Mini Review - (2022) Volume 13, Issue 2
Hypothermia as a Treatment Option for Intra and Post Ischemic Stroke
Manik Mathur* and
Bayraktutan U
Division of Clinical Neurosciences, GNRC Hospitals, Assam, India
*Correspondence:
Manik Mathur, Division of Clinical Neurosciences, GNRC Hospitals, Assam,
India,
Tel: +7297825248,
Email:
Received: 16-Jan-2022, Manuscript No. ipjnn-22-12394;
Editor assigned: 18-Jan-2022, Pre QC No. P-12394;
Reviewed: 22-Feb-2022, QC No. Q-12394;
Revised: 24-Feb-2022, Manuscript No. R-12394;
Published:
03-Mar-2022
Abstract
Neuro-inflammation is a key component in the ischaemic cascade following cerebral ischaemic insult that results into tissue damage, leakage in the bloodbrain barrier and death in the sub-acute phase. Failure of anti-inflammatory drugs to improve outcome in clinical settings have suggested its response following an ischeamic attack is detrimental. Hypothermia is a robust neuro protectant and has consistently shown benefit against a variety of brain injuries at the experimental level. It has recently been shown to improve neurological outcome in comatose survivors of cardiac arrest and neonatal hypoxic ischemia. Although until now, therapeutic hypothermia doesn’t categorise under any therapeutic standards of parameters, but it is well accepted that cooling should be started as soon as possible following an ischeamic attack. This review discusses the protective influence of hypothermia on the neuro-inflammatory response.
Keywords
Neuroinflammation; Cerebrovascular; Brain ischaemia; Hypothermia
Introduction
Cerebrovascular accidents usually conduit towards functional
disability in aprox 10%-15% of all admissions with long-term
outcomes [1]. Brain ischaemia, a product of numerous pathological
conditions, results into exhaustion of ATP, energy crisis and
failure of ion pumps resulting into depolarization of neuronal
cell membranes and outburst of glutamate resulting in oxidative
stress [2]. Moreover, altered calcium homeostasis, initiation of
cell death pathways (apoptosis, necrosis and autophagy) and
inflammation further instigates the Blood-brain-barrier (BBB)
disruption [3-6]. On clinical grounds, ischaemic patients when
presented already have attained irreversible brain injury and may
paradoxically antagonize the benefits of restoration of blood.
There is overwhelming experimental and clinical data to support
the use of Hypothermia (HT) in limiting ischaemic brain damage
[7]. Several animal studies have demonstrated that induction of
HT decreases final infarct volume and increases potency of brain
to withstand ischaemic attack before permanent damage occurs
[8-10].
Cooling of the body for therapeutic purposes is not a new
concept in medicine. First reported case regarding usage of HT in
traumatic brain injury (TBI) was in 1943 [11] whereas, its surgical
use was obtained in 1955 [12]. In 70s-80s the use of HT as a treatment was abounded due to the complications attached. It
was early 90s that is termed as “The return of Hypothermia” after
numerous animal studies showing its benefits even in its mild
form [8,13-15]. Recently, multicenter trail in Australia showed
survival rate of 49% in HT group v/s 26% in normothermia group
in comatose survivors of out-of-hospital cardiac arrest patients
with induced HT [16]. Another trail including 275 patients in
Austria was conducted in same year reflected that mild HT
improves neurological outcome after cardiac arrest in 55%
patients of HT group compared to 39% of normothermia. Also,
the six-month mortality rate was 41% in HT group to that of 55%
in normothermic group. Author concluded saying, patients who
have been successfully resuscitated following cardiac arrest, HT
increases the favorable rate neurological outcome and reduces
mortality [17]. By regulating intra-ischeamic brain temperature at
different levels, the histological setting was markedly influenced.
For example, hippocampal pyramidial neurons of the CA1 layer
showed grades 2-3 of damagein 100% of hemispheres held at
36°C during ischeamia but only 20% of those at 34°C [18]. Also,
ischeamic injury to dorsolateral striatum, was reduced by 80% at
33-34°C [8]. Induced moderate HT is therefore a logical approach
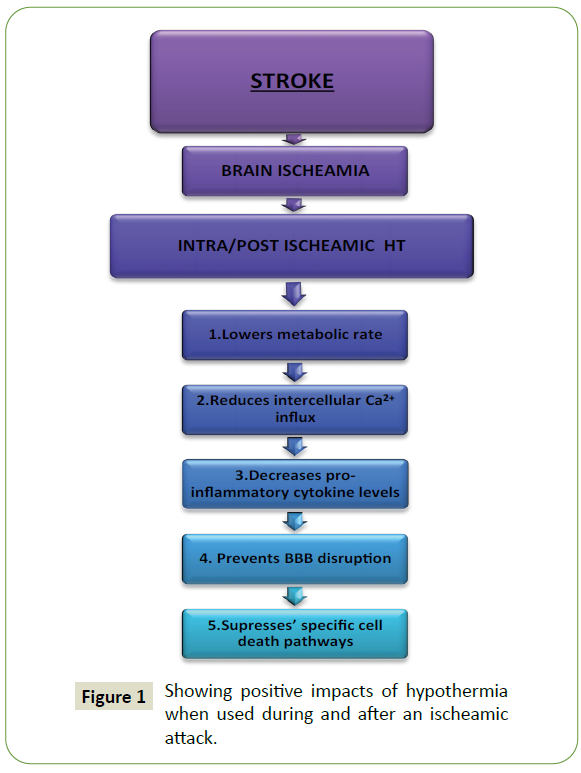
to limit damage from ischeamic attack (Figure 1).
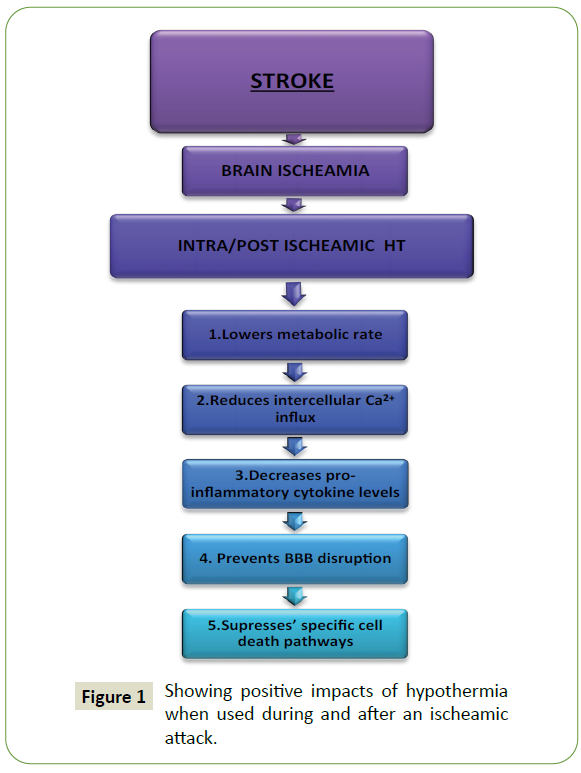
Figure 1: Showing positive impacts of hypothermia when used during and after an ischeamic attack.
There are numerous evidences that suggest therapeutic effects
of HT, by mechanisms including reduction of metabolic rate,
promotion of energy recovery after ischemia, inhibition of glutamate release, reserving cell death, decreased free radical
formation, reducing inflammation and thus preserving the BBB.
Naturally, a reduced metabolic rate might be expected to be one
of the most significant means by which HT could protect against
ischeamia. It has been calculated that, on the measure of reduced
metabolic oxygen consumption, 5 minutes of ischeamia at 37°C
would cause approximately equivalent damage to 15 minutes of
ischeamia at 27ºC [19]. HT also expedites the recovery of ATP
stores following ischeamia, as well as improving the return of
energy metabolism to pre-ischeamic levels [20]. The combination
of reduced demand and improved recovery both during and after
ischeamic episodes is perhaps enough to explain the outstanding
neuroprotection afforded by intra-ischeamic HT.
Overstimulation of the NMDA subtype of glutamate receptor,
is a serious component of the ischemic cascade, it’s very early
occurrence means it is likely to remain a frustrating target for
therapeutic intervention. There are certain evidences that
suggesting HT reduces, or at least delays, the release of glutamate
from ischeamic neurons, probably by delaying the onset of
anoxic depolarization [21]. Using a cardiac arrest model, it was
shown that HT (31ºC/20min) either during ischemia or initiated
at the time of reperfusion reduced extracellular glutamate
concentrations (measured at the hippocampus) [22-24].
Why HT is considered a powerful neuroprotectant?
1. It is the only neuroprotective treatment proven effective in large randomized trials in patients with acute brain
injury [25-27].
2. Animal studies indicate a robust benefit of hypothermia
after focal cerebral ischaemia [28].
Depth of Hypothermia
The effectiveness of HT increases as its depth increases, though
the response is not linear. In a large meta-analysis of animal
studies, Van Der Worp et al., found that the greatest therapeutic
response (reducing mean infarct volumes by approximately
55%) was achieved by cooling to below 30°C, though cooling
to even 35°C, the highest level of HT included, still resulted in a
considerable positive response by decrease in infarct volume up
to 30% [29].
It is worth considering here the use of HT during cardiothoracic
and neurosurgical procedures, in which body temperatures are
lowered from anywhere from 26-35°C, specifically to protect
tissues, including the brain, during an anticipated period
of compromised blood supply. For example during cardiac
surgery, there are two distinct levels of HT that are commonly
used; a target body temperature of 34-35°C is now becoming
accepted as the standard for Cardiopulmonary Bypass (CPB),
while in especially critical cases surgeons may opt to use Deep
Hypothermic Circulatory Arrest (DHCA) in which patients are
cooled to a rather extreme 15-26°C [30].
The adverse effects of HT treatment such as cardiac arrhythmias,
coagulopathies and immunosuppression also increase with
increasing depth, as do the technical difficulties. Therefore, the
optimum target will be the best equilibrium between therapeutic
effects versus detrimental effects versus practicality. While the
finest target temperature is still to be determined, based on
preclinical and clinical studies it will probably be in the range 33
to 35°C, and is referred to as moderate or mild HT.
Timing and Duration
The pathophysiology of cerebral ischeamia is dynamic and
complex, with numerous critical mechanisms taking place and
lasting for different durations. It is an overview to say that
HT reduces the impact of all of these destructive processes.
Consequently, the earlier HT is initiated and the longer it is
upheld while the ischeamic damaging processes are occurring
will license the maximum neuroprotection.
In an animal study, of focal cerebral ischeamia, diverse
pathophysiological effects that are invoked exert their deleterious
effects over different time course extending from early hours to
several days following vessel occlusion [31]. Such observations
would suggest the need of HT to be prolonged. In addition, two
studies compared the effect of cooling under ≤ 12 hrs and 3
hrs found considerably larger benefits in 12 hrs of HT duration
[32,33].
However, longer treatment durations consume more resources
and also increase the health risks, mainly in patients who
require sedation or anesthesia to keep the hypothermic state.
The optimum duration of HT will most likely be in the range
12-48 hours, and is likely also to be reliant on factors such as the exact cause of ischeamia (stroke, cardiac arrest), severity
of ischeamia, age of patient and the time delay to commencing
HT after ischeamia. In terms of therapeutic window, this will
vary depending on the type of ischeamia (focal vs global) and
severity. With respect to rewarming it is becoming increasingly
accepted that slow rewarming at the rate of 0.2-0.3°C/hour is
most desirable [34].
Cooling Techniques
One of the most significant barriers to HT treatments is technical
strain involved in persuading the target temperature in the target
tissue in an appropriate and safe manner. Available techniques
are surface cooling by refrigerated blankets, cooling helmets,
cold air blowers, intravascular heat exchangers, intravascular
cold fluids and intranasal evaporative cooling [35]. These have
advantages and disadvantages in cost, accuracy, degree of
control, rate of cooling and ease of application. Mild HT can be
induced in awake patients, as long as steps are taken to manage
the related discomfort but moderate to deep HT requires sedation
or anaesthesia with intubation, ventilation and intensive care
measures.
At present the intravenous infusion of cold salt solutions (4°C) at
a rate of 20-30 ml/kg over 20-30 minutes is gaining acceptance
as the method of choice to induce HT [36-38]. The cold saline
infusion procedure has several attractions as it is inexpensive,
safe, fast at bringing mild to moderate HT (33-35°C) and suited
for use in both comatose and awake patients [38].
To further support the induction of HT the use of pethidine
alone or with other agents, such as, the anxiolytic buspirone
or magnesium are being used [39-41]. The use of these agents,
along with simple measures such as warm gloves and socks is
especially useful when inducing HT as it minimizes complications
such as shivering [41].
Combination with Other Treatments
A large advantage of HT is that it has been shown to act
synergistically with some other neuroprotective approaches. It is
especially important that any potential stroke treatment should
be compatible with tPA thrombolysis, and in this respect it
appears based on in vitro data that at least for mild hypothermia
(i.e., 35°C), it will not significantly reduce the effectiveness of tPA.
Concluding Remarks and Future Perspectives
There is compelling experimental and clinical evidence that mild
to moderate HT is effective following global and focal cerebral
ischemia. However, it is likely that the depth and duration of HT
that provides the best benefit to patients will vary depending
on the type (global vs focal) and severity of brain ischaemia, the
time that HT is commenced, and patient age and presence of comorbidities
(diabetes, hypertension, obesity). Therefore further
experimental and clinical trials will be required to determine HT
protocols that best suit individual patients. Moreover, based
upon the available human studies, it appears that the use of HT,
in particular mild HT (35°C) is feasible and safe to implement
in clinical situations. In addition, based on current information
therapeutic hypothermia should be commenced as soon as
possible after the ischemic event, and maintained for durations
of 12-48 hours to achieve a sustained benefit in terms of
neuronal recovery and survival and functional benefits. To this
end, future experimental studies in global and focal ischemia
models and the results of the clinical stroke trials, will no doubt,
help address further refinement of therapeutic hypothermia
protocols to better suit individual cases. In addition, evaluation
of the effectiveness of hypothermia in combination with other
potential neuroprotective agents such as magnesium, caffeinol,
glutamate antagonists and anti-oxidants could further improve
efficiency.
REFERENCES
- Diringer MN, Edwards DF, Mattson DT, Akins PT, Sheedy CW, et al., (1999) Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke 30: 724-728.
Google Scholar, Crossref, Indexed at
- Cambell K, Knuckey NW, Meloni BP (2010) Cerebral Ischmia and Post-iscemic Treatment with Hypothermia. Adv Treat Ischemic Stroke.
- Brouns R, De Deyn PP (2009) The complexity of neurobiological processes in acute ischemic stroke. Clin Neurol Neurosurg 111: 483-495.
Google Scholar, Crossref, Indexed at
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333: 1581-1587.
Crossref, Indexed at
- Adams Jr HP, Davis PH, Leira EC, Chang KC, Bendixen BH, et al., (1999) Baseline NIH Stroke Scale score strongly predicts outcome after stroke: A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 53: 126-131.
Google Scholar, Crossref, Indexed at
- Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, et al. (1999) Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 282: 2003-2011.
Google Scholar, Crossref, Indexed at
- Maher J, Hachinski V (1993) Hypothermia as a potential treatment for cerebral ischemia. Cerebrovasc Brain Metab Rev 5: 277-300.
Google Scholar, Indexed at
- Busto R, Globus MY, Dietrich WD, Martinez E, Valdés I, et al. (1989) Effect of mild hypothermia on ischemia-induced release of neurotransmitters and free fatty acids in rat brain. Stroke 20: 904-910.
Google Scholar, Crossref, Indexed at
- Ginsberg MD, Sternau LL, Globus MY, Dietrich WD, Busto R (1992) Therapeutic modulation of brain temperature: relevance to ischemic brain injury. Cerebrovasc Brain Metab Rev 4: 189-225.
Google Scholar, Indexed at
- Karibe H, Chen J, Zarow GJ, Graham SH, Weinstein PR (1994) Delayed induction of mild hypothermia to reduce infarct volume after temporary middle cerebral artery occlusion in rats. J Neurosurg 80: 112-119.
Google Scholar, Crossref, Indexed at
- Fay T (1943) Observation on generalized refrigeration in cases of severe cerebral traum. Assoc Res Nerv Ment Dis Proc 24: 611-619.
Google Scholar
- Stoney WS (2009) Evolution of cardiopulmonary bypass. Circulation 119: 2844-2853.
Google Scholar, Crossref
- Busto R, Dietrich WD, Globus MY, Valdés I, Scheinberg P, et al. (1987) Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab 7: 729-738.
Google Scholar, Crossref
- Buchan A, Pulsinelli WA (1990) Hypothermia but not the N-methyl-D-aspartate antagonist, MK-801, attenuates neuronal damage in gerbils subjected to transient global ischemia. J Neurosci 10: 311-316.
Google Scholar, Crossref, Indexed at
- Marion DW, White MJ (1996) Treatment of experimental brain injury with moderate hypothermia and 21-aminosteroids. J Neurotrauma 13: 139-147.
Google Scholar, Crossref, Indexed at
- Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, et al. (2002) Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 346: 557-563.
Google Scholar, Crossref, Indexed at
- Hypothermia after Cardiac Arrest Study Group (2002) Mild therapeutic hypothermia to improve the neurological outcome after cardiac arrest. N Engl J Med 346: 549-556.
Google Scholar, Crossref, Indexed at
- Busto R, Dietrich WD, Globus MY, Ginsberg MD (1989) The importance of brain temperature in cerebral ischemic injury. Stroke 20: 1113-1114.
Google Scholar, Crossref, Indexed at
- Schaller B, Graf R (2003) Hypothermia and stroke: the pathophysiological background. Pathophysiol 10: 7-35.
Google Scholar, Crossref
- Erecinska M, Thoresen M, Silver IA (2003) Effects of hypothermia on energy metabolism in Mammalian central nervous system. J Cereb Blood Flow Metab 23: 513-530.
Google Scholar, Crossref
- Zhao H, Steinberg GK, Sapolsky RM (2007) General versus specific actions of mild-moderate hypothermia in attenuating cerebral ischemic damage. J Cereb Blood Flow Metab 27: 1879-1894.
Google Scholar, Crossref, Indexed at
- Takata K, Takeda Y, Sato T, Nakatsuka H, Yokoyama M, et al. (2005) Effects of hypothermia for a short period on histologic outcome and extracellular glutamate concentration during and after cardiac arrest in rats. Crit Care Med 33: 1340-1345.
Google Scholar, Crossref, Indexed at
- Hachimi-Idrissi S, Huyghens L (2004) Resuscitative mild hypothermia as a protective tool in brain damage: is there evidence? Eur J Emerg Med 11: 335-342.
Google Scholar, Crossref, Indexed at
- Hachimi-Idrissi S, Yang X, Nguyen DN, Huyghens L (2004) Combination of therapeutic mild hypothermia and delayed fluid resuscitation improved survival after uncontrolled haemorrhagic shock in mechanically ventilated rats. Resuscitation 62: 303-310.
Google Scholar, Crossref
- Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG (2013) Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev 2013: CD003311.
Google Scholar, Crossref, Indexed at
- van der Worp HB, Sena ES, Donnan GA, Howells DW, Macleod MR (2007) Hypothermia in animal models of acute ischaemic stroke: a systemic review and meta analysis. Brain 130: 3063-3074.
Google Scholar, Crossref
- Choi R, Andres RH, Steinberg GK, Guzman R (2009) Intraoperative hypothermia during vascular neurosurgical procedures. Neurosurg Focus 26: E24.
Google Scholar, Crossref, Indexed at
- Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 22: 391-397.
Google Scholar, Crossref, Indexed at
- Yanamoto H, Hong SC, Soleau S, Kassell NF, Lee KS (1996) Mild postischemic hypothermia limits cerebral injury following transient focal ischemia in rat neocortex. Brain Res 718: 207-211.
Google Scholar, Crossref, Indexed at
- Yanamoto H, Nagata I, Nakahara I, Tohnai N, Zhang Z, et al. (1999) Combination of intraischemic and postischemic hypothermia provides potent and persistent neuroprotection against temporary focal ischemia in rats. Stroke 30: 2720-2726.
Google Scholar, Crossref, Indexed at
- Bardutzky J, Schwab S (2007) Antiedema therapy in ischemic stroke. Stroke 38: 3084-3094.
Google Scholar, Crossref
- Jing L (2007) Cooling strategies and transport theories for brain hypothermia resuscitation. Front Energy Power Eng 1: 32-57.
Google Scholar, Crossref, Indexed at
- Van Zanten ARH, Polderman KH (2005) Early induction of hypothermia: will sooner be better? Crit Care Med 33: 1449-1452.
Google Scholar, Crossref, Indexed at
- Moore K (2008) Hypothermia in trauma. J Trauma Nurs 15: 62-64.
- Bernard SA, Rosalion A (2008) Therapeutic hypothermia induced during cardiopulmonary resuscitation using large-volume, ice-cold intravenous fluid. Resuscitation 76: 311-313.
Google Scholar, Crossref
- Kliegel A, Janata A, Wandaller C, Uray T, Spiel A, et al. (2007) Cold infusions alone are effective for induction of therapeutic hypothermia but do not keep patients cool after cardiac arrest. Resuscitation 73: 46-53.
Google Scholar, Crossref
- Mokhtarani M, Mahgoub AN, Morioka N, Doufas AG, Dae M, et al. (2001) Buspirone and meperidine synergistically reduce the shivering threshold. Anesth Analg 93: 1233-1239.
Google Scholar, Crossref
- Zweifler RM, Voorhees ME, Mahmood MA, Parnell M (2004) Magnesium sulfate increases the rate of hypothermia via surface cooling and improves comfort. Stroke 35: 2331-2334.
Google Scholar, Crossref
- Campbell K, Meloni BP, Knuckey NW (2008) Combined magnesium and mild hypothermia (35 degrees C) treatment reduces infarct volumes after permanent middle cerebral artery occlusion in the rat at 2 and 4, but not 6 h. Brain Res 1230: 258-264.
Google Scholar, Crossref, Indexed at
- Zhu H, Meloni BP, Bojarski C, Knuckey MW, Knuckey NW (2005) Post-ischemic modest hypothermia (35 degrees C) combined with intravenous magnesium is more effective at reducing CA1 neuronal death than either treatment used alone following global cerebral ischemia in rats. Exp Neurol 193: 361-368.
Google Scholar, Crossref, Indexed at
- Schwarzenberg H, Müller-Hülsbeck S, Brossman J, Glüer CC, Bruhn HD, et al. (1998) Hyperthermic fibrinolysis with rt-PA: in avitro results. Cardiovasc Intervent Radiol 21: 142-145.
Google Scholar, Crossref, Indexed at
Citation: Mathur M, Bayraktutan U (2022) Hypothermia as a Treatment Option for Intra and Post Ischemic Stroke. J Neurol Neurosci Vol.13 No.2:411