Keywords
Home care; Non-skilled home care; Hospitalization rate; Care management; Standardized home care assessment
Introduction
Nearly ninety percent of people 65 years or older have at least one chronic condition, and a quarter have four or more chronic conditions [1]. As the number of older beneficiaries with multiple chronic conditions continues to rise, providing care in the most efficient setting is essential. When asked about their care preferences, older Americans over whelmingly articulate a desire to age in place and receive care at home rather than in institutional settings [2]. Many aging individuals develop a need for assistance with one or more activities of daily living, and experience falls at high rates, which together is associated with a higher risk of hospitalization [3]. In order to match the personcentered goal of living safely at home for as long as possible with an appropriate degree of support, non-skilled home care caregivers are frequently needed to support limitations on activities of daily living [4]. As such, the demand for non-skilled home care services continues to increase. Recognizing this, the Centers for Medicare and Medicaid Services recently made nonskilled home care an available supplemental offering in Medicare Advantage plans [5].
As a goal of home care is to enable people to age in place at home, care management programs (programs that provide intermittent risk assessment, access to nurses and health care providers - without necessary simultaneous use of the skilled home health care benefit), may be an enabler of success of nonskilled home care programs. Home-based care management has been shown to reduce hospitalizations, rehospitalizations and skilled nursing facility placements and improve patient and caregiver satisfaction [6,7]. In addition, studies have shown that chronically ill Medicare beneficiaries can benefit from nurse-led care management models [8,9].
Despite increasing momentum for both skilled and non-skilled home care as value-add services for high-risk populations, the hospitalization rate among recipients of non-skilled home care has not been previously characterized. In fact, a recent literature search (PubMed) returned no articles reporting hospitalization rate for non-skilled home care recipients. In this study, we aimed to determine the hospitalization rate for multi-morbid recipients of non-skilled home care, and to assess the feasibility of using a nurse-led standardized assessment, outside the skilled home health care benefit, as an intervention to influence hospitalization rates in this population.
Methods
To track hospitalizations, we used a combination of data sources, including the electronic health record and direct communications with patients and practitioners. To track the number of days a person was receiving home care, as well as any hospitalizations that occurred, a census tracking database was used (HCS Interactant®, Wall Township, NJ). We performed a retrospective review of this census tracking and length-of-stay database. Hospitalization rate per 1,000 managed patients per year was calculated as (Admissions/(Managed Months/1,000)) x 12) [10].
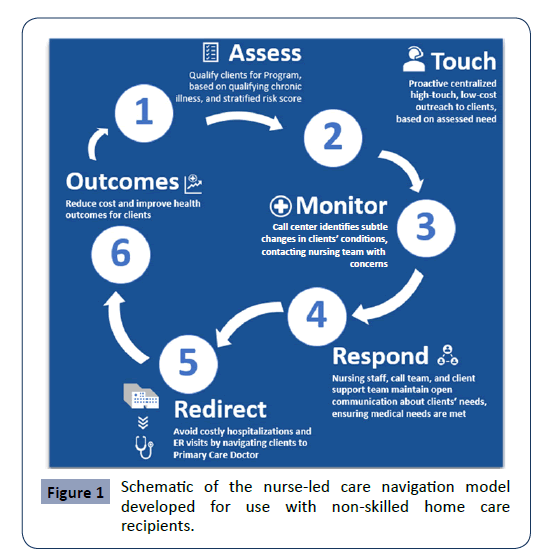
In order to support the development of a standardized assessment tool for non-skilled home care recipients, we performed a review of care management studies, guidelines and protocols to support an evidence-based approach. We selected candidate assessments for integration into the program if the results of a given assessment could trigger activation of a resource that could support a patient in a way that could better align goals of care, increase quality, or lower avoidable acute care utilization. These assessments were built into a care management risk assessment tool we named PREDICS (Figure 1). Care managers performing the assessments were licensed nurses. An initial inhome assessment by a registered nurse was performed on all study patients. During the initial assessment, all study patients received the contact number for the 24/7 nurse contact center. A nurse reviewed the patient’s status and health risks monthly after the initial assessment. A personal care score and homemaking score was determined for each home care recipient. When a significant health risk was identified, the nurse communicated with the patient’s primary care physician. Such risks included new or worsening shortness of breath, new or worsening cough, altered mental status, new or worsening lower extremity edema, intractable pain, wounds, inability to check blood sugar, and medication non-adherence.
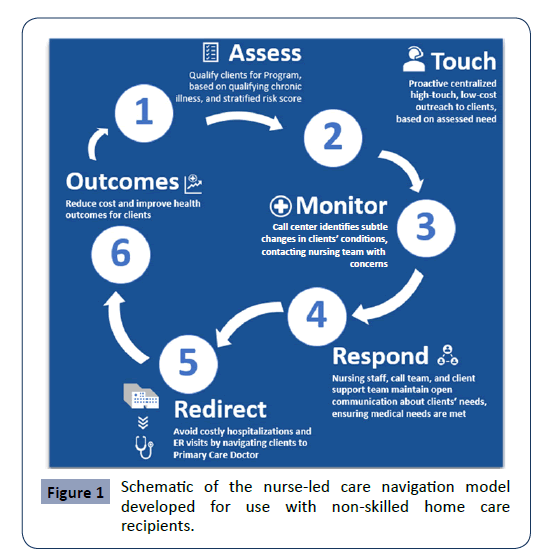
Figure 1: Schematic of the nurse-led care navigation model developed for use with non-skilled home care recipients.
We compared hospitalization rates among recipients of standard non-skilled home care (Control group) to the hospitalization rates for patients receiving care via a risk-stratified nurse care management program (Study group). Inclusion criteria for both control and study groups were identical: 65 years or older, a primary or secondary diagnosis of congestive heart failure, chronic obstructive pulmonary disease, pulmonary hypertension, diabetes, or a wound. Three non-skilled home care branches of similar size (based on persons served) were placed into the study group, and three home care branches of similar census size were placed into the control group. We used Interactant data to calculate the overall hospitalization rate, as well as the rate that each group experienced.
Data Analysis
Data from the study group was available for a four-month period between March 2019 and June 2019. This data was matched with the corresponding four-month home care data from the control branches. Non-skilled home care services were provided for a total of 6,058 total patient months (2,888 in the control group and 3,170 in the study group). In the control group, 129 hospital admissions occurred during this period (536 admissions per 1,000 managed patients per year). In the study group, 134 hospital admissions occurred (507 admissions per 1,000 managed patients per year) (Table 1).
Table 1 Characteristics of Home Care Recipients Served Between March 1, 2019 and June 30, 2019.
| |
Total |
Home Care |
Care Management Plus Home Care |
| Managed Months |
6,058 |
2,888 |
3,170 |
Age
Mean (SD); Min-Max |
72.3 |
72.9 |
71.7 |
| Female n (%) |
907 (60%) |
428 |
479 |
| Hospitalizations |
263 |
129 |
134 |
Hospitalization Rate
Hospitalizations per1,000
Patients Per Year
1,000 Patients Per Year |
529 |
542 |
516 |
| |
|
|
| |
Our statistical approach to data analysis was two-pronged. First, we used mixed linear modeling to compare differences in hospitalization rates between the study and control sites (fixed effect) while accounting for clustering of patients within branches (random effect). We also used some of the risk assessment data from the patients receiving nurse-led care management such as home-making scores and personal care scores to predict instances of hospitalization in this group using logistic regression. To ensure independence of observations, each record in this subanalysis belonged to a unique individual. If the same person was hospitalized more than once, only the most recent hospitalization and assessment record was retained.
Results
Mixed Linear Modeling
Grouping of patients by branch accounted for 4.9% of variability in hospitalization rate per 1,000 managed patients per year. This intraclass correlation coefficient (ICC) was not statistically significant (p=0.88) due to a large standard error of estimate (SE=17,327.83). The random effect of the interaction of home care branch by treatment condition accounted for additional 25% of variability in hospitalization rates (Table 2). However, the study condition itself failed to explain a significant amount of residual variance (69.8%) in hospitalization rate after controlling for the random effect of branch and branch-by-condition interaction (F1,4=0.04, p=0.85). Nonetheless, patients in the study group had lower mean rate of hospitalization (507 hospitalizations per 1,000 managed patients per year) compared to the control group (536 hospitalizations per 1,000 managed patients per year).This effect, however, was not statistically significant, possibly due to the four-month study period being too short to reach significance.
Table 2 Estimates of Covariance parameters for a Mixed Linear Modeling analysis of hospitalization rates as a function of condition (study vs. control) while controlling for the random effect of home care branch.
| Parameter |
Estimate |
Std. Error |
Wald Z |
p |
(95% CI)
Lower bound Upper Bound |
| Residual |
35,363.19 |
11,787.73 |
3.00 |
0.003 |
18,399.99 |
67,965.00 |
| Branch |
2,491.17 |
17,327.83 |
0.14 |
0.89 |
0.003 |
2.08E+9 |
| Condition x Branch |
12,795.50 |
0.00 |
- |
- |
- |
- |
ICC for Branch=0.049; ICC for Branch x Condition=0.25
Logistic regression
Within the study group, we first eliminated records of patients with multiple assessments and hospitalizations retaining only the most recent records. We also excluded patients with records of hospitalization at the target branches without corresponding assessment data. Our final sample comprised 304 unique patient records, only 24 of whom were hospitalized (7.8%). In binary logistic regression, when one category of the dependent variable is a rare occurrence compared to the other category, the Type II error increases as it makes it much harder to detect a significantly better proportional by-chance accuracy rate in the model with all of the predictors in the equation compared to the null model [11]. This, in turn, results in a very poor performance of the maximum likelihood estimation procedure used in logistic regression producing biased and inaccurate parameter estimates [12].
In the current study we split the sample of non-hospitalized study patients (n=283) into two halves of 142 and 141 individuals, respectively. We randomly sampled 24 patients from the first half, combined them with the sample of 24 hospitalized patients and developed a logistic regression model on this training sample. If the model produced a good data fit and explained a significant amount of variance in the criterion (hospitalization), we intended to validate the model by saving its estimated parameters and applying them to the testing sample, which contained 24 patients randomly sampled from the second half of the non-hospitalized patient pool. Application of the training model’s parameters to the new sample would produce estimated posterior probabilities of group membership in the testing sample. These probabilities can then be used to classify participants into groups and access the shrinkage of the testing model compared to the training model [13].
Our logistic regression analysis on the training sample with homemaking and personal care risk scores entered as predictors did not reveal any significant improvement of the null model in prediction of instances of hospitalization, increasing the proportionate by-chance accuracy of classification by only 3.3% from 50% to only 53.3%, which is not statistically significant (χ2=3.43, p=0.84). The model accounted for only 0.5% of variability in hospitalizations (Nagelkerke R2=0.005). Parameters on individual predictors are summarized in Table 3.
Table 3 Logistic regression analysis summary for the final model predicting hospitalization among Study patients between March 1st and June 1st, 2019 (n=48) Nagelkerke R2=0.005.
| Prediction Accuracy (%) |
Predictor |
B |
Wald |
Sig |
Exp (B) |
| Sensitivity |
69.6% |
Home Making Score |
-0.04 |
0.01 |
0.93 |
0.99 |
| Specificity |
36.4% |
Personal Care Score |
-0.01 |
0.16 |
0.69 |
0.99 |
| Overall |
53.3% |
|
|
|
|
|
Discussion
There is limited hospitalization rate data currently available for non-skilled home care recipients. In fact, a recent literature search (PubMed) returned no articles reports on hospitalization rate for non-skilled home care recipients. In this report, we provide a means for calculating hospitalization rate using a home care census tracking database, and we describe a method of providing value-add, nurse-led care management as a resource for home care recipients. Tracking hospitalizations and calculating hospitalization rate is an important step toward building home-centered care programs, in order to help reduce unnecessary hospitalizations for home care recipients. With home care increasingly being recognized by physicians and payors as a valuable service for complex patients, laying the groundwork to track and report important outcome measures such as hospitalization rate can be an enabler of further valuebased care initiatives.
In this study, home care recipients were hospitalized at an overall rate of 520 hospitalizations per 1,000 per year.This rate is comparable to that reported by community-dwelling Medicare beneficiaries enrolled in the Program of All-Inclusive Care for the Elderly (PACE).In this study, Segelman reported a hospitalization rate of 539 hospitalizations per 1,000 per year for dually eligible PACE enrollees [14]. The rate we report is higher than the 2000- 2006 Medicare average hospitalization rate for those 75-84 years of age (392 hospitalizations per 1,000 per year), which is to be expected, since our cohort had a serious medical diagnosis, in addition to requiring non-skilled home care for caregiving assistance.
This report shows that implementation of a nurse-led care management program that uses a standardized assessment tool is feasible for recipients of non-skilled home care. The PREDICS tool was built to enable an evidence-based workflow for nurse care managers with an aim of selecting assessments that could provide actionable, discrete, risk stratified data output. Using the PREDICS risk of hospitalization assessment tool, we were able to risk stratify home care recipients and leverage nurses to help address risks. Once a risk was identified, the nursing team notified the patient’s physician or his/her designee so an appropriate action could be taken. This model may be more effective when coupled with a more directly aligned home care physician or nurse practitioner, and this requires further study. Future studies are needed to determine whether other activities, such as active home-based medication management, may also positively affect hospitalization rate.
Conclusions and Implications
In conclusion, measuring hospitalization rate in recipients of nonskilled home care is possible, and we found home care recipients with a serious medical diagnosis had an average hospitalization rate of 520 hospitalizations per 1,000 managed patients per year. Further, this study demonstrates that applying a nurse-led care management model to provide additional support to non-skilled home care recipients with a chronic medical diagnosis is feasible. Whether or not the model can influence hospitalization rate in non-skilled home care recipients requires additional study.
33499
References
- Bodenheimer T, Wagner EH, Grumbach K (2002) Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA 288:1909-1914.
- Keenan TA (2010) Home and community preferences of the 45+ population. AARP.
- Landers S, Madigan E, Leff B, RosatiRJ, McCann BA, et al. (2016) The Future of Home Health Care: A Strategic Framework for Optimizing Value. Home Health Care Manag Pract 28:262-278.
- (2018)2019 Medicare Advantage and Part D Rate Announcement and Call Letter.Centers for Medicare & Medicaid Services.
- Wajnberg A, Wang KH, Aniff M, Kunins HV (2010) Hospitalizations and skilled nursing facility admissions before and after the implementation of a home-based primary care program. J Am Geriatr Soc 58:1144-1147.
- Hughes SL, Weaver FM, Giobbie-Hurder A, Manheim L, Henderson W,et al. (2000) Effectiveness of team-managed home-based primary care: a randomized multicenter trial. JAMA 284:2877-2885.
- Shurrer J, O’Malley A, Wilson C, McCall N, Jain N (2017) Evaluation of the Diffusion and Impact of the Chronic Care Management (CCM) Services: Final Report. Mathematica Policy Research.
- Mills WR, Poltavski D, Douglas M, Owens L, KingA, et al. (2020) A Platform and Clinical Model to Enable Medicare's Chronic Care Management Program. Popul Health Manag 23:107-114.
- McCall N, Geonnotti K (2015) Utilization Measures Worksheet. Mathematica Policy Research 2015.
- Petrucci CJ (2009) A primer for social worker researchers on how to conduct a multinomial logistic regression. J Soc Serv Res 35: 193-203.
- King EN, Ryan TP (2002) A preliminary investigation of maximum likelihood logistic regression versus exact logistic regression. Am Stat 56: 163-170.
- Steyerberg EW, Harrell FE, Borsboom, GJ, Eijkemans, MJ, Vergouwe Y, et al. (2001) Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol 54: 774-781.
- Segelman M, Szydlowski J, Kinosian B, McNabney M, Raziano DB, et al. (2014) Hospitalizations in the Program of All-Inclusive Care for the Elderly. J Am GeriatSoc 62: 320-324.