Keywords
Mental health care, Psychiatrists, Health care.
Introduction
Some well-known roles of psychiatrists include those of prescribing medication, managing crises, leading treatment teams, training and supervising non-specialist health workers, and monitoring and assessing mental healthcare programs. Some say that there are as many ways to practice psychiatry as there are psychiatrists.
Faced with this heterogeneity, a more immediate question might arise: What does it mean to be a psychiatrist today? Moreover, what is a psychiatrist? How do we address plurality if psychiatry is meant to be a scientific discipline and a reproducible practice? What do we do about the growing, global mental healthcare needs?
Throughout its brief history, psychiatry has been influenced and defined by numerous streams of thought that are sometimes complementary and sometimes contradictory to each other. Our present time is no exception to this rule. The question looms whether psychiatry, drawn by medicine and also by the humanities, should belong under the field of neurosciences or the social sciences? In either case, how does psychiatry address the needs and life conditions of its patients?
Through interviews of psychiatrists and users, a few tracks of reflection have emerged. As expected, psychiatry seems deeply embedded in medicine. If the biological model has been able to improve some parts of psychiatric practice and its users’ quality of life, many psychiatrists identify limits to this model and are frustrated by its tendency to marginalize their role into one of medication management. The degrading conditions of clients’ lives, the increase of health inequities, and the decrease in psychiatrists’ ability to find “out of the box” solutions are fundamentally ignored in the face of a theoretical premise. This paper attempts to address this issue from a historical, sociological, and global perspective.
Methods
The study was approved by the institutional review board for human research at Yale University. This research employs mixed methods. A literature search drew from a variety of areas— psychiatry, medicine, anthropology. sociology, economics, public health, global health, law, and philosophy— and different periods of time due to the authors’ interest in gaining a cross-disciplinary perspective. Moreover, over 10 months, the principal author conducted participatory observation of weekly clinical meetings of psychiatrists at a community mental health center; monthly scholarly meetings that included psychiatrists, psychologists, and philosophers; and Assertive Community Treatment (ACT) team sessions in New York, Philadelphia, and New Haven. While working in the community center, the first author also conducted structured, quasi-qualitative taped and transcribed interviews of 12 psychiatrists typically lasting around one hour each. The subjects for the study were recruited by “snowball sampling” from the community center and its inpatient unit [1]. The first author also had discussions with peer mentors and informal discussions with different professionals—sociologists, anthropologists, psychologists, researchers in public health, and writers—concerned with mental health issues. The results are compiled here in the form of quotes to provide an example of the wide range of perspectives of psychiatry is and where it may be going.
Results
Psychiatry: a branch of medicine
Psychiatry is a relatively new field within medicine. In the past, one might have depended on a priest or other authority for matters that family members and other immediate social supports could not handle. However, with the advent of modernity, many such social supports have disappeared, and the role of psychiatry is to step in where society is unable to meet those needs and to try to help individuals cope with symptoms and adapt to their environment. Nevertheless, psychiatry, which lacks consistent internal markers of disease, seems to be for some a branch of medicine that is relatively underdeveloped. One psychiatrist stated: “Psychiatry is about where internal medicine was 100 years ago in the sense that we have our observations, we put people together based on our observations, which are all macroscopic: you are hearing voices, or you are not.” Over the past century, different models and metaphors of psychiatric illness have been tried, come into and gone out of fashion, and have been debunked, only to be revisited. Compared to other disciplines of medicine, it is impressive that the landscape of psychiatry can appear to remain so uncharted: No one knows “what causes what.” What difference do psychiatric treatments make? Do they mask symptoms? Do they make them go away? Do they improve the course of the illness? Do they worsen it? That a branch of medicine can still ask these questions suggests that it is still in its formative stages.
Psychiatric research over the past forty years has failed to produce a single biological test that one can use in the clinic. There may someday be tests to diagnose depression or anxiety or schizophrenia, but they are not available today. In their absence, psychiatry is caught up in the politics of a classificatory game that most of medicine went through in the nineteenth century. Such a state of things might be cause for despair over psychiatry’s ability to escape its present stagnation. The feeling among American psychiatrists is that the paradigms and major assumptions and ways of producing knowledge in psychiatry need to be re-thought. “Psychiatry is developing in great ways, but I have no idea where it is going,” said one psychiatrist. Contemporary psychiatry may have more to gain by strengthening its connections with public health and the social sciences than by focusing on ever more subtle uses of costly psychotropics. The current weakness of the field is also its strength: the more psychiatry is the branch of medicine that is nebulously at the interface between individuals and society, the more integrative it can be in encompassing the full range of human experience, from the biological to the sociological. As one psychiatrist noticed: “We have our illnesses, we have our syndromes, we have obligations from the state that few other groups of physicians have, and we are forced to put those together and balance the needs of society and of the people.” There is a “natural link” between psychiatry and social sciences that we will develop throughout the article.
How can psychiatry and medicine help each other?
For psychiatrists, having a medical background is very helpful for thinking about the impact of treatments (medication and psychotherapy) and the biological causes of psychological manifestations, for the mind and body are one. It also helps in thinking about the multifaceted human being before the physician, as biology is one factor among many that contribute to and partly constitute one’s experience of life. Psychiatrists are physicians. This fact can contribute to a holistic practice of mental healthcare. . Few other professions have this opportunity. . In addition, an understanding of biological systems can help psychiatrists to destigmatize mental illnesses, considering them as illnesses “like any other” and not a moral failing. If there are advantages to a “biomedical” perspective for psychiatry, can the fact of being informed by a “psychological” perspective help the other disciplines of medicine?
In 1958, Hollingshead and Redlich [2], in a multi-year study analyzing the link between social class and the occurrence of mental illness in the New Haven, Connecticut, community, emphasized the importance of locating the person in their specific context, and the impact of all kinds of factors, including background, religion, area of residence, culture, and relationships within the community. Psychiatry involves the full spectrum of human experience. It involves all of the things that the rest of medicine involves and goes beyond it. Of course the rest of medicine is not entirely focused on individuals’ physical functioning, as many social and cultural components also play a role in how a disease manifests. One psychiatrist said: “The responsibility of psychiatrists is not only to know all of the basics of medicine but also to be as knowledgeable as possible about human culture and societal experiences”. Psychiatrists should attend to these domains as more than just “external stressors”. They should see them in a multidimensional context, interacting intricately and elaborately with the individual. Context and individuals are not linked linearly but dialectically and interactively [3]. If psychiatry comprehends the social environment in this way, it could guide other disciplines of medicine in that direction, as even biomedicine recognizes that it, too, cannot ignore the “biopsycho- social” origins of disease. Eventually, psychiatry through its expertise in the patient-doctor interaction and with its teamoriented approach can be a useful model for the rest of medicine.
Mental Illness
During a lecture that the first author attended during the course of the study reported here, a psychiatrist involved in the construction of the Diagnostic and Statistical Manual, Third Edition (DSM-III) said:
People are very critical of DSM-III, and they have good reasons, but it’s important to compare with before DSM: the psychiatric world was really weird. It was a mess, with people using a common language but meant different things.
Has the situation changed in the last thirty years? Psychiatrists are more or less consistent in the use of language regarding mental health and illness and sophisticated in the fine distinctions they make among themselves, but the fundamental definition of mental illness remains a mystery. Asked the question—a common one in court testimony—“What is mental illness?” their responses vary widely and often reflect a lack of knowledge. One psychiatrist honestly stated:
Mental Illness is something that I try to understand…. I don’t know any more what illness is, and especially mental illness…. I don’t think we do know what mental illness means…. What we call mental illness is an exaggeration of the normal, perhaps deformed by social factors, and to what extent is it really an illness? We do not know.
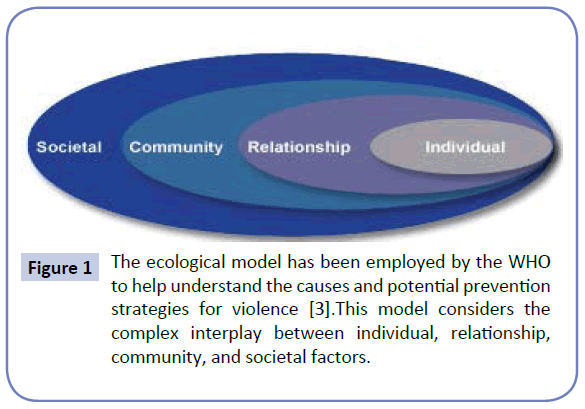
Other psychiatrists agreed on the “brain-based” aspect of the disorder but without any idea of the pathophysiology of that disorder. They seem to have the feeling that something difficult to delineate happens in the brain, but they do not know what thing or phenomenon is. If mental illnesses are brain-based, what is the difference between neurological and mental diseases? One psychiatrist answered: “Neurologists have evidence that is more convincing in pathology. They usually find anatomical correlation, and mental illnesses are defined by exclusion: if you don’t understand what’s going on, it’s a mental illness”. A current idea is that mental illness is an illness “like any other.” But what is an illness like any other? This assumption can be true in the sense that the concept of mental disorder, like many other concepts in medicine, lacks a consistent operational definition that covers all situations. Perhaps the lack of knowledge and consensus is more notable for mental illness than for ‘physical illness,’ as noted previously, since psychiatry does not have internal markers of illness. Psychiatrists tend to focus more on the consequences of illness—the debilitation of functioning it causes, the socialenvironmental difficulties and maladaptive behaviors associated with it for individuals, the difficulties of communication and daily activities that serve as signs of it—than on the illness itself: …. Mental illnesses are defined in terms of the level of functioning more than a particular diagnosis. The bio-psycho-social model of mental illnesses has helped to bring together the relevant areas for most psychiatrists, but a unified perspective that illuminates how the three clusters are linked is lacking. A better approach might be the “ecological” one that the World Health Organization (WHO) advocates for violence prevention (Figure 1).
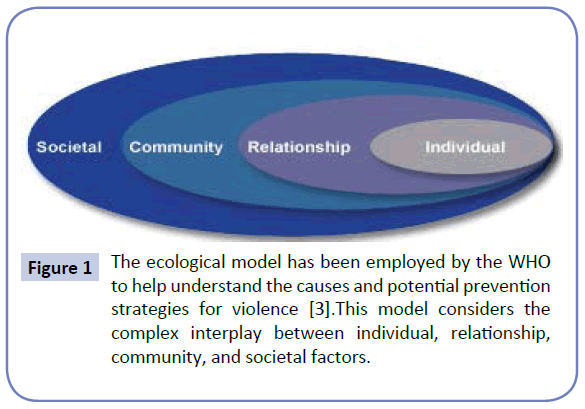
Figure 1: The ecological model has been employed by the WHO to help understand the causes and potential prevention strategies for violence [3].This model considers the complex interplay between individual, relationship, community, and societal factors.
In the 1980’s, Langsley [4,5] conducted two quantitative studies and defined a psychiatrist as “a clinician whose main skills are in evaluating and treating psychiatric disorders”. Regarding this lack of knowledge and understanding of mental illnesses and the crisis that clients and the health system are undergoing, it seems necessary to go beyond a simple definition of a psychiatrist as someone with skills for treating mental illness. The current and urgent question arising in our research is, rather: How and with which skills can psychiatrists improve symptoms, the life context that contributes to patients’ symptoms, and the mental health delivery system that often misses people’s needs?
Discussion
While some field experiences and research has demonstrated the positive impact of peer workers and community care [6,7] and while the recovery model can offer a fresh perspective to psychiatry, psychiatrists still resist such practices and the recovery model and are slow to adjust their practice to it.
To understand this resistance and why psychiatrists and doctors in general are becoming fearful of any kind of change, it might be useful to examine some trends in medicine over the past twenty-five years. First, physicians in general have lost much of their previous leadership roles to administrators, thus arguably reducing their roles to those of “workers” rather than leaders in mental healthcare. Second, medicine itself has become an industry. Often psychiatrists have to see thirty patients in one day, allotting ten minutes for each, and do their write-ups and communication with other providers in their free time. Care delivery often is not based on the right treatment but the most cost-effective one. Psychiatry is not the only specialty to be affected by such changes: U.S. medicine , since its industrialization, has dropped from its leading position to number 37 in the WHO’s ranking of global health systems [8]. One psychiatrist lamented:
Instead of the team working together with peer workers, social workers, nurses, psychologists, and psychiatrists, it became: the psychiatrist is expensive, so just cut out this portion, and the rest will be handled by this person. And instead of a team handling the situations, the team became: you take this portion, you take that, and you are supposed to communicate during your free time, and of course you don’t have free time.
Third, as a consequence of the first two developments, psychiatrists have largely been marginalized into a medication management role.
The recovery movement may have room for psychiatry, if psychiatry can become clear about and endorse its potential contribution to it. Recovery-oriented approaches and interventions appeared in part as a response to the fiasco of the “deinstitutionalization movement, but has become its own distinct movement. The recovery movement also has roots in the work of “psychiatric survivors,” inspired in turn by feminist, anti-racist, and AIDS awareness movements. With these roots and influences, recovery is probably more capable of supporting sustainable and positive change in psychiatry than current biologically and medication-based approaches, as the American Psychiatric Association, the Royal College of Psychiatrists, and a growing number of psychiatric bodies across the world are beginning to recognize [9].
Yet what is, or what can be, the function of psychiatrists in this movement? Recovery, in its core principles, is not an “antipsychiatry” movement. Psychiatrists must learn not to be the center of mental healthcare but one of multiple actors, interacting in a horizontal rather than vertical way. Effecting such a change is complicated by the fact that the culture of medicine is based on a pyramidal distribution of power, with the Medical Doctor at the top of the pyramid. Some publications on medical education about “the hidden education” suggest that the phenomenon persists, despite the report of students and trainees of the hierarchical and competitive atmosphere as a humiliating experience [10-12]. This organization has a strong impact not only during education but also in practice, in research, and in health policy.
Sharing power does not mean losing power. In fact, it may amount to an effective enhancement for psychiatrists, who may, however, need to welcome the effective power of other medical actors.. One way that psychiatrists may be able to enhance their roles is to use their knowledge and training to affect positive change in health care policies. Psychiatrists’ intimate encounter with individuals might be applied to a larger scale, through advocating for reform in mental health delivery and policies that would, for example, help prevent mental illness. One psychiatrist noted: “I feel I am using all the skills of being a psychiatrist when I interpret the behaviors of individuals and how they manifest at larger scale, be it at the level of society or even nations.” To most effectively act in the manner that this psychiatrist emphasizes, however, psychiatry must shift its gaze to include an understanding of social and healthcare systems. . Users of such systems are caught up in the complicated and illogical nature of these systems and their resistance to change. Psychiatrists can extend a hand to clients to help navigate through those experiences and to give them understanding. While psychiatrists’ role as advocates may pale in comparison to others actors such as peers, social workers, and, potentially, healthcare administrators, becoming better advocates for their patients may have a healing effect on patients and on the discipline of psychiatry. This, we argue, is a minimum standard of advocacy for the practice of psychiatry:
If you see the same thing happening to clients over and over, something needs to be changed” says one psychiatrist. “How do you diagnose a problem within a hospital or a social system? Again, how do you measure the problem, put together a change cycle, and institutionalize that change?”
Psychiatrists must observe and understand what has happened to their clients in their individual contexts) and be able to evaluate their success in implementing and improving their interventions. In the first case, we argue for a mobilized psychiatry, a physical mobility whereby psychiatrists go out to and work in their local communities while also adopting creative training methods such as role play and learning from clients and peer mentors. In the second case, we underline the importance of social sciences for the psychiatrists in the evaluation and contextualization of their interventions.
Conclusion: Psychiatry and Global Mental Health, a Great Opportunity
According to the perspective of those interviewed for this study, there is a crisis happening within psychiatry, a disconnect between what psychiatric clients desire and what psychiatrists are delivering. In 1865, Rudolf Virchow [13] defined the physician as a “natural attorney of the poor”. In 2015, perhaps more than is the case for other physicians, psychiatrists, especially those working in the domain of public services, have the opportunity and responsibility to advocate for their patients, who typically find themselves at the bottom of the socioeconomic ladder, struggling to survive socially and economically as well as mentally and emotionally. . Too often, people with mental illness navigate between prisons, hospitals, shelters, and the streets, a trajectory that has come to be called “the institutional circuit” [14]. This circuit seems to work autonomously, permitting society to keep those “undesirables” away, or as Hopper and Baumohl [15] argue, in abeyance for a society that lacks social roles in which to put them.
Psychiatry is undergoing a dual crisis: an intrinsic crisis of its theoretical model, and a practical crisis in its diminishing ability to provide for a vulnerable population at a time of increasing economic difficulty. “Crisis” (from the Greek “krisis,” for “crossing”), etymologically defined, is better considered not as a negative consequence of a problem but rather as a moment of system imbalance, the inevitability of change, and the opportunity for improvement [16]. Times of crisis can be times of opportunity. The current dual crisis of psychiatry represents a favorable moment for rethinking and redefining the discipline. The limits of the medical model and the potentialities of the social sciences to shed new light on mental illnesses and to respond to them efficiently represent an opportunity for improvement and the renewed relevance of contribution of psychiatry to human prospering.
Eventually, one way for psychiatrists to become the best advocates for their patients is to understand their experiences as relative to a particular context and to see their networks as an inter-subjective field of socioeconomic and cultural relations. Additionally, the psychiatrist must be immersed in the situation at the same time as looking at it from a distance to assess it and to evaluate and monitor their own actions -and hence become an “applied anthropologist.” The strong links between anthropology and psychiatry are then obvious. Kleinman [17] shows that psychiatry needs anthropology for three reasons: first, “to make sense of cross-cultural and interethnic differences in the meanings and experiences of illnesses”; secondly, to show that psychiatric knowledge, institutions, and practices can be analyzed from a cultural perspective; and finally to provide relevant skills for a global perspective in mental health.
In the same way that Kleinman thinks that psychiatry and anthropology are useful to each other, psychiatry and global mental health can interact positively. We should not lose sight of the fact that these complexities are the result of an expanded opportunity for psychiatry to make a difference at a global level, along with a greater recognized need, and that there is much we can do to reshape our profession and reputation as psychiatrists if we rise to the challenge. Within Western countries, the growing representation of asylum seekers and refugees [18], the new issues that they bring [19] and the diverse cultural backgrounds that present to clinics illustrate the widening expanse of medicine’s involvement. Psychiatry is well-positioned to inform the rest of medicine (as well as law and other social fields), all through the knowledge and sensitivity that are gained from learning to become a better advocate for the client. To do so, we must step up our own awareness and training to enlarge our vision.
Acknowledgments
The authors would like to gratefully acknowledge Larry Davidson and the Program for Recovery and Community Health (PRCH) for their support of this research, and Grace Lee for her valuable conceptual contributions to this article.
7823
References
- Biernacki P, Waldorf D (1981) Snowball sampling: Problems and techniques of chain referral sampling. Sociological Methods & Research 10: 141-163.
- Hollingshead AB, Redlich FC (2007) Social class and mental illness: a community study. 1958. American journal of public health. 97: 1756-1757.
- Krug EG, Mercy JA, Dahlberg LL, Zwi AB (2002) World report on violence and health. Biomedica 22 Suppl 2: 327-336.
- Langsley DG, Hollender MH (1982) The definition of a psychiatrist. Am J Psychiatry 139: 81-85.
- Langsley DG, Yager J (1988) The Definition of a Psychiatrist - 8 Years Later. Am J Psychiat 145: 469-475.
- Rowe M, Bellamy C, Baranoski M, Wieland M, Connell MJO, et al. (2007) A peer-support, group intervention to reduce substance use and criminality among persons with severe mental illness. PsychiatServ 58: 955-961.
- Davidson L, Chinman M, Kloos B, Weingarten R, Stayner D, et al. (1999) Peer support among individuals with severe mental illness: A review of the evidence. Clinical Psychology: Science and Practice 6(2): 165-187.
- Murray CJ, Frenk J (2010) Ranking 37th--measuring the performance of the U.S. health care system. N Engl J Med 362: 98-99.
- Davidson L, Rakfeldt J, Strauss JS (2010) The roots of the recovery movement in psychiatry : lessons learned. Chicester, UK ; Hoboken, NJ: Wiley-Blackwell.
- Marinker M (1997) Myth, paradox and the hidden curriculum. Med Educ 31: 293-298.
- Seabrook MA (2003) Medical teachers' concerns about the clinical teaching context. Med Educ 37: 213-222.
- Lempp H, Seale C (2004) The hidden curriculum in undergraduate medical education: qualitative study of medical students' perceptions of teaching. Brit Med J 329: 770-773.
- Hopper K, Jost J, Hay T, Welber S, Haugland G (1997) Homelessness, severe mental illness, and the institutional circuit. PsychiatrServ 48: 659-665.
- Hopper K, Baumohl J (1994) Held in abeyance: Rethinking homelessness and advocacy. American Behavioral Scientist.
- Kleinman A (2001) Why psychiatry and cultural anthropology still need each other. Psychiatry 64: 14-16.
- Zonana H (2010) Commentary: the role of forensic psychiatry in the asylum process. J Am Acad Psychiatry Law 38: 499-501.
- Kagee A, Naidoo AV (2004) Reconceptualizing the sequelae of political torture: limitations of a psychiatric paradigm. Transcult Psychiatry 41: 46-61.