Keywords
Pediatric, Children, Sepsis, Septic shock in pediatrics, Emergency department, Emergency room, Pediatric Intensive care unit, PICU, ED, ER
Introduction
Septic shock in and of itself is frightening. Severe sepsis and septic shock constitute a relevant cause of morbidity and mortality in critically ill children [1]. Septic shock still represents a clinical challenge even in developed countries, being a leading causes of admissions to the pediatric emergency department and the pediatric intensive care unit. In the management of septic shock, early diagnosis and rapid treatment have the maximum impact on clinical course and patient outcome [2]. Undeniably, early recognition of septic shock and institution of antibiotic therapy can reduce mortality in children [3]. Septic shock in children is a clinical challenge for all healthcare providers, but especially in the nonpediatric emergency department. Early diagnosis, allowing rapid therapeutic intervention, is essential in improving the outcome of these patients.
The goals of the Doctor of Nursing Practice (DNP) project included identifying the barriers to successful interventions of pediatric shock patients in non-pediatric emergency departments and to successfully implement a goal-directed guideline for pediatric septic shock in specifically chosen non-pediatric emergency departments in the Central Valley. The vision of this project is that every emergency department will be noted for its commitment to quality and excellence and offer the finest possible service in emergency physician leadership, management, clinical care, patient satisfaction, and pediatric patient safety.
Problem statement
Despite tremendous advances, the morbidity and mortality attributed to pediatric sepsis remain unacceptably high and pediatric patients who arrive in non-pediatric emergency departments in septic shock and are left unrecognized are at a risk for deterioration. The rapid recognition of septic shock is essential as early reversal of shock results in an improved outcome.
Since signs of early septic shock may be subtle and the condition dynamic there is a danger of overlooking them in a busy emergency department. The patient may not always adhere to the classic stages of shock described in textbooks. The problem with sepsis/septic shock exists all across the country, however this project focused on the barriers to caring for pediatric septic shock patients in Central Valley emergency departments that are eventually transferred to Children’s Hospital Central California.
Purpose
The DNP project focused primarily on identifying the barriers to implementation of successful interventions for pediatric septic shock patients found in non-pediatric emergency departments. The 2006 Institute of Medicine (IOM) report Emergency Care for Children: Growing Pains use the word “uneven” to describe the current status of pediatric emergency care in the United States (IOM, 2006). The literature identified several barriers that limit adherence to current guidelines, including lack of early recognition of severe sepsis and septic shock as well as treatment delay, difficulties in obtaining adequate vascular access and advanced airway management, central venous pressure and central venous oxygen saturation monitoring, shortage of health care providers, absence of goals and treatment protocols, difficulties in obtaining specialized transport and access to pediatric intensive care beds, as well as educational gaps [4-6].
Pediatric septic shock is a frequently occurring disease condition that is associated with high morbidity and mortality [7]. Shock is an acute, complex state of circulatory dysfunction resulting in failure to deliver oxygen and nutrients to meet metabolic demands which are usually increased during shock. If left untreated, multiple organ failure and ultimately death will occur [8]. This strongly points out the importance of early recognition and aggressive treatment of children with shock. Comparable to adults, such an approach – termed early-goal directed therapy (EGDT) – has been shown to significantly reduce mortality in pediatric septic shock [4]. Several lines of evidence indicate that early identification and treatment of severe sepsis and septic shock improve outcomes. Early initiation of hemodynamic resuscitation with specified treatment endpoints has consistently improved mortality rates in numerous clinical trials [4].
Mortality rates increase as the patient progresses through this time-sensitive pathology. Every hour’s delay in resuscitation in the emergency department results in a 40% increase in mortality in children with septic shock [9]. Severe sepsis remains one of the leading causes of death in children with greater than 4,300 deaths annually and an estimated cost of $1.97 billion [10]. Each case of pediatric shock possesses unique features for the initial examiner and is capable of confounding even experienced physicians [11]. Fisher et al. indicated that the clinical course in pediatric shock is a dynamic process with a wide etiological spectrum and variable physical finding.
Theoretical framework
Knowles Learning Theory
The learning theory used for this project was Knowles theory of learning. Knowles made four assumptions about adults as learners. First, adults tend to be more self-directed as a result of their maturity; secondly, adults possess personal histories which defines their identities and serve as a resource of experiential learning upon which new learnings can be applied; thirdly, motivation in adults is directed to more socially relevant learning; and lastly, adult learners have interest in immediate application for problem-solving [12]. This learning theory applied to this project best because of the population surveyed. Nurses are adult learners and learn best by giving them the information and allowing them to apply it to practice.
According to Knowles [13], adults become ready to learn those particular things they need to know and do so they can cope effectively with their real-life situations. In short, it is easier for people to learn when they are developmentally capable of it and feel the need to learn it. When choosing a learning theorist/theory for this authors project, Malcolm Knowles’ theory of teaching adults unparalleled any other. Teaching adults’ means allowing them to make the decision there is something they need to learn.
Quality education is built around the concept of nourishing those intrinsic motivators [12]. Learning feeds on itself and suggests to the learner to become even more proficient in the job. In a classic study, Rogers [14] illustrated that when an adult learner has control over the nature, timing, and direction of the learning process, the entire experience is facilitated. Adults have a need to be selfdirected, deciding for themselves what they want to learn. They enter into the learning process with a goal in mind and generally take a leadership role in their learning. The challenge for educators is to be encouraging to the learner but also reinforce the process of learning. The endpoint of learning cannot always occur quickly or on a pre-set timeline.
The research on learners has shown that adults learn differently from younger students. Adults have special needs as learners and these needs should be taken into consideration when planning education for adults. By using combinations of adult learner techniques and strategies, educators can create educational experiences that will enhance the learning of participants. Adults may not be motivated to learn what educators tell them to learn unless they perceive a need to learn. Learning activities should clearly demonstrate to the learner where he or she would benefit in their jobs.
Roger’s Diffusion of Innovation
Along with having substantial evidence to support the practice change, other strategies for change include planning, organization, buy-in from stakeholders, recruiting champions for the cause, being realistic regarding available time, resources, and applying the principles of change theory to affect change. Rogers [15] has developed one of the better-known theoretical approaches to diffusion of innovation. This theoretical framework is helpful when determining the adoption of specific clinical behaviors and when deciding which components will require additional effort if diffusion is to occur.
Three characteristics that Rogers identifies as central to the adoption of a change include the potential user’s perception of the benefit to practice, its compatibility with the practice setting and the population [15]. Clinicians need to know the why and the how to initiate a change in practice. They also need to understand the underlying theory or framework that explains how the innovation will work. Diffusion theory offers a plausible explanation for why some clinical activities are adopted rapidly and others only with difficulty, despite strong evidence of their potential benefits. Some clinical behaviors may be adopted relatively easily because of the nature of the behavior itself, while others may involve a complex interplay between social systems, communication style and the decision-making process [15].
There is a need to prospectively test the assumptions of the model in the healthcare environment using rigorous experimental design. Rogers’ innovation-diffusion theory states that users’ acceptance of an innovation is influenced by their perception of its relative advantage [15]. Research provides information on the costeffectiveness and potential benefit to patients of implementing a new clinical activity. However, the objective data may be less important than the clinician’s perception of whether the innovation will be advantageous [15]. Decisions about implementing bestevidence practice are driven not only by patient welfare but also by the relationship between the interests of the patient, the clinician and the healthcare system.
Review of Literature
Literature review
An extensive literature review was completed by this author using a systematic approach. The inclusion criteria was pediatric patients with a diagnosis of sepsis to septic shock or both, either in a pediatric intensive care unit or a non-pediatric emergency department setting. This independent review of the literature examines the recent pathogenic, diagnostic, and therapeutic advances in severe sepsis and septic shock for pediatric patients, with particular relevance to non-pediatric emergency practice. Databases utilized included: PubMed, Up-to-Date, Cochrane, CINHAL, and evidenced based journals. MESH words included: pediatric, children, sepsis, septic shock in pediatrics, emergency department, emergency room, pediatric intensive care unit, PICU, ED, and ER.
Although adherence to published guidelines for the management of severe sepsis and septic shock patients is known to lower mortality, actual adherence to these recommendations is low [4]. The aim of this review was to explore the initial management of pediatric patients with severe sepsis/septic shock, as well as discover the main barriers to the adherence to current guidelines on management of these patients.
In analyzing the literature, for more than two decades the endpoints for pediatric septic shock are clear. Early recognition and goal directed therapy are crucial to the survival of these patients. In fact most of the studies have proven outcomes of decreased mortality. Recent studies have led to a better understanding of the pathogenic mechanisms and the development of new or newly applied therapies [16]. These therapies place early and aggressive management of severe sepsis and septic shock as integral to improving outcomes.
In one study of 96 episodes of pediatric septic shock, 13 of 70 occurrences of septic shock and multiple organ system failure resulted in death, as opposed to none of the other 26 occurrences with septic shock without organ failure [17]. In comparison, [18] demonstrated in a randomized controlled study that the key to successful implementation in the emergency department of goal-directed therapy of septic shock and severe sepsis with hypo-perfusion was aggressive early intervention. In a retrospective study by Caricillo et al., [19] pediatric survivors of septic shock were found to have received an average of 42 ml/kg over the first hour of resuscitation, whereas non-survivors had received only an average of 23 ml/kg over the first hour. By the end of the first six hours, both survivors and non-survivors ended up receiving similar volumes.
Results from a study by Han, et al. [5] showed that compliance with the Academy of Critical Care Medicine (ACCM) and Pediatric Advanced Life Support (PALS) guidelines as seen in Appendix F, was associated with early shock reversal and improved survival. The mortality rate was eight percent for patients who were treated in compliance with the guidelines compared to thirty-eight percent for patients who were not.
Numerous studies have proven results that aggressive fluid resuscitation with crystalloids or colloids is essential to improve survival in children with septic shock [5,19,20] In an acute shock situation vascular access is one of the priorities after airway and breathing are secured. This is often difficult in pediatric patients because of the physiologic processes of shock with resulting vascular constriction. In a comparison study by Kanter et al., [21] establishing an emergency intravascular access is crucial in the resuscitation process whether it be peripheral or intraosseous access. Another comparison study identified lack of vascular access, lack of early septic shock diagnosis, and lack of treatment protocols as barriers to rapid fluid resuscitation [6]. According to Oliveira et al., [6], emergency department physicians and pediatric intensivists reported pseudo uniform adherence to current recommendations in the management of pediatric septic shock and severe sepsis with respect to antibiotic administration and rapid fluid resuscitation. The data reviewed was overwhelmingly in favor of goal-directed therapy for all pediatric patients with severe sepsis/septic shock.
Overcoming the barriers
In reviewing the literature many solutions were proposed, the most significant being the American Heart Association’s (AHA) 2010 guidelines [22]. The inflammatory triad of hyperthermia, increased heart rate, and vasodilation is a fairly benign indication of septic shock in pediatrics, but the addition of altered mental status manifested by irritability, drowsiness, confusion, and/or poor interaction [9] adds another portion to the conundrum. Health care providers in non-pediatric emergency departments may still feel that the above clinical picture is still unclear and may not be suggestive of shock. As this disease process progresses, signs of septic shock become more apparent as the patient becomes more altered, urine output decreases along with cardiac output and liver function. The patient begins to have a widened pulse pressure that eventually deteriorates to a hypotensive state. It is critical to identify septic shock in its earliest stages as aggressive early treatment is necessary for optimal outcome [22].
As soon as the healthcare provider identifies septic shock at any point, the AHA’s guidelines for obtaining adequate tissue perfusion should be instituted. These guidelines include high flow oxygen and rapid fluid resuscitation of 20 ml/kg up to 60 ml/kg. If the blood pressure is refractory to fluid resuscitation, inotrope initiation should be instituted, preferably dopamine or epinephrine for cold shock and norepinephrine for warm shock [22]. Continuing on the Pediatric Advanced Life Support (PALS) shock algorithm, the administration of catecholamine is recognized as the next step for those patients at risk for absolute adrenal insufficiency. The American Heart Association assessment parameters are specific to the pediatric population as are the recommended treatments. Educating to these guidelines is crucial as it is reflective of an abundant amount of research and best practice. The comfort of caring for pediatric patients comes from many years of experience. Caring for critically ill pediatric patients takes a finesse of quickly recognizing that the child needs immediate intervention to produce a positive outcome.
Razzak [23] indicated that there are delays in recognition of the disease process and institution of appropriate therapy, especially in the emergency department due to patient volumes and time constraints of the care provider. The initiation of treatment can hit barriers due to physician failure, system delays and, work-up delays, comfort of the health care provider with a pediatric patient, as well as recognition of the pathophysiology. Kisson et al. [9] stated that the inflammatory triangle of fever, tachycardia, and vasodilation is a common sign of benign infections in children who present to the ED. Septic shock is suspected when children with this triad have a change in mental status manifested as irritability, inappropriate cry, drowsiness, confusion, poor interaction with parents, and lethargy by Kasson et al. [9]. Kasson et al. [9] also indicated that clinical diagnoses are made in children that have suspected infection, manifested by hypothermia or hyperthermia, and have clinical signs of inadequate tissue perfusion. Recognition of septic shock in its early stages and applying appropriate interventions is not consistent and has led to increased cost and mortality [24].
The American College of Critical Care Medicine has published practice guidelines incorporated into the American Heart Association Pediatric Advanced Life Support courses [25]. The definition of septic shock in children differs from adults and includes sepsis and cardiovascular organ dysfunction, but hypotension is not required to meet criteria as it is in adults. Care for septic shock that is delivered early in the emergency department will enhance outcomes. The rapid recognition of septic shock is essential as early reversal of shock results in an improved outcome [26]. Sepsis is a clinical diagnosis and does not rely on the isolation of the causative infectious organism. Since signs of early septic shock may be subtle and the condition dynamic, there is a danger of overlooking them in a busy emergency department according to Cruz [27]. The pediatric patient may not always adhere to the classic stages of shock described in textbooks. The hallmark of septic shock is decreased perfusion. For children changes that occur before the onset of hypotension are the recognized clinical triad of hyper or hypothermia, altered mental status and peripheral vasodilation or vasoconstriction [28]. Any change in mental status of a febrile child should prompt immediate consideration of septic shock.
The Joint Commission and the American Academy of Pediatrics (AAP) have partnered together to create a culture of safety in all emergency departments who provide emergency care to children [29]. As the majority of children seeking emergency care are thankfully not severely ill or injured, the ongoing experience in the assessment and management of very ill or critically injured children for the clinical staff in these emergency departments is limited. The Institute of Medicine (IOM) has noted that many hospital EDs are not equally capable of caring for children and adults, and that the needs of children, at times, have been overlooked [30]. The evidence is clear and even though the studies for children are limited there is an overwhelming consensus that early recognition and early intervention of care in the septic shock pediatric patient improves outcomes.
Innovation
According to Schumpeter innovation is a significant and permanent change in the way of doing things. One of the goals for this project is to invoke permanent change in non- pediatric emergency departments and the way they care for septic shock children. Change is never an easy project but the nature of effective leadership and change innovation is a key factor in the life and success of an organization. Leadership transforms potential into reality and good leaders propose new paradigms when old ones lose their effectiveness. Leadership is a major way in which people change the minds of others and move departments and organizations forward to accomplish identified goals. There are many leadership theories however transformational leadership theorizes to inspire followers to perform beyond expectations and is currently the most widely studied leadership theory [31]. Research evidence clearly shows that groups led by transformational leaders have higher levels of performance and satisfaction than groups led by other types of leaders [32]. Transformational leaders hold positive expectations for followers, believing that they can do their best and as a result, they inspire, empower, and stimulate followers to exceed normal levels of performance.
All innovation champions of Central Valley emergency departments will need to hold followers to high expectations and will need to be unquestionably transformational leaders. They will have to inspire, empower and stimulate their people every day with the care they provide to children. Their support of this project goes without saying and they will need to be the top change agents if the project is to be successful. Most health care providers want to do what is right for children and finding a balance and direction to implement this project will be epic.
Methodology
Chart review
The scientific and systematic investigation of existing health records is an important and valued methodology in health care research, specifically in epidemiology, quality assessment studies, and emergency medicine [33]. A retrospective chart review was completed for this project at Children’s Hospital Central California with the hospital Institutional Review Board approval to determine where the survey questionnaire would be directed. One hundred patient charts were reviewed for this project with criteria of demographic information, sepsis/septic shock admission diagnosis, length of stay, as well as the unit the patient was admitted to whether it was the Pediatric Intensive Care Unit or the Acute Care Unit.
As principle investigator all medical records accessed for this project were currently in existence at the time of the Institutional Review Board submission. The desired medical record data was recorded by the investigator in such a way that the patients cannot be identified either directly, or indirectly via linkage codes assigned to the data. This means that the investigator cannot link names, social security numbers, or any other patient identifiers to the data set. As a consequence, the resulting research data set is necessarily completely anonymous. For that reason, once the information has been extracted from the medical record, it will never be possible for the investigator to go back to the medical record and add other patient-specific information to this research dataset.
Survey
A survey is a systematic method of collecting data from a population of interest. It tends to be quantitative in nature and aims to collect information from a sample of the population such that the results are representative of the population of interest. One potential advantage of online survey is that it is relatively easy to collect data from multiple participants to compare responses to the same questions. Most recent research show that no significant differences exist in the qualitative and quantitative data quality between online and other survey modes [34]. There are disadvantages to online survey and the most discussed key disadvantages of online survey include low coverage of population, sample self-selection as well as the non-response error because participants are not familiar with the survey formation [35].
For this project a survey questionnaire was sent to twelve identified Central Valley, California emergency departments via Survey Monkey (Appendix A). The questionnaire focused on the objective of identifying the barriers to caring for pediatric patients in general and then pediatric septic shock patients. The survey was completely anonymous in a non- intimidating survey environment. Each survey was coded so that only the hospital it came from could be identified. Once the data was collected all possible identifying information was deleted. It was felt that an online survey best suited the privacy needs of the participants and the likelihood of responses was much more insured. As the survey was developed every question added value as it moved closer to the objective. The questions included multiple choice questions and free text items to allow for reasons behind the responses. These allowed for useful insights as to identification of the barriers.
The purpose of the questionnaire aimed at identifying the barriers to successful implementation of treatment for pediatric patients found in non-pediatric emergency departments with sepsis/septic shock. The information collected will eventually be used to develop an education program for outreach service in the Central Valley of California. Completing the survey involved no risk to the participants and although the results of this study may be published, no information that could identify the participants will be included. As the participants moved through the survey they were able to respond to the multiple choice questions but also respond in the free text box if they chose to do so.
Participants
The participants for this project were chosen based on the retrospective chart review and the emergency department where the pediatric patient were transferred from. The educator for each hospital was asked to send out the survey to nurses, nurse practitioners, physician assistants if there were any, and physicians. The only demographic was greater than or less than five years of emergency department experience and what type of healthcare provider they were. No other identifying information was gathered. The surveys were coded so that only the principal investigator would know which hospital they were sent from during data collection.
Results
From October 2013 to January 2014, a survey was conducted among twelve Central Valley emergency departments where the survey was sent to physicians, nurses, and nurse practitioners or physician assistants if applicable to the emergency department. The purpose of the survey was to discover the barriers to implementation of treatment of pediatric patients with a diagnosis of sepsis/septic shock. The survey was conducted by means of an online questionnaire using Survey Monkey (Appendix A) with an expected response date of no later than January 31, 2014. The data collected was significant in that it showed that most of the healthcare providers (n = 687) felt there was some kind of barrier in their emergency department when caring for pediatric patients (Appendix B). The data was also significant because the response was overwhelming with the amount of participants. The data for the individual health care providers is included in Appendix C, D, and E.
Nurses
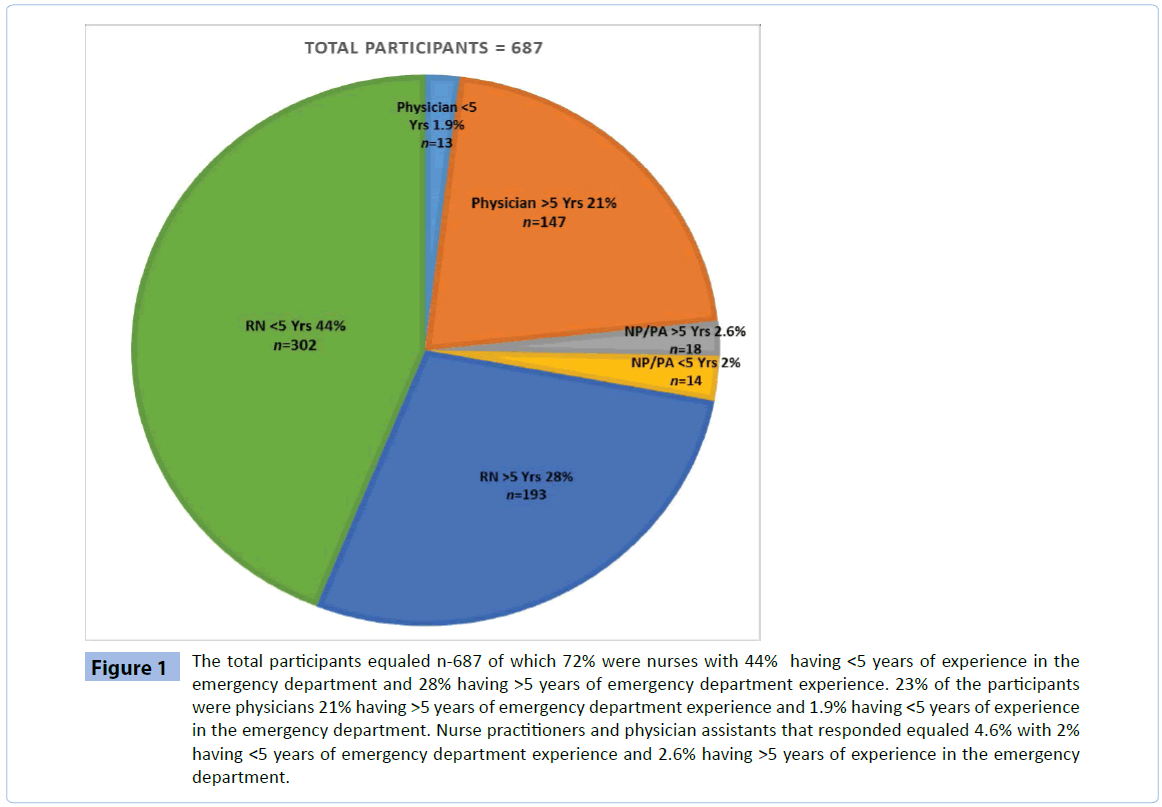
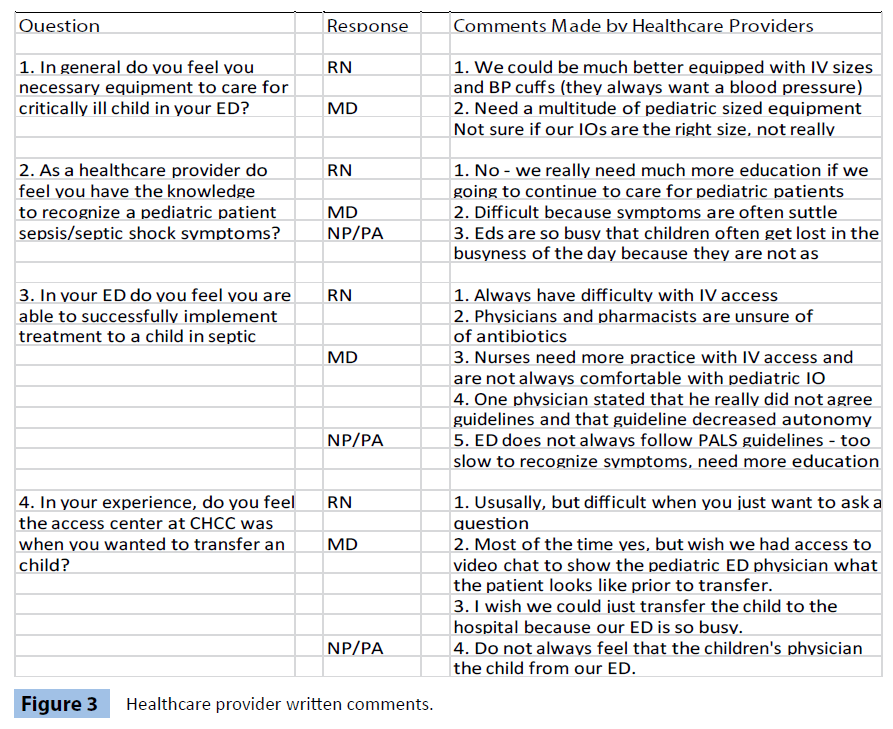
Of the participants, the nursing staff responses were the most significant (n = 495) of which 44% (n = 302) had less than five years of nursing experience. This was kind of frightening as these are the nurses who are put out at the triage desk and left to recognize that a child may be in a shock state. 28% (n = 193) of the nursing participants had greater than five years of emergency department experience (Figure 1). 100% of the nurses responded that they would like to have further education about caring for pediatric patients in their emergency department along with 100% responded that there were many barriers to caring for pediatric patients in their emergency department especially critically ill patients. Some of the comments made by the nurse that responded included that they always have difficulty with IV access especially if the child is critically ill and they would really like to have more education and the ability to practice more. The nurses also states that they could be much better equipped with IV sizes and blood pressure cuffs for example. One person stated that when they call to give nurse to nurse report to Children’s “they always want a blood pressure” (Figure 2).
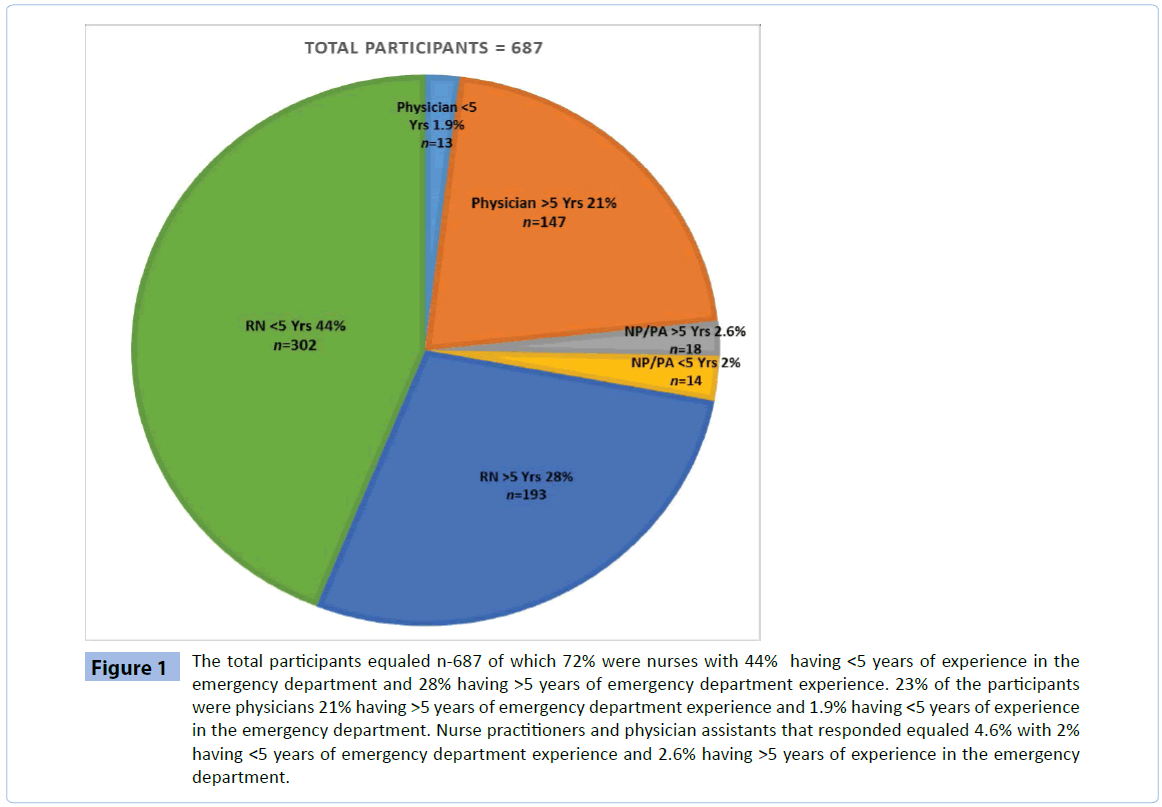
Figure 1: The total participants equaled n-687 of which 72% were nurses with 44% having <5 years of experience in the emergency department and 28% having >5 years of emergency department experience. 23% of the participants were physicians 21% having >5 years of emergency department experience and 1.9% having <5 years of experience in the emergency department. Nurse practitioners and physician assistants that responded equaled 4.6% with 2% having <5 years of emergency department experience and 2.6% having >5 years of experience in the emergency department.

Figure 2: A compilation of healthcare provider responses and the average percentage of how the survey questions were answered. Of note 100% of the participants responded that they would want further education in the care of pediatric patients. A significant amount of participants (87%) also responded that they had barriers in the emergency department when caring for pediatric patients. 84% responded that there was a knowledge deficit and 82% responded they did not have the right equipment to care for pediatric patients.
Nurse practitioners/Physicians assistants
Of the nurse practitioners/physician assistants (NP/PA) (n = 32) that responded 2% had less than five year of emergency department experience and 2.6% had greater than 5 years of experience in emergency medicine (Figure 1). Many of the NP/PAs were not comfortable with pediatric patients in their emergency departments and deferred care to the physician. Comments from this group of participants included that their emergency departments are often busy and children get lost in the busyness of the day because their symptoms are frequently subtle. The NP/PA group also commented that their emergency department does not always follow the PALS guidelines and that they are too slow to recognize sepsis and septic shock in pediatric patients. This group also commented that there was a definite need for further education with pediatric patients (Figure 2).
Physicians
Of the physicians that responded, (n = 160), 1.9% responded they had less than five years of emergency department experience and 29% responded they had greater than five years of experience in emergency medicine and yet they still fail to recognize septic shock in pediatrics (Figure 1). Most physicians felt there were barriers in their emergency department and could use more education to care for pediatric patients. One suggested the use of video conferencing in order for the pediatric emergency physician to actually see the patient prior transfer. Others responded that their emergency department was busy and they wished they could just transfer the child out to the children’s hospital. One physician stated that he really did not agree with the guidelines and that guideline decreased autonomy. Still more responded that symptoms displayed by children are so subtle that sepsis and septic shock are often missed (Figure 3).
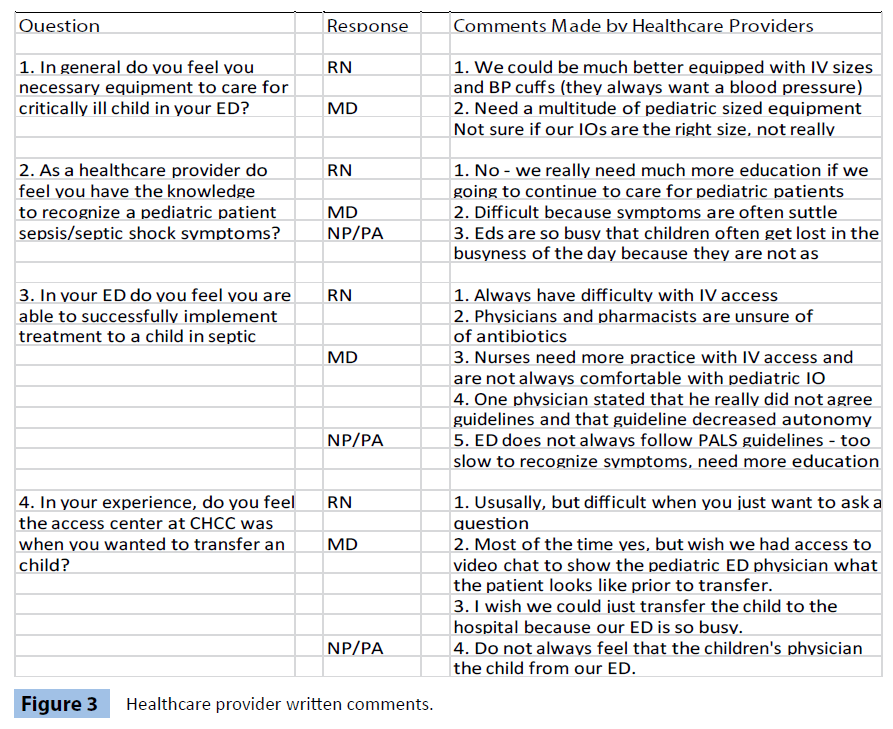
Figure 3: Healthcare provider written comments.
The results of the survey were broken down by healthcare provider and then as a compilation of results using an average percentage of all healthcare providers. The first question was to indicate how comfortable the health care provider felt they were with pediatric patients in general. 55% of the responses were slightly comfortable and 75% of the participants felt they were also slightly knowledgeable. However they are still not recognizing sepsis in these patients. The survey also asked if the healthcare providers felt there were barriers to caring for pediatric septic shock patients in their emergency department along with equipment and knowledge of septic pediatric patients. These results were surprising in that over 80% of the responses were that non-pediatric emergency department’s health care providers did feel they have barriers, lack of equipment and knowledge. What was disheartening is that these facilities know they have lack of equipment and knowledge but why? How can they not have what is necessary to care for these patients? Especially if they have agreed to be a full service emergency department! The communities where these children come live depend on their emergency departments to take care of them. What was exciting from all of this was that 100% of the participants wanted to be educated on pediatric patients so a future project is promising (Figure 2). A compilation of healthcare provider responses and the average percentage of how the survey questions were answered. Of note 100% of the participants responded that they would want further education in the care of pediatric patients. A significant amount of participants (87%) also responded that they had barriers in the emergency department when caring for pediatric patients. 84% responded that there was a knowledge deficit and 82% responded they did not have the right equipment to care for pediatric patients.
Within the survey, participants also had an opportunity to write in responses if they chose. Some of those responses included that the nurses were not comfortable putting an IV in pediatric patients and the physicians were not comfortable with intraosseous insertion. Some of the responses were that they just wished they could transfer the patient to us and then we could take care of them. Some of the responses were they felt the barriers were that their ED is often very busy and children get lost in the shuffle because of their subtle symptoms. Others felt that for the most part our access center was helpful but hard to get through if they just had a question. So access to help was often a barrier (Figure 3).
Discussion
The inconsistent clinical picture that sepsis and septic shock can present can cause hesitation in costly interventions. According to Vansant and Schmeltzer, if there is any doubt about whether the patient requires sepsis treatment, health care providers may choose less aggressive and less effective options in an effort to cut costs and risk. Perhaps a resolution to this fear is the utilization of lactate levels as a means of risk stratification and prognosis in the hemodynamically stable patient [36]. The use of lactate measurements is gaining recognition in medicine as a useful indicator of tissue hypo-perfusion. Furthermore, lactate screening as a method of risk stratification and prognosis has been shown to be beneficial in hemodynamically stable patients with suspected infection [36].
Efforts to improve care can be tedious and discouraging at times. Schorr [16] recognizes implementation of severe sepsis guidelines as an issue due to lack of administrative support, staff resistance, unfamiliar equipment, and inability to apply sepsis education in the clinical setting. As implementation proves to be problematic, researchers have hit their share of stumbling blocks as well. According to Dellinger et al. [2], over the past twenty years, thousands of patients have been enrolled in sepsis clinical trials with little success of overcoming identified barriers.
Limitations
Although this study only focused on the Central Valley of California, it is a beginning. What was not looked at were pediatric patients that came to Children’s Hospital Central California emergency department after they had been seen at another facility; partially treated; sent home; and the parents brought the child in on their own. When the child arrives to the ED they are quite ill because of under treatment and misdiagnosis days earlier. Another .limitation of this project included bias of the survey due to interpretation of the questions by each healthcare provider and that the survey was anonymous so the participants are completely unknown to the investigator.
Recommendations
Implementing an emergency department septic shock protocol and care guideline for children will improve compliance with fluid resuscitation and early antibiotic and oxygen administration. Unrecognized and undertreated septic shock increases morbidity and mortality. Consistent successful treatment of septic shock cannot begin in the intensive care unit for pediatric patients who present to the emergency department (ED) in shock; it must begin at the time of triage in the ED. Early recognition and treatment of septic shock benefits all ED patients, because the effort to recognize early shock leads to a more meticulous patient assessment from the initial encounter.
The future for sepsis and septic shock for the pediatric population definitely needs to include education. Health care providers want to do what is right for their pediatric patients but lack of knowledge can be detrimental. This project has laid the foundation for further development of an outreach educational project. It is with high expectation that there would be an implementation of a sepsis protocol in every non-pediatric Emergency Department that includes:
• A triage sepsis recognition tool
• Improved staffing of the resuscitation area
• Prioritization of antibiotic
• Improved graphic vital sign monitoring
• Decreased time to intravenous access and first bolus
• Decreased time to antibiotic administration
• That the physician group at Children’s Hospital Central California emergency department will help the outlying facilities by asking the right questions and not be judgmental
• Making sure that our outlying facilities have specific pediatric carts with the right equipment such as the correct intravenous sizes, intraosseous sizes, Broselow tape for estimated weight, blood pressure cuffs, etc.
• There could be an outreach education program set up by Children’s Hospital clinical educators including physicians
• A call back program could be set up to let referring facilities know how they did with the child they sent to Children’s Hospital Central California, whether the outcome was good or bad.
Every referring facility should call the tertiary facility early, stabilize the patient and then feel good about the outcome. As with all good questions this project added more. Another survey could be developed to ask Central Valley emergency departments:
• what equipment they do have to determine what their need is
• how can we open the lines of communication for access to Children’s experts.
• A further investigation could look at what patients came to Children’s Hospital Central California emergency department (ED) after they had been seen at another facility and partially treated and sent home and the parents bring the child to the ED and the child is quite ill because of under treatment and misdiagnosis.
• There could be mobile pediatric simulation education where education could be taken on the road to the outlying facilities and teach them how to put IVs and IOs in by practicing on fake arms and legs.
• Educating what the symptoms are to look for in pediatrics patients.
• A future study could also look at which facilities send the most patients to children's and start there with the education.
• The possibilities are endless.
The future for sepsis and septic shock for the pediatric population includes education. Health care providers want to do what is right for their pediatric patients but lack of knowledge can be detrimental to this population. This project has laid the foundation for further development of an outreach educational project. Non-pediatric emergency departments need to be ready for any pediatric patient that arrives in their facility. Every hour without treatment for sepsis/ septic shock increases mortality up to 40% and even though the studies for children are limited there is an overwhelming consensus that early recognition and early intervention of care in the septic shock pediatric patient improves outcomes [37-41].
Conclusion
Shock reversal from early aggressive fluid administration and vasoactive agent support for pediatric patients can substantially decrease mortality; for each unrecognized and untreated hour of shock, the mortality rate is estimated to increase twofold [5]. In all studies regarding pediatric patients who present to the emergency department in septic shock, whether it be a pediatric or non-pediatric emergency department, early recognition and early goal directed intervention would decrease mortality and insure shock reversal [42-44]. It is the belief of this author that the development of written protocols and education of teams could add to the achievement of the goal that every child with severe sepsis/septic shock should be treated according to the latest evidence to heighten their chances of survival.
The early recognition and initial management of severe sepsis and septic shock in children during the first hour of resuscitation is crucial. Rapid recognition of hemodynamic abnormalities and early suspicion of infection are essential to achieve favorable outcomes [38]. Pediatric shock is treatable if recognized early. Successful management requires early aggressive fluid resuscitation followed by treatment individualization based on bedside assessment. Support should escalate rapidly following American College of Critical Care task force guidelines. Life-saving interventions do not require state-of-the-art medical technology, can be instituted by primary care physicians, and lead to dramatic improvement in survival [37,45]. Just as there are "golden hours" in the treatment of stroke, acute myocardial infarction, and trauma, early recognition of septic shock and formulation of a goal-directed therapeutic plan are critical [6,46].
6737
References
- Odetola FO,Gebremariam A, Freed GL (2007) Patient and hospital correlates of clinical outcomes and resource utilization in severe pediatric sepsis. Pediatrics 119: 487-494.
- Dellinger P R, SchorrC, Trzeciak S (2011)Multicenter clinical trials in sepsis: Understandingthe bigpicture and buildingasuccessful operation atyour hospital. Critical CareClinics 25:215-225.
- Inwald DP,Tasker RC, Peters MJ, Nadel S; Paediatric Intensive Care Society Study Group (PICS-SG) (2009) Emergency management of children with severe sepsis in the United Kingdom: the results of the Paediatric Intensive Care Society sepsis audit. Arch Dis Child 94: 348-353.
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, et al. (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41: 580-637.
- Han YY,Carcillo JA, Dragotta MA, Bills DM, Watson RS, et al. (2003) Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics 112: 793-799.
- Oliveira CF, NogueiradeSaFR, OliveiraDS, Gottschald AF, MouraJD, et al. (2008) Time and fluid sensitive resuscitation forhemodynamicsupport of children in septicshock: barriers to the implementation of theAmerican Collegeof Critical CareMedicine/Pediatric Advanced LifeSupport Guidelines in apediatric intensivecareunitin a developingworld.Pediatric EmergencyCare 24: 810-815.
- Watson R S, Linde-Zwirble W T, Lidicker J, Carcillo J A, Angus D C (2002) The increasing burden of severe sepsis in U.S. children. Critical Care Medicine, 29(46).
- Vanzant A M, Schmelzer M (2011) Detectingand treatingsepsisin the emergency department. Journal of EmergencyNursing 37: 47-54.
- Kissoon N, Orr RA, Carcillo JA (2010) Updated American College of Critical Care Medicine--pediatric advanced life support guidelines for management of pediatric and neonatal septic shock: relevance to the emergency care clinician. PediatrEmerg Care 26: 867-869.
- Goldstein B,Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. PediatrCrit Care Med 6: 2-8.
- Fisher JD, Nelson DG, Beyersdorf H, Satkowiak LJ (2010) Clinical spectrum of shock in the pediatric emergency department. PediatrEmerg Care 26: 622-625.
- Knowles MS (1984) Andragogy in action. Jossey-Bass, San Francisco, USA.
- Knowles MS (1981) The adult learner: A neglected species. (3rd Edn). Gulf Publishing Company, USA.
- Rogers E M (2003) Diffusion of innovations (5th Edn.). Free Press, USA.
- Schorr C (2011) Performance improvement in the management of sepsis. Critical CareClinics 25:203-213.
- Kutko MC,Calarco MP, Flaherty MB, Helmrich RF, Ushay HM, et al. (2003) Mortality rates in pediatric septic shock with and without multiple organ system failure. PediatrCrit Care Med 4: 333-337.
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, et al. (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345: 1368-1377.
- Carcillo JA, Davis AL, Zaritsky A (1991) Role of early fluid resuscitation in pediatric septic shock. JAMA 266: 1242-1245.
- Santhanam I, Sangareddi S, Venkataraman S, Kissoon N, Thiruvengadamudayan V, et al. (2008) A prospective randomized controlled study of two fluid regimens in the initial management of septic shock in the emergency department. Pediatric Emergency Care 24:647–655.
- Kanter RK, Zimmerman JJ, Strauss RH, Stoeckel KA (1986) Pediatric emergency intravenous access. Evaluation of a protocol. Am J Dis Child 140: 132-134.
- Chameides L, Samson R A, Schexnayder S M, Hazinski M (2011)Pediatric advanced life support. American Heart Association
- Siddiqui S,Razzak J (2010) Early versus late pre-intensive care unit admission broad spectrum antibiotics for severe sepsis in adults. Cochrane Database Syst Rev: CD007081.
- Kleinman M E, de Caen A R, Chameides L, Berg R A, Berg, M D, et al. (2010) Pediatric basic and advanced life support: 2010 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Pediatrics 126:1261.
- Han Y, Carcillo J A, Dragotta M (2000) Early reversal of shock is associated with improved outcome during inter-facility transport of pediatric septic shock. Pediatric Research 47:108A.
- Cruz AT, Williams EA, Graf JM, Perry AM, Harbin DE, et al. (2012) Test characteristics of an automated age- and temperature-adjusted tachycardia alert in pediatric septic shock. PediatrEmerg Care 28: 889-894.
- Carcillo JA, Fields AI; American College of Critical Care Medicine Task Force Committee Members (2002) Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med 30: 1365-1378.
- American Academy of Pediatrics (AAP) (2009) Committee on pediatric emergency medicine, American College of Emergency Physicians pediatric committee, Emergency Nurses Association pediatric committee: Guidelines for care of children in the emergency department. Pediatrics 124:1233–1243.
- Institute of Medicine (2006). Committee of the future of emergency care in the US health system. Emergency care for children: Growing pains. National Academies Press, Washington, USA.
- Judge TA, Piccolo RF (2004) Transformational and transactional leadership: a meta-analytic test of their relative validity. J ApplPsychol 89: 755-768.
- Bass B, Riggio R (2006) Transformational Leadership. (2nd Edn). Erlbaum.
- Worster A, Haines T (2004) Advanced statistics: understanding medical record review (MRR) studies. AcadEmerg Med 11: 187-192.
- Lindhjem H, Navrud S (2011) Are Internet surveys an alternative to face-to-face interviews in contingent valuation? Ecological Economics 70:1628-1637.
- Windle J, Rolfe J (2011) Comparing responses from internet and paper-based collection methods in more complex stated preference environmental valuation surveys. Economic Analysis and Policy 41:83-97.
- Jones AE, Puskarich MA (2009) Is lactate the "Holy Grail" of biomarkers for sepsis prognosis? Crit Care Med 37: 1812-1813.
- Cruz AT, Perry AM, Williams EA, Graf JM, Wuestner ER, et al. (2011) Implementation of goal-directed therapy for children with suspected sepsis in the emergency department. Pediatrics 127: e758-766.
- Weiss S L, Pomerantz W J (2012) Septic shock: Rapid recognition and initial resuscitation in children. Pediatric Critical Care Medicine 13:219.
- Barclay L (2011) ED septic shock protocol and guideline may improve care.
- Bilkovski RN, Rivers EP, Horst HM (2004) Targeted resuscitation strategies after injury. CurrOpinCrit Care 10: 529-538.
- Brierley J, Carcillo J A, Choong K, Cornell T, Decaen A, et al. (2009) Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Critical Care Medicine, 37:666-688.
- Burt CW, Middleton KR (2007) Factors associated with ability to treat pediatric emergencies in US hospitals. PediatrEmerg Care 23: 681-689.
- Carcillo JA,Kuch BA, Han YY, Day S, Greenwald BM, et al. (2009) Mortality and functional morbidity after use of PALS/APLS by community physicians. Pediatrics 124: 500-508.
- Gaieski DF,Mikkelsen ME, Band RA, Pines JM, Massone R, et al. (2010) Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med 38: 1045-1053.
- Maar SP (2004) Emergency care in pediatric septic shock. Pediatric Emergency Care 20:617-624.