Keywords
High blood pressure; Activity; Stress at workplace; Obesity
Introduction
Cardiovascular diseases are the leading cause of death in the world. High blood pressure (HBP), still called "silent killer", with discrete manifestations but consequences very often serious and sometimes fatal, is the first risk factor [1]. More than one over three adults suffers from high blood pressure, a condition that accounts for about half of the deaths from stroke and heart disease. Responsible for 7.5 million deaths in 2004 [1], 25% of the hypertensive population was recorded in 2005 and 30% are expected in 2025 [2].
In Africa, the situation is close to that of the Occident; in fact, there are 80 million people with high blood pressure today, and in 2025 we expect as twice as much; Africans have a greater genetic risk, with an earlier HBP apparition, more severe and more difficult treat [3]. Many people are remaining undiagnosed [1]. Its expansion in Africa would depend on globalization, lifestyle changes, dietary habits and professional activities. In Cameroon, high blood pressure is the most common cardiovascular disease, with a prevalence of 20%. Affecting one over four adults, it is the leading cause of death and the leading cause of acquired disability from adults [4]. The prevalence reached in companies 24,8% [5].
In the ALUCAM group, high blood pressure is the leading cause of long-term absenteeism, with recrudescence of new cases and registration of fatal outcomes by stroke or cardiac arrest. HBP appears to be more prevalent among workers in operational sectors who are theoretically more active than others. This seems to be contradictory with current scientist literature data, which refers to physical activity and normal BMI as protective factors for HBP [6]. There are therefore other risk factors present in the environment of these workers related to their activity.
Subject and methodology
This is a case-control study carried out between January 1st and September 30th, 2013, which concerned all ALUCAM group’s employees (n=637) working in the industrial site, a subsidiary of the Rio Tinto Alcan global group. The factory is located at Edea in Cameroon, in the coastal region. We have used two questionnaires to collect data about individual and company’s determinants on the one hand. On the other hand, the assessment of psychosocial risk by the Karasek model. The database of the occupational health center has completed the collection. Each worker is a part of a similar exposure group (SEG), made up of people undergoing the same professional constraints and nuisances [7-11].
The activity is all physical (muscular and visual effort), mental (memory) and even social (collegiality) solicitations of the individual, used to carry out the task. It constitutes "real work", which is the way that the task named also "prescribed work" is performed. There is always a gap between the “real work” and the “prescribed work”. In this perspective, acting on the workload means intervening on the determinants linked to it [12]. The term "active" designated workers in the operational sector, exposed to the nuisances and constraints of the factory. The administrators were characterized by the sedentary nature of their work. The identification of each was directly dependent to the SEG. We will consider as educated workers with a higher or secondary level of education, and as older workers, all those over 45 years old. We will retain the medians of the following Karasek scores as study references: Psychological Demand: 21, Decisional Latitude: 71, Social Support: 24. The statistical test used was that of Chi2. A value of P<0.05 shows a statistically significant relationship. An Odds ratio> 1 marks the strength of the link. The data capture and analysis was done from Epi-info version 3.5.4 of July 30, 2012. Informed consent of each participant was obtained beforehand.
Results
The average age of hypertensive workers was 52 years, with a mode at 53, a minimum age of 37, a maximum age of 60, and a standard deviation of 5.1 years. The population was made up of 73% of older workers. The graph of HBP's age and general population's age have almost the same trend. The population includes 57% of workers over 45 years old. Older hypertensive workers were by far more dominant (14%) than younger hypertensive workers (1%). The Chi2 test gives p-value = 0.0000 with OR = 16.95. We found the installation of hypertension after 45 years old in 65% of cases. The average age of onset of hypertension was 44.9 years.
Almost half of the study population was obese (46%). There is more obese in the active workers (38%) than in the sedentary population (8%). Obese had the highest percentage of hypertension. Sedentary patients with normal BMI do not have hypertension (p=0.0000 with OR=4.7). The seniority curve in the factory and the one in the service mix. Almost all workers (90%) had not changed service since hiring.
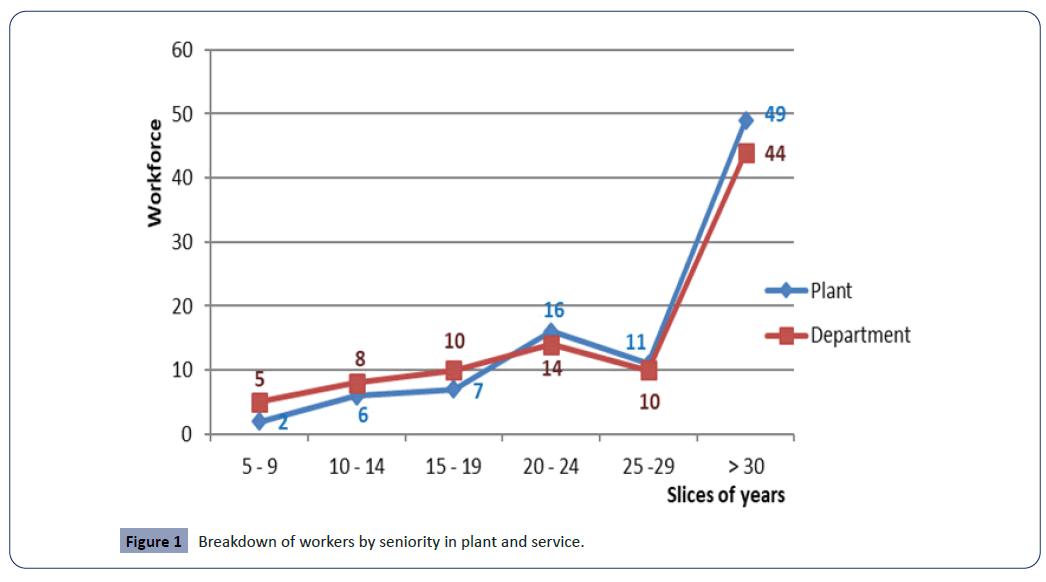
The population in 54% of cases had more than 30 years of seniority, with an average of 27 years (Figure 1).
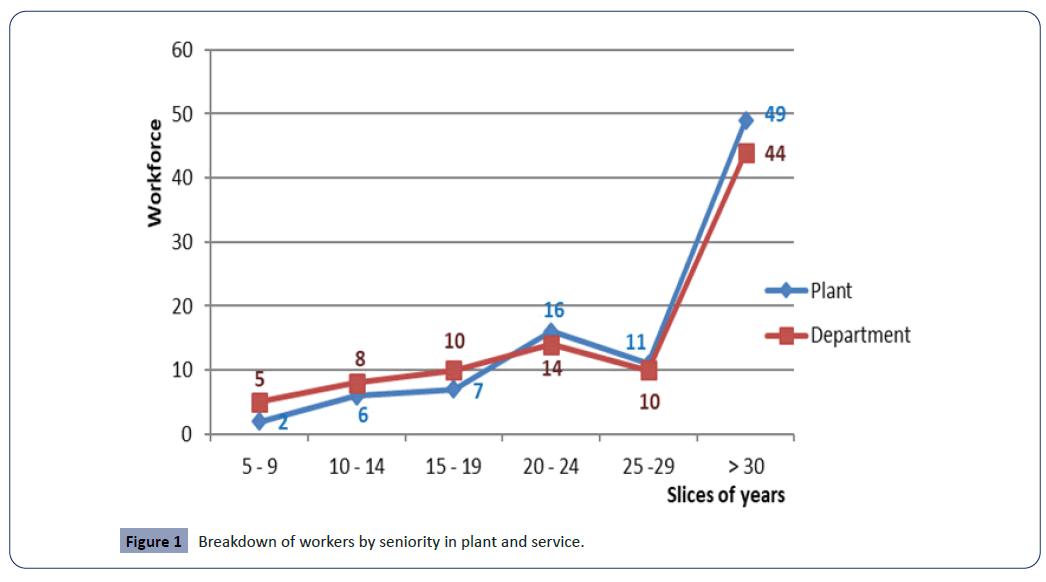
Figure 1: Breakdown of workers by seniority in plant and service.
Hypertensive workers had a family history of HBP in 38% of cases. In addition, they had diabetes in 17% of cases. The dyslipidaemias were present in 2% of the cases of comorbidities. Workers took cigarettes in 4% of cases, and occasionally consumed alcohol in 56%.
Workers in the active sectors accounted for 91% of the hypertensives (p=0.0000 with OR=7.16). There were more workers posted sick (8%), with a counterclockwise work pace (p=0.0168 with OR=1.72). Operators accounted for the largest percentage (66%) of hypertensive workers.
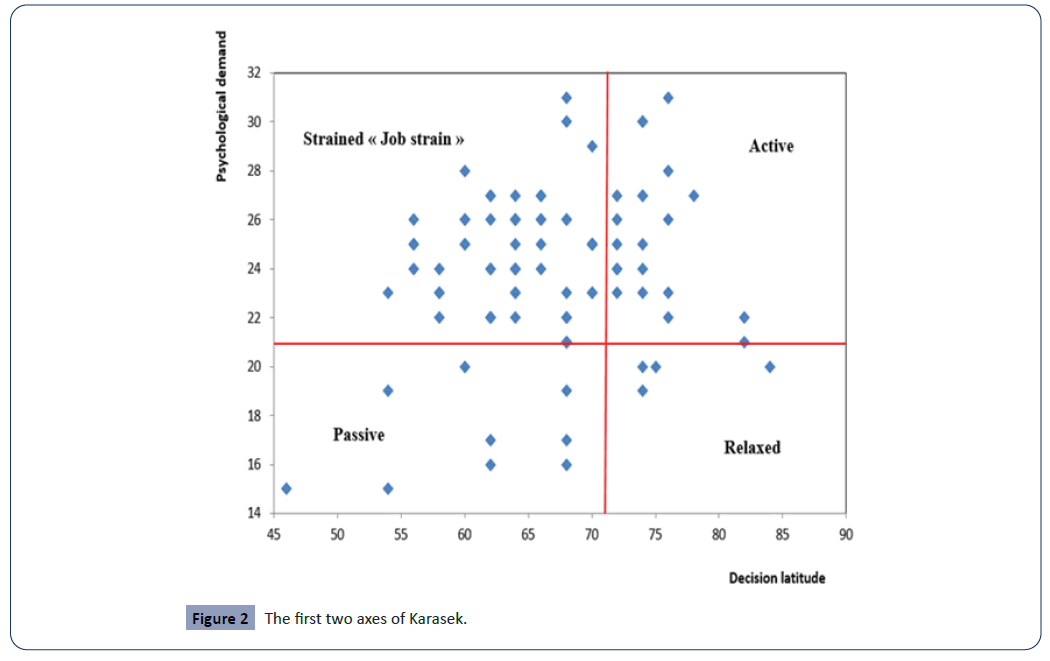
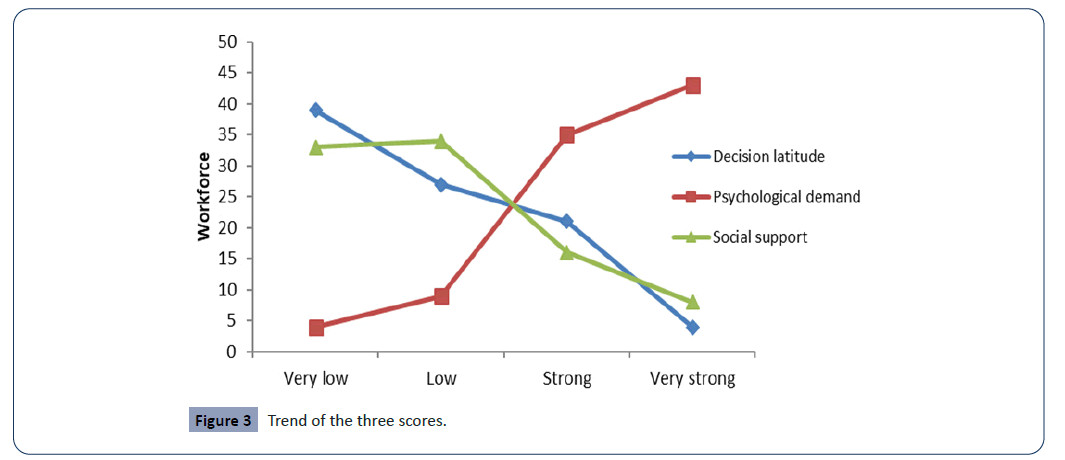
The workers in 63% of cases were found in the dial strained or called "job strain", among which 70% of operators. The cloud is much denser in the strained dial, representing workers who have high psychological demands and low decision latitude. 70% of the "Strained" dial consists of the operators (Figure 2). Social support and decision latitude decrease as psychological demands increase (Figure 3).
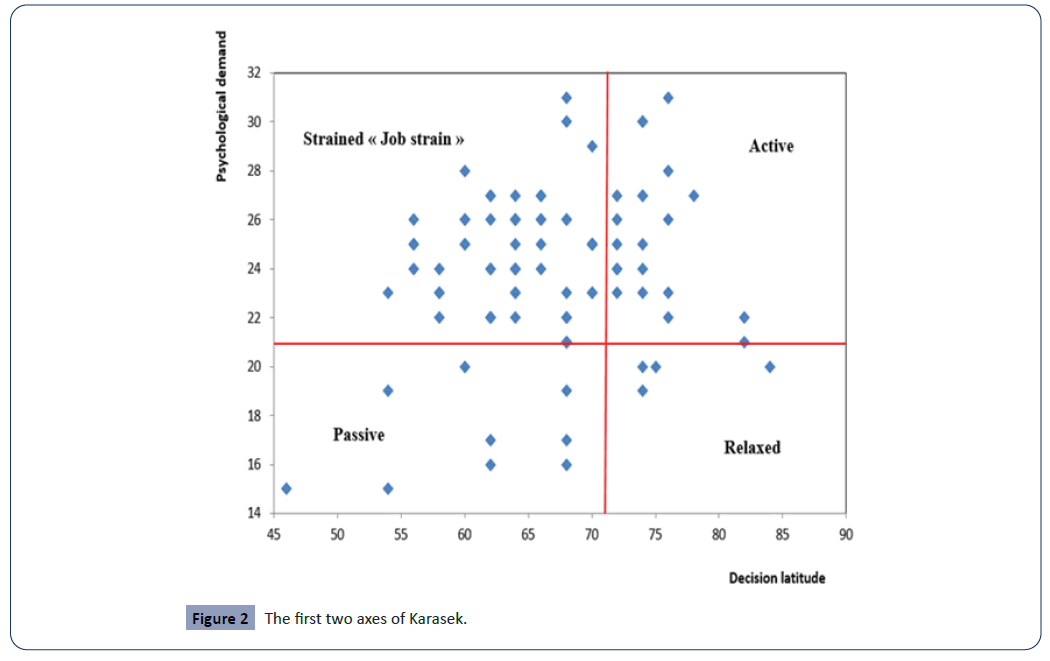
Figure 2: The first two axes of Karasek.
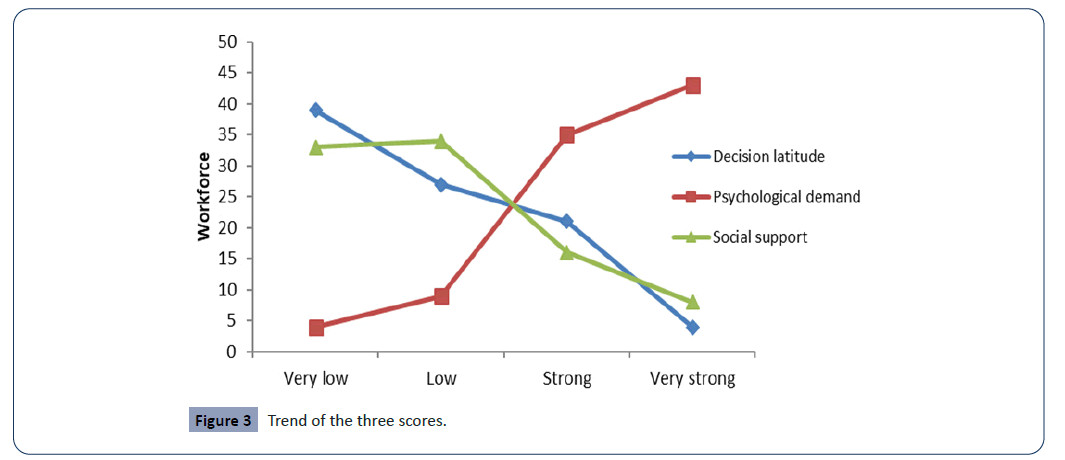
Figure 3: Trend of the three scores.
Discussion
The prevalence of HBP in the ALUCAM group is 14.3%. It is lower than the national companies’ prevalence which is 24.8%. This gap, for the least important, is most certainly justified by the fact that we have not considered the temporary staffs during this study which have approximately the same workforce than ALUCAM group permanent staff.
The hypertensive workers of the ALUCAM group were mostly married (97%). Nevertheless, during various interviews, many workers admit to very often experiencing strong marital strain, which affect them considerably. Marriage is therefore not necessarily a protective factor. Our hypertensive workers were exclusively men [13-20]. There are very few women in the factory, the physically less demanding tasks always devolving on them. This male population is aging, and therefore more vulnerable. There are 73% of workers over 50 years old. The average age was 52, for a 53-year-old mode. The youngest worker was 37 years old and the oldest worker was 60 (age limit for retirement) [21-25]. It is therefore a homogeneous study population. The year of installation of the HBP is just as great because, 65% of these workers had developed a HBP more than 45 years. The age of the hypertensive population and that of the general population follow the same curves [26-31]. The original population is aging, it is quite normal to have the same shot in the hypertensive population. The calculated p-value gives us p=0.0000 for a OR=16.6. Age is therefore a specific risk factor for the development of hypertension in this population [32].
The seniority, both in the company and in the department, is closed; the two graphs are practically superimposable. The worker, for many years perform the same tasks in the same environment and under the same conditions. This situation gives rise to certain monotony in carrying out the work, with the consequences that this could imply for both health and safety. As a result, 90% of hypertensive workers had never change the current role since hiring.
The average seniority of this group was 27 years old. 54% of this population had more than 30. The others (10%) changed jobs after spending an average of 11 years in the same department. It is known that the monotony is a situation likely to lead to a context of malaise at work.
The first observation reveals that HBP occurs in this population of "older" workers, at the average age of 45, as described in the literature [1]. However, to this is added the fact that its installation follows a period of business activity relatively long, with average seniority at 27 years and peaks at 40 years. These workers, regularly followed in occupational health center, the year of discovery of HBP corresponds to its year of installation. Almost half (42%) of our general population worked in the post. Among the hypertensive population, there were more shift workers (54%). The peculiarity of these posts is that they are all counterclockwise, this is to say that they do not follow the rhythm of the sun. This gap can have a real impact on the recovery of workers, as 11% of them complained of insomnia. Sleep having a clear importance on the metabolism of lipids and carbohydrates, unregulated, it causes a bad mobilization of the latter. To this is added the uncontrolled feeding of workers, and especially meals at odd hours after work (23h - midnight) constituting a health risk.
The lack of a canteen makes it very difficult to manage their food in the workplace. All this being likely to lead to excessive weight gain. Thus, there is a significant link between shift work and the presence of high blood pressure, as p=0.0168, with a binding force of OR=1.72. Shift work is therefore a risk factor for high blood pressure.
One third (33%) of the obese group was hypertensive. Obesity affects almost half of the hypertensive population (46%). By calculating the fraction of obese hypertensives among the entire obese population of the ALUCAM group, to make the percentages comparable, we obtain 27% of hypertensive obese exercising a so-called "active" job, and 5% of sedentary population. Obese hypertensives were therefore more numerous in the active than in the sedentary ones. The prevalence of obesity among active hypertensives (27%) was higher than that of the general population (29%).
The sedentary, mostly managers and executives are the most educated. They therefore have the advantage of having more information and provisions for understanding the risk factors of hypertension. They thus take the consequent recommended measures. In addition, they have provided them with fast and up-to-date information tools (Internet, books, seminars, etc.). Observation shows that all the group's managers have a rather normal BMI. In addition, we also find that no sedentary worker with normal BMI had HBP. The Chi-square test shows a significant link between HBP and obesity (p=0.0000) with OR=4.7, denoting the strength of this link. Thus, obesity is a risk factor for the occurrence of hypertension for this group of individuals.
We also found that 38% of hypertensives workers had a family history of hypertension and 17% of diabetes. These hypertensive workers with diabetes in addition are 16 people. However, the prevalence of diabetes in the general population of the ALUCAM group is 3%, which corresponds to 19 people. 85% of diabetics in the ALUCAM group are also hypertensive. The statistical test performed confirms a significant link with hypertension and diabetes’ history (p=0.0000; OR=39.96). Diabetes is therefore a very important risk factor in this population for the development of hypertension.
Hypertensive workers in 4% of cases took cigarettes, and 89% did not take alcohol or rarely. The sports activity was not very developed in our subjects because only 21% of them practiced sport regularly. This observation can certainly be justified by the constraining nature of the schedules of posted workers. Many workers say they are "washed out" at the end of the day, and they are also convinced that their work is a significant sport.
The diet of 33% of these hypertensive workers was characterized by the very regular consumption of meat. But the consumption of meat is riskier than that of fish or vegetables. These foods often contain fats and cholesterol that can lead to weight gain and increased LDL cholesterol. The low level of education, in addition to shift work, can also justify bad practices (food, sports, addictive) that they develop. Indeed, up to 15% of these workers, exclusively made up of operators, have a basic level of education, often not enough to understand the subtlety of certain risks.
The distribution of hypertensive workers shows a predominance in the operational sectors where physical activity is intense. So, 89% of these came from factory departments, where physical demand is high. These sectors had the particularity of accumulating physical nuisances such as noise and heat, recognized for their impact on health and particularly on HBP. The average noise level in each of these sectors being greater than 85 dB (A), with peaks up to 130dB (A), requiring effective noise protection. All this has repercussions on the mental health of the workers [32,33] who in addition were aware of being in an environment which presented dangers (noise, machine, chemical) and risks (cut, crush, hearing loss) permanent for their health and safety.
Made up of 66% of operators, our hypertensive population was mostly operators. Assigned to "messy" tasks. The psychosocial risk assessment according to the Karasek model shows that 86% of workers experience a high psychological demand, and only 27% have significant decision latitude. Social support decreases with increasing solicitations. This is a rather crude representation of the psychosocial level which does not indicate much yet.
The torchbearer of Robert Karasek's methodology in the risk assessment process shows that the cloud of hypertensive workers is located more in the "Strained" dial, also called "Job strain". This population represents 63% of hypertensive workers. It is inside this dial that the risk of having repercussions on health is much high. It is easy to see that social support and decision latitude decrease while psychological demand increases (Figure 3). Demand is so strong in the population, but the support of hierarchy and colleagues is weak. However, workers with high psychological demands and low decision-making latitude would see the impact on health decrease if they enjoyed good social support [25,26].
Operators make up 70% of workers in "strained" work situations. The Sumer 2003 survey [15] corroborates this by classifying operators as the most exposed to "Job strain".
The stress at work, defined as the strained nature of the work perceived by the worker, constitute risk factors for health, and the increase of blood pressure in particular, as has been advanced, although not objectified, by a study carried out at the Autonomous Port of Abidjan [27]. To this will be also added the job occupied and the role of the operator.
HBP thus has rather diversified origins which, most of the time, develop as a result of the accumulation of several risk factors. Lifestyle, eating habits, sedentary lifestyle and suffering at work are the most frequently mentioned causes, some of which have been identified in this study. The Chi-square test gives us a p=0.000, which shows a significant link between the "active" work and the installation of the HBP. OR=7.16, confirms the strength of this link. The workstations of these hypertensive workers contain nuisances whose impact (extra auditory) on health in general, and HBP in particular, is known [16]. In fact, it is actually the "nuisance at work" component, consisting mainly of noise and heat, which takes precedence over the physical activity itself in terms of risk, the nuisances at the workplace inducing a stress with physiological manifestations, therefore in favour to the HBP installation.
The study conducted by Taleb et al [28], shows that the risk of HBP associated with the age of exposure to noise over 20 years is significantly multiplied by 2.4 (p=0.03). That associated with a psychological work environment combining high psychological demands and low decision latitude is significant and is a key risk factor for hypertension. These results support the hypothesis of the hypertensive role of exposure to undesirable psychosocial factors at work or chronic exposure to noise and indicate a group at risk for HBP in the workplace [29-31]. These results corroborate our data.
Conclusion
The mental health of workers is dependent on management. The psychosocial work environment is now recognized as a determinant of health, especially cardiovascular health. We therefore consider risk factors of genetic (age, family antecedents), somatic (obesity) and especially psycho-social (stress and suffering at work).
Regarding the age and family history of the worker, the results we obtained are confirmed by data from the international and national literature that usually associate hypertension with older subjects, and therefore with seniority. The link between age and hypertension was clearly established (p=0.000 OR=16.6). In this population, workers over 45 are therefore more likely to develop an HBP. With a family history such as diabetes (p=0.000 OR=39.96), the risk of developing hypertension increases.
Shift work induces poor regulation of sleep, leading to poor mobilization of lipids and carbohydrates, among other things. These atypical work schedules are also known to give the worker a lower quality diet, especially when the company does not have a canteen to regulate the flow and quality of food. The consequence is the uncontrolled weight gain (obesity) which is the first risk factor for the development of diabetes, which itself is in this population an important risk factor for the installation of hypertension (p=0, 0168, OR=1.72). Beyond the somatic consequences (obesity) shift work also generates stress in the worker related to the constraint of schedules and the pressure induced by shift work itself.
The expansion of occupational health and safety in the group has enabled the establishment of control methods that protect the worker from the physical dangers that surround him, through effective collective and individual measures. Today, workers are well equipped (training, habitation, STOP 5, PPE) to face the physical risks they encounter. Thus, it is not so much the activity as "work done" requiring a specific technique that is a risk factor in itself, but rather the psychological environment and the social context in which the latter is carried out. As a result, if the workers carrying out these activities enjoyed a good margin of decision latitude and strong social support from the hierarchy and colleagues, the impact on health would be considerably lessened. The Karasek dispersion graph confirms this because, according to the Sumer 2003 survey, "strained" workers are more worried about the risk of sanctions in the event of an error, which makes them more stressful and worsens the feeling of uneasiness, thus increasing the cardiovascular risk. In addition, employees in a situation of "Job strain" have an even more negative judgment on their health when say they lack support. Thus, we have seen in Figure 3, the steady decline in social support and decision latitude while the psychological demand for it is constantly increasing. This situation gives the worker a real feeling of suffering at work, unproductive, in the face of the negative impact it has on the health and safety of workers and the company.
We consider two fundamental risk factors: obesity and stress/ suffering at work. Thus, our results show that among hypertensive workers, 46% are obese, compared with 63% who are stressed or suffer at work. Psychosocial risk is therefore the most important risk factor for the development of hypertension.
Ultimately, the activity has a significant impact on the occurrence of hypertension, through its psychosocial components unfavourable for the worker in general, and particularly to the operator.
The results of this study can be extended to other companies with the same work’s conditions and the same social habits. However, much more refined later analyses, considering quantifiable risk factors with a very high relevance in the physio pathological analysis of the installation of the HBP, constituting the limits of our study, would make it possible to further refine this work. And make it more complete. There are:
• Systematic dosages of lipids in all workers,
• Assessment of the psychosocial level of all workers,
• Include temporally staff on the study.
29793
References
- WHO (2011) Global status report on noncommunicable diseases 2010. Geneva.
- College of Teachers of Cardiology and Vascular Diseases (2013) Hypertensionadult blood pressure. Francophone Virtual Medical University.
- Campbell NRC, Lemogoum D (2009) Hypertension in sub-Saharan Africa: a massive and increasing health disaster awaiting solution. Cardiovasc J Afr 26: 152–154.
- Monkam-Mbouende Y (2011) High blood pressure and prevention. Cameroonian Society of Cardiology.
- Stellman JM (2000) Encyclopedia of occupational health and safety. International Labour Organization.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. (2003) The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA 289: 2560-2572.
- University College of Nephrology Teachers (2010) Epidemiology of hypertension in adults.
- Mélihan-Cheinin P, Larochette N, Martin D, Basset B, Postel-Vinay N, et al. (2004) The fight against smoking. Efficacy of measures against societal factors. Rev Prat 17: 1865-1882.
- Fournier PS, Montreuil S, Brun JP, Bilodeau C, Villa J (2010) Scoping Study of Workload Factors Impacting Health and Safety: A Case Study in the Service Sector. IRSST publications
- Guy B, Patrick C (2003) Foreword (Stress and post-traumatic mental disorders). The practitioner's review 8: 825-866.
- Guignon N, Niedhammer I, Sandret N (2003) Psychosocial factors at work An evaluation using the Karasek questionnaire in the SUMER 2003 survey. Documents for the occupational physician TF 175.
- Fricot R (2010) Psycho-social factors, a danger for the company. AFOMETRA.
- Jacob S, Hery M, Stengel B (2008) Exposure to organic solvents. Risk of progression of chronic kidney disease to end stage renal disease. Studies and surveys TF 170.
- (2008) Exposure to organic solvents, Document for the Occupational Physician.
- Kidney Disease Outcomes Quality Initiative (2004) K/DOQI Clinical Practice Guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis 43: S1–290.
- Burnier M, Menno Pruijma T, Battegayb E (2009) Renal failure. Forum Med Suisse 9: 497.
- Schoolwerth AC, Sica DA, Ballerman BJ, Wilcox CS (2001) Renal considerations in angiotensin converting enzyme inhibitor therapy: a statement for healthcare professionals from the council on the kidney in cardiovascular disease and the council for high blood pressure research of the American Heart Association. Circulation 104: 1985-1991.
- Presne C, Monge M, Mansour J, Oprisiu R, Choukroun G, et al. (2007) Diuretic- based therapy. Nephrology Ther 3: 392-426.
- Beaudeau P, Besancenot JP, Caserio-Schönemann C (2003) Cold and health, INVS, investigation report.
- DARES (2008) Psycho-social risks: The model of Karasek Sumer 2003 First synthesis.
- Karasek R, Theorell T (1990) Healthy Work: Stress, Productivity and the Reconstruction of Working Life. New-York: Basic Books.
- Koffi NM, Sally SJ, Kouame P, Silue K, Nama AJD (2001) Facies De L’hypertension Arterielle En Milieu Professionnel A Abidjan. Black African Medicine 48: 257-260.
- Taleb A, Brahim BM, Benrezkallah L, Benkalfat FZM (2003) Exposure to noise, psychosocial environment and high blood pressure in the workplace. Archives of Occupational and Environmental Diseases 64: 246-252.
- BelkiÃÂÃÂââ¬Ã
¾ÃÂâÂÂâ⇠K, Landsbergis P, Schnall P, Baker D, Theorell T, et al. (2000) The Workplace and Cardiovascular Disease (Occupational Medicine: State of the Art Reviews). Philadelphia: Hanley & Belfus Inc.
- Marmot MG, Bosma H, Hemingway H, Brunner E, Stansfeld S(1997) Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet 350: 235-239.
- Brisson C, Larocque B (2001) Validity of occupational stress and decision latitude on health in the National Population Health Survey of 1994-95. Canadian Journal of Public Health 92: 468-474.
- Fouda AAB, Lemogoum D, Manga JO, Dissongo JII, Tobbit R, et al. (2012) Epidemiology of obesity in the work milieu, Douala, Cameroon (free access). Rev Med Brux 33: 131-137.
- Dawber TR, Kannel WB (1996) The Framingham study. An epidemiological approach to coronary heart disease. Circulation 34: 553-555.