Gustav Y Cederquist1 and James J Harding1,2*
1Department of Medicine, Memorial Sloan Kettering Cancer Center, 300 East 66th Street, NY, NY 10065, USA
2Department of Medicine, Weill Cornell Medical College, 1300 York Avenue, NY, NY, 10065, USA
Corresponding Author:
James J Harding
Department of Medicine
Memorial Sloan Kettering Cancer Center
300 East 66th Street, NY, NY 10065, USA
Tel: 646-888-4314
E-mail: Hardinj1@mskcc.org
Received date: July 08, 2016; Accepted date: July 11, 2016; Published date: July 14, 2016
Citation: Cederquist GY, Harding JJ. Horner’s Syndrome and Syncope. Arch Can Res. 2016, 4:3.
A 70-year-old female complained left eyelid drooping and three syncopal episodes over one week. Six years prior, she was diagnosed with Merkel cell carcinoma of the right nasal vestibule and underwent combined modality therapy.
Case Blog
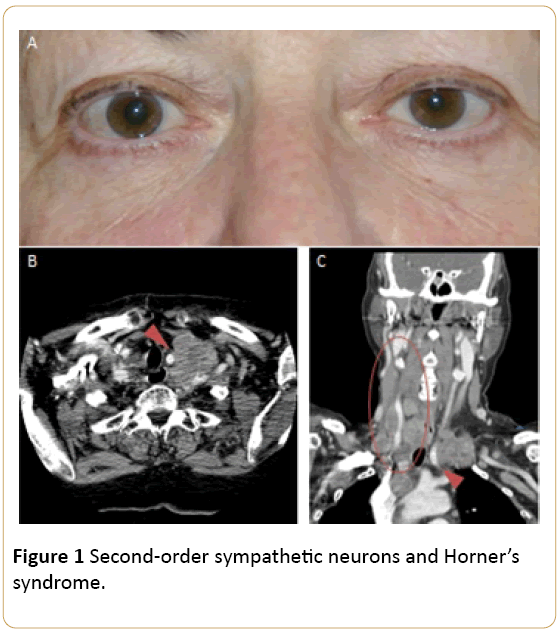
A 70-year-old female complained left eyelid drooping and three syncopal episodes over one week. Six years prior, she was diagnosed with Merkel cell carcinoma of the right nasal vestibule and underwent combined modality therapy. Physical examination revealed left-sided ptosis and myosis (Figure 1A). Computed tomographic imaging revealed supraclavicular and thoracic inlet adenopathy. A lymph node encased the left common carotid artery (Figure 1B and Figure 1C leading to compression of second-order sympathetic neurons and Horner’s Syndrome. Right-sided cervical adenopathy along the carotid artery stimulated the carotid baroreflex leading to recurrent syncope (Figure 1C, red circle). Horner’s syndrome is the triad of miosis, ptosis, and anhidrosis. The latter occurs in 50% of cases, is subtle, and depends on level sympathic disruption. Horner’s syndrome should prompt an evaluation for lesions along the sympathic tract, including stroke, malignancy, and carotid artery dissection. The patient received etoposide and carboplatin with transient symptom improvement.
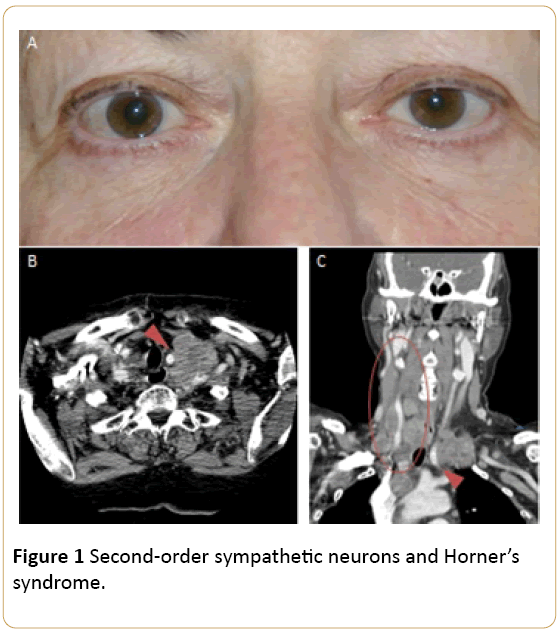
Figure 1: Second-order sympathetic neurons and Horner’s syndrome.
9912