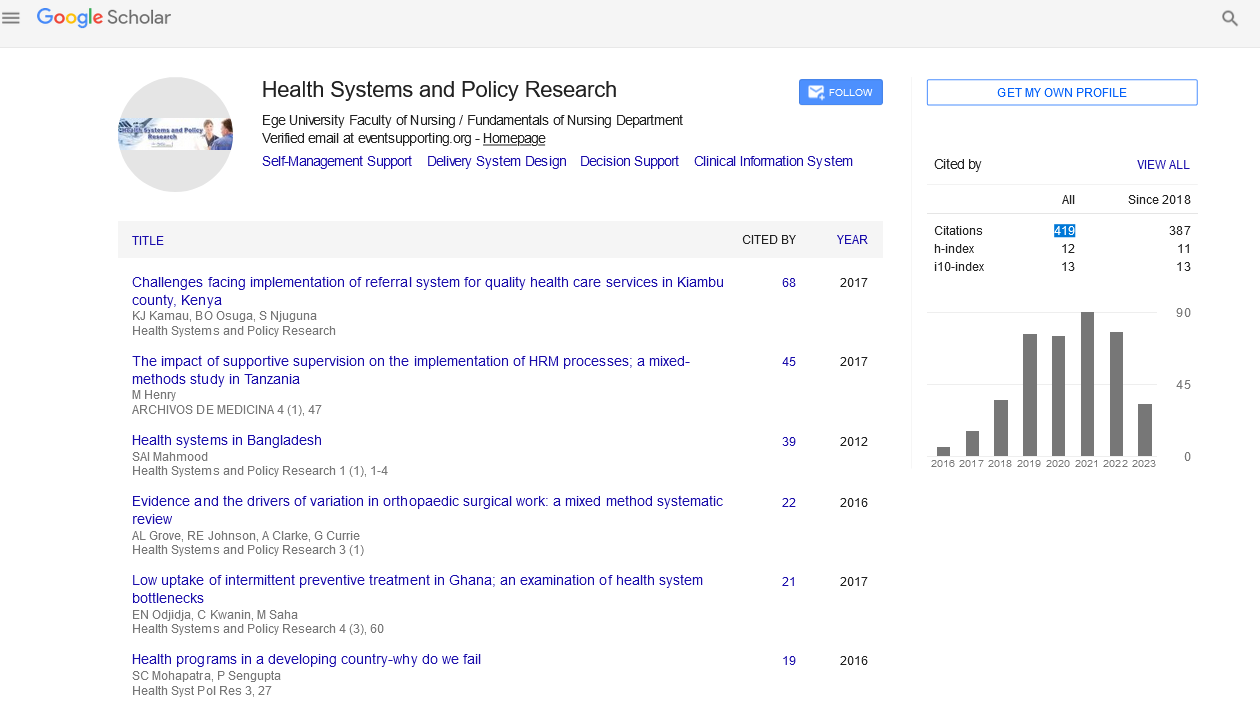
Perspective - (2023) Volume 10, Issue 1
Health Care Reform Fixes Instead Of a Long-Term Strategy In 2014
Kishan Gupta*
Department of Health care, University of California, United States
*Correspondence:
Kishan Gupta, Department of Health care, University of California,
United States,
Email:
Received: 02-Jan-2023, Manuscript No. Iphspr-22-13390;
Editor assigned: 05-Jan-2023, Pre QC No. Iphspr-22-13390;
Reviewed: 19-Jan-2023, QC No. Iphspr-22-13390;
Revised: 23-Jan-2023, Manuscript No. Iphspr- 22-13390 (R);
Published:
31-Jan-2023, DOI: 10.36648/2254-9137.23.10.170
Abstract
The Health Minister began implementing legislative amendments that both directly and indirectly influence primary healthcare towards the end of 2013. Many organisations of medical professionals, notably family medicine doctors, strongly opposed the revisions. The latter mainly criticised the formal inclusion of specialists in paediatrics and internal diseases into PHC within the statutory health care system, which in practise meant that these two groups of specialists were no longer required to specialise in family medicine from to enter into contracts with the public payer and would be able to set up solo PHC practices something over which family medicine physicians used to have a monopoly. They contended that internists and paediatricians lacked the qualifications to serve as PHC doctors.
Keywords
Primary health care; Health care legislation; Health care reform; Family medicine
INTRODUCTION
The powerful Family medicine professionals' opposition to the change, which is backed by two powerful organisations, might jeopardise future policy implementation [1]. And so guarantee the delivery of an extensive and well-coordinated PHC [2]. Given the lack of family medicine professionals, the administration said that the proposed step was required to ensure the supply of PHC in the future [3]. The proposed modification was also backed by a few organisations of medical experts [4]. The primary argument in favour was that it may increase access to PHC, particularly for young people [5]. Although this was not the focus of the criticism or even a discussion of policy, the plan neglected the growing healthcare requirements of elderly people, who were the main beneficiaries of PHC services [6]. As is customary for modifications in the Polish healthcare system among other things, the policy was enacted by the Parliament in March April 2014 without consultation with the important stakeholders [7]. Council for the accrediting of qualifications in the profession [8].
Discussion
Each member state shall, subject to the provisions relating to acquired rights, make the pursuit of such activities within the framework of its national social security system conditional upon possession of evidence of formal qualifications referred to in Annex V of the Directive, as provided for in Article 29 of this Directive, which governs the pursuit of professional activities by general practitioners. In Poland, a family medicine certificate serves as proof of such official credentials [9]. Since the Directive's passage, PHC services must be provided through contracts with the Polish Social Health Insurance System [10]. National Health Fund (NHF), provided that the applicant has such a diploma. On the basis of the aforementioned rules pertaining to the acquired rights, PHC physicians who do not hold a diploma in family medicine but who have worked as PHC physicians for at least ten years previous to the enactment of the Directive have been exempted. Up until 2017, any other PHC doctors who lacked this credential and wanted to practise in the social health insurance system also had to become family medicine specialists. Due to Poland's low family medicine physician density (one per 3500 people as opposed to the one per suggested by experts) and the limited amount of time available to complete family medicine specialty In 2017, it was clear that there would be a family physician shortage, which would jeopardise the delivery of PHC. Given this threat and the potential negative effects that the ageing of the population may have on the employment opportunities for this group of specialists in the future, the Minister of Health proposed at the end of 2013 to make it legal for all internal disease and paediatric specialists to work in the statutory healthcare system as PHC physicians and to establish their own practises. The new policy, according to some policy analysts, amounts to a de facto return to the prior arrangements, when other medical specialities, including as internists and paediatricians, were permitted in PHC. It was also indicated that the mentioned policy was not supported by any evidence.
Conclusion
Although it is doubtful that the reform is supported by any thorough analyses, many European countries for example, those in Refs involve internists, paediatricians, and other medical specialists in the delivery of PHC, and many of these nations rank highly in this regard for example, in terms of its accessibility, continuity, and coordination. Also, paediatricians and internists were formally included in the provision of PHC not only in the communist times but as late as which is when the 2004 Act on Health Care Services Financed by Public Sources was amended, requiring them to get a family medicine diploma until 2017. This indicates that some of them may have a wealth of experience working in PHC settings and should be qualified to offer patients high-quality PHC. Additionally, the formal integration of paediatricians into PHC is likely to enhance the standard of care for kids and teenagers: if there are more paediatricians working in PHC, it may be more likely that a child accessing PHC will be seen by one, and the standard of care for this patient group may rise. However, because internists and paediatricians are only permitted to provide medical services that fall under the purview of their incorporation into PHC will not increase access to family medicine generally because of their separate specialty see the Ministry of Health's view on this.
Acknowledgement
None
Conflict of Interest
None
References
- Bar Zeev N (2020) Moss W: Encouraging results from phase 1/2 COVID-19 vaccine trials. Lancet 6736: 31611.
Indexed at, Crossref, Google Scholar
- Day M (2020) Covid-19: Experts criticise claim that remdesivir cuts death rat. BMJ 370: m2839.
Indexed at, Crossref, Google Scholar
- Dyer C (2020) Pandemic preparedness: doctor leads campaign for UK government to release report. BMJ 369: m1732.
Indexed at, Crossref, Google Scholar
- Gilson L (2006) Trust and health care: theoretical perspectives and research needs. J Health Organi Manag 20: 359–75.
Indexed at, Crossref, Google Scholar
- Horton R (2020) Offline: Covid-19 and the NHS – "a national scandal". Lancet 395: 1022.
Indexed at, Crossref, Google Scholar
- Iacobacci G (2020) Covid-19: UK must prepare now for winter peak or risk many more deaths, scientists warn. BMJ.
Indexed at, Crossref, Google Scholar
- Iacobacci G (2020) Covid-19:Government is criticized for ‘scandalous’£ 10bn spent on test and trace. BMJ.
Indexed at, Crossref, Google Scholar
- Iacobucci G (2020) Covid-19: PM promises inquiry but says it won't happen during pandemic. BMJ.
Indexed at, Crossref, Google Scholar
- Limaye R, Sauer M, Ali J (2020) Building Trust While Influencing Online COVID-19 Content in the Social Media World. Lancet Digit Health 2: e277-e278.
Indexed at, Crossref, Google Scholar
- Mullard A (2020) Flooded by the torrent: the COVID-19 drug pipeline. Lancet 395: 1245-1246.
Indexed at, Crossref, Google Scholar
Citation: Kishan Gupta (2023) Health Care Reform Fixes Instead Of a Long-Term Strategy In 2014. Health Sys Policy Res Vol. 10 No. Issue 1:170