Richard Beaumont1, Iris Garcia2, Marie Josee Valladares2, Diana Medina2, Sinthia Solorzano2*, Oscar Perez3, Yasmin Gomez3 and Miriam Hernandez4
1General Surgery, Universidad Nacional Autónoma de Honduras, Honduras
2UNAH Doctorates in Medicine and Surgery, Universidad Nacional Autónoma de Honduras, Honduras
3Physicians for Social Service WCC San Marcos, Sta. Barbara, USA
4Medicine and Surgery UNICAH, Universidad Católica de Honduras, Honduras
*Corresponding Author:
Sinthia Solorzano
UNAH Doctorates in Medicine and Surgery, Universidad Nacional Autónoma de Honduras, Honduras
Tel: 50431715887
E-mail: sinthiasolorzano@gmail.com
Received date: 19 September 2016; Accepted date: 03 October 2016; Published date: 08 October 2016
Citation: Beaumont R, Garcia I, Valladares MJ, et al. Hemobilia a rare entity: Case report and literature review. Ann Clin Lab Res. 2016, 4: 4.
Keywords
Hemobilia; Hepatic artery; Cholecystitis
Introduction
Hemobilia is defined as the presence of blood in the biliary tree [1]. Caused by an abnormal communication between the blood vessels and bile ducts [2]. This condition is characterized by the classic triad of jaundice, pain in the right upper quadrant and upper gastrointestinal bleeding.
It occurs mainly post-trauma and iatrogenic causes, diagnosis should be suspected by history, making differential diagnoses.
Then a case of female patient treated at the hospital area of Puerto Cortes with a recent history of cholecystectomy who develops porteriormente hemobilia classic triad, right upper quadrant pain, obstructive jaundice, upper gastrointestinal bleeding and secondary anemia. Who it was performed as definitive treatment ligation of the right hepatic artery.
Case Presentation
Female patient, 42 years old, literate, housewife, with surgical history of open cholecystectomy 25 days of evolution, is presented to the emergency hospital area of Puerto Cortes, with a history of abdominal pain 2 hours of evolution, located in epigastrium, moderate intensity, continuous, without irradiation, without mitigating or exacerbating, accompanied by jaundiced tint, shaking fever, and vomiting. Physical examination has stable vital signs, jaundiced mucous membranes and sclera in abdomen with drain bile presence of small amount hematic fluid, with pain on deep palpation in epigastric no signs of peritoneal irritation. Admission is decided to complete imaging studies.
USG reporting tabicada subcapsular collection of 366 cc about to rule biloma and requested to perform percutaneous drainage is performed.
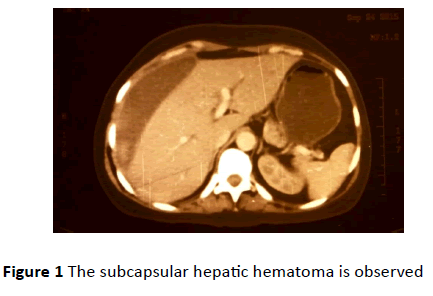
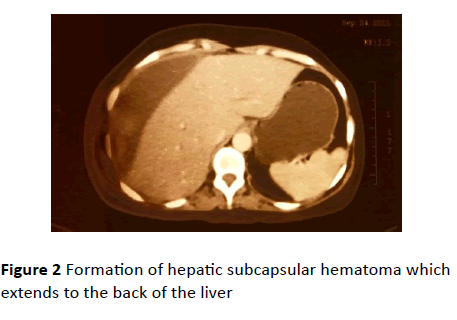
Abdominal CT is performed which reports subcapsular hepatic hematoma located in the right subphrenic space which extends to the posterior region of the liver, as shown in Figures 1 and 2.
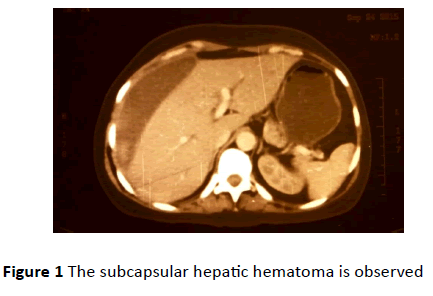
Figure 1 The subcapsular hepatic hematoma is observed
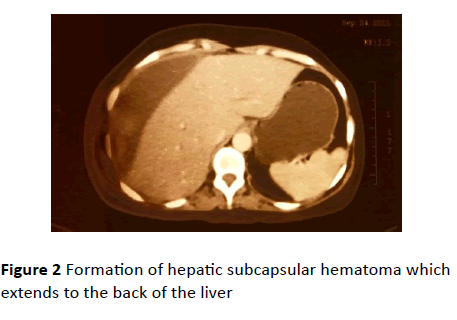
Figure 2 Formation of hepatic subcapsular hematoma which extends to the back of the liver
Five days later patient starts with upper gastrointestinal bleeding with melena, CBC reported severe anemia with HGB: 6.2 mg/dl HCT: 18.0, continuing with pain in the right upper quadrant and jaundiced tint. Chemical reporting is done TGO: 265.5 U/L, TGP: 254.8 U/L, BT: 2.8 mg/dl, BD: 2.3 mg/dl and BI: 0.5 mg/dl, TP: TPT 16 sec and 58 sec. Percutaneous drainage was performed without success.
Patient is transfused unit packed red cells, however upper gastrointestinal bleeding continues intermittently, hypotension and jaundiced, transfusion of 2 units of packed red cells over is decided. Table 1 shows the evolution of laboratory data is shown.
| Exams |
09.20.15 |
09.25.15 |
09.28.15 |
09.30.15 |
09.10.15 |
10.13.15 |
10.16.15 |
10.18.15 |
| Hemoglobin |
8.7 mg/dl |
9.8 mg/dl |
6.2 mg/dl |
|
7.3 mg/dl |
7.4 mg/dl |
8.1 mg/dl |
7.7 mg/dl |
| hematocrit |
26.4% |
26.7% |
18% |
|
7.3% |
21% |
|
|
| platelets |
316 10'3/ul |
511 10'3/ul |
|
|
|
559 10'3/ul |
|
|
| Total bilirubin |
1.4 mg/dl |
|
|
2.8 mg/dl |
|
|
|
|
| Direct bilirubin |
1.0 mg/dl |
|
|
2.3 mg/dl |
|
|
|
|
| Indirect bilirubin |
0.4 mg/dl |
|
|
0.5 mg/dl |
|
|
|
|
| TGO |
219.4 u/l |
|
|
265.5 u/l |
|
|
|
|
| TGP |
259.2 u/l |
|
|
254.8 u/l |
|
|
|
|
| Prothrombin time |
|
14 sec |
|
16 sec |
|
|
|
|
| Thromboplastin Time |
|
39 sec |
|
58 sec |
|
|
|
|
Table 1 Data laboratory
Patient despite being transfused, not improving their anemic syndrome and upper gastrointestinal bleeding continues intermittently, it decides to take operating room to explore the bile duct. Intraoperatively the dilated common bile duct with the presence of a blood clot approximately 8 cm × 6 cm in size, to be removed active bleeding profusely shown and proceeds to the ligation of the right hepatic artery which gives bleeding was observed and hemobilia checks the diagnosis. Following surgery, the patient remains in the hospital until levels of liver and hemoglobin tests were within normal values.
Currently patient has a favorable evolution without relapse or severe sequelae after surgery. It can be concluded that the patient had a box hemobilia shown by clinical presenting the triad of jaundice, abdominal pain and gastrointestinal bleeding intermittently and being confirmed intraoperatively, showing clinical improvement after surgery.
Discussion
The hemobilia is a condition that must be considered in the differential diagnosis of a patient with upper gastrointestinal bleeding intermittently, as Cumana mentioned in his article in 2011, the hints that should be suspected hemobilia in those presenting bleeding colestacis high with signs of digestive.
In the case of the patient presented earlier, she had a history of cholecystitis chronic calculous why he underwent open cholecystectomy and subsequently began with the symptoms of abdominal pain in the right upper quadrant, jaundice and upper gastrointestinal bleeding intermittently, confirming the triad appears in the hemobilia mentioned in the literature.
Due to the infrequency of hemobilia that was not the primary diagnosis of the patient, imaging studies were required to rule out other causes of gastrointestinal bleeding and other studies to suspect in the pathology coupled with the classic triad presented by the patient.
Once established and suspected diagnosis due to poor patient presenting the significant declines in digestive bleeding secondary to hemoglobin, we proceeded to perform surgery in order to stop the bleeding.
Ligation of the hepatic artery was the surgical procedure performed with great success, as Rincón mentioned in your article, the treatment of hemobilia is essentially surgical and according to the site where this specific bands of blood vessels conducted and bile canaliculi, segmental resections or ligation of the hepatic artery.
Summary
Hemobilia is a condition that occurs in clinical practice infrequently, have different etiologies. It is defined by the presence of blood in the bile duct. Characterized by the classic triad of jaundice, right upper quadrant pain and upper gastrointestinal bleeding. For diagnosis we can use various complementary, imaging and endoscopic studies. Treatment is generally surgical hemobilia. For postoperada female patient who developed chronic cholecystitis obstructive jaundice, with upper gastrointestinal bleeding and abdominal pain. It was performed as definitive treatment ligation of the right hepatic artery. With satisfactory evolution.
Literature Review
Hemobilia is defined as the presence of blood in the biliary tree [1]. Caused by an abnormal communication between the blood vessels and bile ducts [2]. First described by Francis Glisson in 1654, a young deceased with pain right upper quadrant followed by massive upper gastrointestinal bleeding. Antoine Portal in 1977 was the first to recognize a case of antemortem hemobilia. Quincke describes a case of hemobilia in 1871, emphasizing clinical features. Kehr performed the first surgery in a case of hemobilia in 1903 identifying an aneurysm of the hepatic artery carrying broken artery ligation. The term Hemobilia was first coined by Sandblom in 1948 in a publication by bleeding from posttraumatic biliary tract: Hemobilia traumatic few years later was Walter who described the use of arteriography with embolization for the treatment of bleeding [3].
This condition is characterized by the classic triad of jaundice, right upper quadrant pain and upper gastrointestinal bleeding. Among the most important etiologies in order of frequency are: liver trauma (accidental or iatrogenic), inflammatory causes (acute and chronic cholecystitis), infection (cholangitis, liver abscess, parasitic infections), and vascular diseases (aneurysms, vasculitis, arteriovenous malformations) [4]. Even tumors or coagulation disorders [5]. Approximately 2/3 hemobilia cases are due to medical interventions. Liver biopsy and percutaneous transhepatic cholangiography are the most common causes of damage to the liver vasculature resulting in hemobilia [6].
Hemobilia diagnosis is difficult in daily practice; Recently with the development of interventional radiology has reduced the number of surgeries, transarterial embolization by obtaining success rates between 80% to 100% [7].
In patients with a clinical suspicion of hemobilia, endoscopy is the first test since it allows objectify bleeding through the papilla of Vater is performed [6]. However, only 12% of endoscopies are diagnostic, which means that other complementary techniques, often necessary. CT angiography is sensitive and specific providing information about the patient 's vascular anatomy and visualization of possible anatomical variants. Angiography plays an important role in managing hemobilia for both diagnosis and treatment [3].
The management of hemobilia depends on the severity of the bleeding, the underlying disease, age and general condition of the patient. The definitive treatment of removing the cause of bleeding, including liver resection, linked directly or packing of bleeding vessels, cholecystectomy, pancreatic resection, resection of the aneurysm, fistula closure or other. False aneurysms can be treated by embolization or balloon tamponade. In general, selective arterial embolization is recommended whenever possible, reserving surgery for cases of failure or complication of embolization, the tumor unresectable and cholecystitis [8].
Conclusion
Management and prognosis of hemobilia depends on the clinical and the speed with which the box is suspected.
The treatment is to identify the cause and give management, which is usually achieved by surgical procedures.
17243
References
- Arrojo B, Canhoto M, Barata P (2010) Hemobilia after pseudoaneurysm of a right hepatic artery branch. Spanish magazine digestives diseases 102: 386-387.
- Córdoba A, Monterrubio VA, Well I, Cork SG (2007) Hemobilia: a rare cause of massive gastrointestinal bleeding. Cir Esp 82: 368-372.
- Beltran VF, Castillo EA, AH Hidalgo (2005) Hemobilia secondary to pseudoaneurysm broken: case report. Rev. gastroenterol 35.
- Panno C, Gutierrez S, Echeverria R, Garbe C, Milocco M, et al. (2015) Hemobilia secundarria to the hepatic artery pseudoaneurysm. ACTA Latin American Gastroenterology 45.
- Hernandez GR (2003) Hemobilia: a case, complications follow. Ciruj Cir 71: 137-144.
- Cumana R, Fernandez C, Isern AM, Bronstein M, Senior M, et al. (2011) Hemobilia: imaging: A report of two cases. GEN magazine 65: 132-135.
- Dousset B, Sauvanet A, Bardou M, Legmann P, Vilgrain V, et al. (1997) Selective Indications for surgical iatrogenic hemobilia. Surgery 121: 37-41.