA, KA and KL showed relatively lower tobacco use, oral cancer rates for these states were among the highest in India. These differences need to be analyzed further by exploring factors such as alcohol use as well as any genetic factors.
Conclusion
Challenges for THR aimed at SLT use in South East Asian countries like India remain incomprehensibly accountable to socio-cultural and economic complexities. Although reduced risk products such as Snus, ENTs Nicotine Replacement Therapy (NRT) along with cessation initiatives based on Smartphone use provide some clues, THR for these Asian countries need an improvised strategy by first understanding existing challenges. Preliminary national census data suggests that oral cancer is a much bigger health risk than lung cancer requiring hybrid cessation models with equal if not larger share of cessation focusing on SLT use as compared to smoking. Further, our study emphasizes the urgent need to re-innovate THR products along with early interventional and detection technologies for South East-Asia, especially considering that underprivileged population sub-groups form majority of patients diagnosed with oral cancer which is a direct health burden from consumption of SLT products characterized with carcinogenic chemicals.
Conflict of Interest
The authors would like to report no existing or potential conflicts of interest.
40140
References
- Mehrotra R, Yadav A, Sinha DN, Parascandola M, John RM, et al. (2019) Smokeless tobacco control in 180 countries across the globe: Call to action for full implementation of WHO FCTC measures. Lancet Oncol 20(4): e208-e217.
- Mishra GA, Pimple SA, Shastri SS (2012) An overview of the tobacco problem in India. Indian J Med Paediatr Oncol 33(3):139-145.
- Sundararaman T (2017) Global adult tobacco survey, India. Ministry of Health and Family Welfare Government of India. ISBN : 978-81-937917-0-7.
- Singh LL, Paswan B, Singh SK, Das KC, Ram F,et al. (2010) Global Adult Tobacco Survey; GATS India International Institute for Population Sciences. Ministry of Health and Family Welfare G of I.
- Gopinathan P, Kaur J, Joshi S, Prasad VM, Pujari S, et al. (2018) Self-reported quit rates and quit attempts among subscribers of a mobile text messaging-based tobacco cessation programme in India. BMJ Innov 4:147-154.
- Siddiqi K, Shah S, Abbas SM, Vidyasagaran A, Jawad M, et al. (2015) Global burden of disease due to smokeless tobacco consumption in adults: Analysis of data from 113 countries. BMC Med 13:194.
- Pednekar MS, Nagler EM, Pawar P, Sorensen G (2016) The Prevalence of Tobacco Use among Manufacturing Workers: Findings from the Baseline Survey of the Mumbai Worksite Tobacco Control Study. J Prev Med 1:3.
- Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L (2003) Tobacco use in India: Prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tob Control 12(4):e4.
- Gupta PC, Ray CS, Murti PR, Sinha DN (2014) Rising incidence of oral cancer in Ahmedabad city. Indian J Cancer 51(Suppl 1):S67-72.
- Bonnie RJ, Stratton K, Kwan LY (2015) Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. National Academies Press (US), ISBN-10: 0-309-31624-3.
- Petersen PE (2003) The World Oral Health Report 2003: Continuous Improvement of Oral Health in the 21st Century--the Approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 31(Suppl 1):3-23.
- Warnakulasuriya S, Trivedy C, Peters TJ (2002) Areca nut use: An independent risk factor for oral cancer. Br Med J 324(7341):799-800.
- Sinha DN, Abdulkader RS, Gupta PC (2016) Smokeless tobacco-associated cancers: A systematic review and meta-analysis of Indian studies. Int J Cancer 138(6):1368-1379.
- Gupta PC, Sreevidya S (2004) Smokeless tobacco use, birth weight, and gestational age: Population based, prospective cohort study of 1217 women in Mumbai, India. Br Med J 328(7455):1538-1540.
- Mallath MK, Taylor DG, Badwe RA, Rath GK, Shanta V, et al. (2014) The growing burden of cancer in India: Epidemiology and social context. Lancet Oncol 15(6):e205-12.
- IHME. Global Burden of Disease (GBD). Data Visualization. GBD Compare. Viz Hub.
- Singh S, Mini GK, Thankappan KR (2015) Tobacco use during pregnancy in rural Jharkhand, India. Int J Gynecol Obstet 131(2):170-173.
- Gakidou E, Afshin A, Abajobir AA, Abate KH, Abbafeti C, et al. (2017). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 390(10100):1345-1422.
- Gupta PC (1999) Gutka: a major new tobacco hazard in India. Tob Control 8(2):134.
- Bagchi NN, Ganguly S, Pal S, Chatterjee S (2014) A study on smoking and associated psychosocial factors among adolescent students in Kolkata, India. Indian J Public Health 58(1):50-53.
- Monika S, Dineshkumar T, Priyadharini S, Niveditha T, Priyadharshini SK, et al. (2020). Smokeless tobacco products (STPs) harbour bacterial populations with potential for oral carcinogenicity. Asian Pacific J Cancer Prev 21(3):815-824.
- Wu J, Joza P, Sharifi M, Rickert WS, Lauterbach JH (2008) Quantitative method for the analysis of tobacco-specific nitrosamines in cigarette tobacco and mainstream cigarette smoke by use of isotope dilution liquid chromatography tandem mass spectrometry. Anal Chem 80(4):1341-5.
- Xue J, Yang S, Seng S (2014). Mechanisms of cancer induction by tobacco-specific NNK and NNN. Cancers (Basel) 6(2):1138-56.
- Straif K, Weiland SK, Bungers M, Holthenrich D, Taeger D, et al. (2000). Exposure to high concentrations of nitrosamines and cancer mortality among a cohort of rubber workers. Occup Environ Med 57(3): 180–187.