Keywords
Infertility, anxiety, depression, marital stress, communication, social support.
Introduction
Infertility, the failure for a woman to become pregnant after one year of regular sexual relationships without contraceptives, is perceived as a problem across virtually all cultures and societies.
Clinicians and researchers consistently report that infertile women view infertility and its treatment as extremely stressful [1,2,3,4]. Individual differences in psychological stress suggest that various psychological processes mediate or moderate the relationship between stressors and the psychological reaction to a chronic disease [5]. It is therefore, increasingly important to understand both the magnitude of the stress and personal resources of infertile women, as they try to adapt to the problems of infertility and its treatment. A range of psychosocial variables may influence infertile women’s stress during infertility treatment [6]. Variables such as satisfaction with marital relationship, satisfaction with spousal communication and satisfaction with communication with other people may be considered determinants of emotional stress and may be also considered either as risk or as protective factors to explain individual differences in emotional stress to infertility.
Previous research has studied the impact of marital satisfaction and communication satisfaction on infertility related stress and psychological adjustment to infertility [6]. These studies have consistently reported a negative effect of sexual and marital dissatisfaction, poor marital communication regarding infertility problem and dissatisfaction with social support from friends and family on infertility related stress. Abbey and colleagues [7] were among the first who identified an association between social support and psychological stress in infertile individuals. They found that spouse interpersonal conflict related negatively to well being of infertile individuals and sexual dissatisfaction related significantly positively to fertility problem stress. In Canada, the Fertility Problem Inventory assessment indicated that sexual and relationship concerns predicted depression in infertile patients [8]. Mindes and colleagues [9] found that women who reported more infertility-specific unsupportive social interactions had higher rates of depressive symptoms and overall psychological stress.
Matsubayashi et al., [10] revealed that anxiety and depression of infertile women were significantly associated with lack of husband’s support. Verhaak and colleagues examined the impact of social support on stress immediately after a failed infertility treatment [11] and six months after the first failed fertility treatment [12]. They found that increased levels of anxiety were significantly and positively related to marital dissatisfaction and that increased levels of depression were significantly and positively related to perceived dissatisfaction with social support.
Lechner and colleagues [13] reported that dissatisfaction with perceived social support was statistically and positively associated with higher levels of stress outcomes (health complains, anxiety, depression, grief) after failed fertility treatments. In line with previous studies, a recent study by Slade and colleagues [14] reported that perceived availability of social support and partner relationship satisfaction were negatively related to anxiety, depression and infertility related distress. A recent study by Gourounti and colleagues [15] observed that Greek infertile women who reported greater spousal concern had higher levels of anxiety, depression and emotional distress.
The aims of this cross-sectional study were to examine a) the association between marital satisfaction and distress, b) the association between communication with partner and distress, and finally c) the association between communication with other people and distress. Based on previous research, we hypothesized that women with high marital satisfaction and good communication with partner and other people would experience lower level of distress.
Methodology
Study Setting
The study was conducted in one of the largest public infertility clinics in Greece to achieve a large and representative database. Infertile women were residents of the greater Athens area.
Study design and data collection
This study was a cross sectional survey which involved collecting information from the participants by using three questionnaires. Data were collected over an eleven-month period, from November 2005 to September 2006. In detail, women received a letter in an envelope, just before undergoing their first treatment attempt in that clinic. Aim and expected benefits of the study were explained in the letter, and a member of the research team approached each woman who expressed interest in taking part, in order to provide further information for the study. Participants were given the opportunity to ask for clarification if it was necessary.
Explanations were given, when necessary, to the participants by the researcher and finally the questionnaires were returned to the researcher who was not an employee of the fertility clinic.
Participants
The population from which the participants were drawn was infertile women undergoing fertility treatment. According to the inclusion criteria the women chosen: a) were able to read and write in Greek language in order to have the ability to complete the questionnaires, b) have unsuccessfully tried to conceive a child with natural methods for more than one year, and c) have had an infertility diagnosis and were not waiting for a new one. Researchers approached 452 women in the infertility clinic to ask them to participate in the study, 410 women (90.7%) agreed to take part and finally 404 women (89.3%) returned completed questionnaires.
Measures
In order to quantitatively assess the psychological disturbances, validated and standardised psychometric tools were used. The research instruments were three self-administrated questionnaires. The State-Trait Anxiety Inventory questionnaire (STAI) by Spielberger [16] and Centre for Epidemiologic Studies- Depression Scale by Radloff [17] were employed to assess the psychological distress. The COMPI questionnaire [18] was used to assess the satisfaction from the marital relationship and the extend of the communication with the partner and the other people.
STAI questionnaire was used in order to measure anxiety in women undergoing fertility treatment. STAI assessed both state and trait anxiety. State anxiety is defined as an unpleasant emotional condition that emerges in case of threatening demands or dangers.
Therefore, it should be low in non stressful moments and high if circumstances perceive to be threatening or dangerous. Trait anxiety, on the other hand, reflects the stable tendency of a person to respond with state anxiety in the anticipation of threatening situations. Trait anxiety refers to chronic anxiety and describes the tendency to perceive situations as threatening, and hence to experience state anxiety in stressful situations. The STAI state scale consists of 20 items that ask people to describe how they feel at a particular moment in time rated on a 4- point scale ranging from not at all to very much so.
The STAI trait scale consists of 20 statements describing how people generally feel (e.g., confident) rated on a 4-point frequency scale ranging from almost never to almost always. Total scores for state and trait anxiety ranging from 20 to 80 [19], whereas the published normative score by non-pregnant women for state anxiety is 35.2 (SD 10.6), for trait anxiety is 34.8 (SD 9.2) and by people with diagnosed anxiety disorder is ranging between 47 and 61 [19]. The STAI has been adapted to Greek and has been found to have satisfactory psychometric properties (state α = 0.92, trait α= 0.89) and construct validity [20].
The Center for Epidemiologic Studies- Depression Scale (CES-D) was used to assess depression symptoms of the study population. CES-D is a self-reporting 20-item scale that covers affective, psychological, and somatic symptoms occurring during the past week. Responses to item statements are graded from 0 (rarely or none of the time) to 3 (most or all of the time). Scores for each item in the CES-D Scale are summed to obtain an overall score. The overall score ranges from 0 to 60, the higher the score the more frequent the depressive symptoms. Several cut-off points that are indicative of depression have been suggested in previous studies [19]. In a previous Greek study it has been found that sensitivity and specificity of CES-D exceed 90% at a cut-off point of 23 [21]. In this study the cut-off score of 23, as suggested by Fountoulakis and colleagues [21], was adopted not only because sensitivity and specificity of CES-D exceed 90% at the score of 23 but also because the demographic characteristics of sample in study by Fountoulakis et al., [21] are similar to the demographic characteristics of our sample.
The COMPI questionnaire has been adapted from a previous Danish study [18,22]. A total number of 14 items from COMPI questionnaire were used to assess sociodemograpfic profile of participants. Sociodemographic background information included variables concerning age, years of marriage, occupation and social position and educational level. A total number of 6 items from COMPI questionnaire were used to measure marital stress and marital benefit. Infertility related stress on the marital domain (subscale of four items) assessed the stress that infertility had produced on the marital and sexual relations. Marital benefit was measured by two items: our childlessness has (i) brought us together; (ii) strengthen our relationship. The response categories for the two items of the marital stress subscale was a four-point Likert response scale from (1) none at all to (4) a great deal. The response categories for the remaining two items of marital stress subscale and the two items of the marital benefit subscale were a five-point Likert response scale from (1) strongly disagrees to (5) strongly agree. The range differed according to the subscale: and marital stress (range 0-14), marital benefit (range 0-8). Total scores were calculated by summing the relevant items. Higher scores indicated higher marital stress and lower marital benefit. One item from COMPI questionnaire were used to measure communication with partner. Communication with partner was measured by one item (Do you find it difficult to talk with your partner about your fertility problem?). The response key was: 1) yes always, 2) yes sometimes, 3) no never; dichotomised into 1-2 versus 3. Six items from COMPI were used to measure infertility related communication strategy (e.g. communication regarding treatment, childlessness, emotions related to infertility) with other people.
The response key was: 1) not to other people, 2) only to close people, 3) to most people I know. The score ranged from 3 to 18 and higher score indicated increased communication with other people.
Reliability of the subscales of COMPI questionnaires was assessed by Cronbach’s alpha. In this study the alpha coefficient was 0.72 for the marital stress subscale, 0.92 for the marital benefit subscale and 0.93 for the subscale of the infertility-related communication with people.
Ethical considerations
Permission to complete this study was obtained from an Institutional Ethical Research Committee. Participants were assured of keeping their anonymity and their answers confidential, as well as about their right to refuse at any time to go on with the survey, in case they decided to do so. Participants were also assured that the collected data would be used only for the purpose of the study, and that their decision to withdraw or refusing to participate would not compromise the standard of the received care.
Statistical analysis
Descriptive and inferential statistics were conducted by using SPSS version 17.0. Data analyses involved descriptive statistics in order to calculate frequencies, means and standard deviations for each variable. Differences between women with high and low level of communication with their partner were examined by using independent samples t-test for continuous variables (e.g. state anxiety, depression, marital stress). Pearson correlation coefficients were used to determine the associations between the continuous variables. Chi- square analysis was used for categorical data. Analysis of variance (ANOVA) was carried out when comparing multiple groups of data. The level of statistical significance was set up at 0.05.
Results
The mean age of participants was 36.9 years (SD = 4.1 and range = 25-47) and the majority proved to have had medium level of education, to be working for a living and had no children. In detail, 38% percent of the women had tertiary education (high educational level), 48% of the women had secondary education (medium level) and 14% of the women had primary education (low level).
Besides this, most of the women (72%) were working and 28% of women were housewives. The mean duration of infertility was reported to be 2 years (SD 0.9 years) and the majority of the participants had previous experiences with infertility treatment, with 2.4 to be the mean number of previous treatments. Most women (86%) reported having no children and only 14% of women had at least one child. Diagnosis of infertility was recoded into female infertility, male infertility, mixed infertility (both female and male infertility) and idiopathic infertility (unknown aetiology). When asked to give the reason of infertility, participants categorized the cause of their infertility as follows: female aetiology (n = 102), male aetiology (n = 150), combined female and male aetiology (n = 90) and unknown aetiology (n = 62).
The mean score of participants’ state anxiety was 44.5 (SD 9.5) and the trait anxiety was 41.8 (SD 7.1). Both were found to be much higher than the published normative scores of state and trait anxiety which are 35.2 and 34.8 respectively [19]. Taking into consideration the ranges for low and high level in subscales of marital stress and marital benefit [23], the findings of this study showed low levels of experienced marital stress (range 0-14, mean 3.1, SD=3.0) and high levels of marital benefit (range= 0-8, mean 6.3, SD= 2.0) Furthermore, the majority of participants (84%) had a score of CES-D less than 23, which was indicative of non-depressive symptoms. The mean CES-D score was 13 (SD=9). The mean score of participants’ communication regarding infertility with people (range 3-18) was 9.4 (SD= 4.2). In addition, 83% of women did not find it difficult to communicate with their partner regarding infertility.
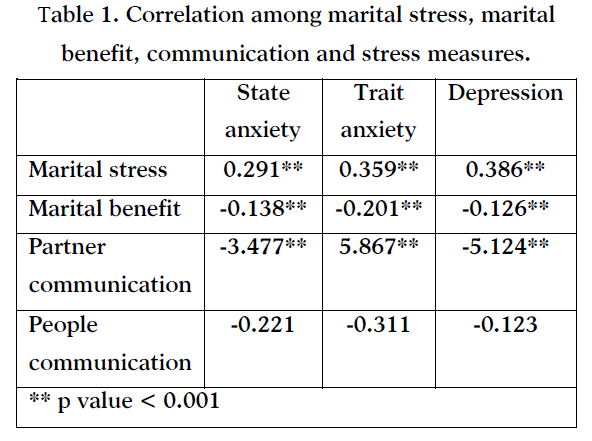
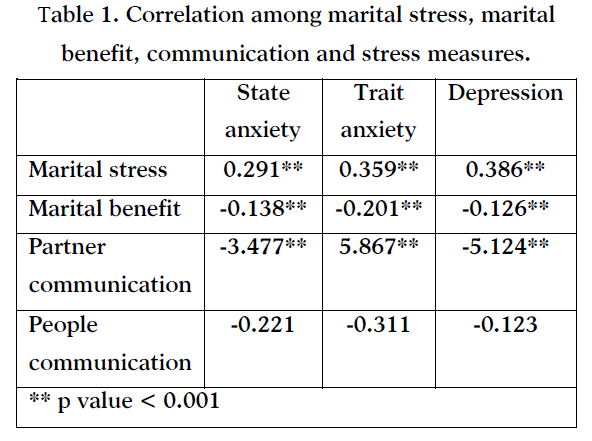
Correlation among marital stress, marital benefit, communication and stress measures were explored (see Table 1). Marital stress score was positively and statistically associated with state anxiety, trait anxiety and depression. Marital benefit was negatively and statistically associated with state anxiety, trait anxiety and depression. Communication with partner was negatively and statistically associated with state anxiety, trait anxiety, depression and marital stress. Communication with people was not statistically associated with anxiety, with depression, with marital stress, or with marital benefit. Communication with partner was positively and statistically associated with marital benefit (t= 2.606, p=0.010) and positively and statistically associated with marital stress (t=-4.541, p<0.001).
Discussion
Based on previous research, it was hypothesized that communication regarding infertility with other people would enhance psychological well being [7,11,12,14]. However, the data indicate that communication regarding infertility with other people is not a protective factor of anxiety and depression. This finding could be attributed to the fact that infertility can be kept secret from others [24]. Many women are unwilling to discuss their infertility problem with others out of embarrassment or discomfort about discussing sexual and fertility issues [24].
Many research studies conducted in different countries- industrialized and non-industrialized societies- suggest that infertile women have expressed feelings of stigmatization due to their fertility problems [25,26]. The ability to procreate is viewed as an essential part of individuals’ masculinity or feminity and therefore it is difficult to discuss infertility issues with others. In traditional settings and cultures, women have been shown to carry a greater burden of infertility, where there have been social pressures and expectations for women to procreate [26,27,28,29].
Taking into consideration the Greek tradition, motherhood makes a woman feel complete, demonstrating her ability to be a good mother and fulfilling her social role [30].
According to the study hypothesis women with high marital satisfaction and satisfying communication with their partner would experience low level of anxiety and depression. The study findings confirm the study hypothesis and suggest that concerns regarding the marital relationship and poor marital communication might be sources of anxiety and depression in infertile Greek women. This finding is consistent with findings of previous studies [7,8,10,14,15]. It seems that Greek infertile women may feel uncomfortable sharing information about their problem with others and tend to rely more on their partner for esteem, affirmation and tangible support. Therefore, marital dissatisfaction and poor marital communication can be a risk factor of increased anxiety and depression.
Professional psychological interventions with aim to relieve or diminish these conditions might have significant therapeutic benefits for women attending infertility clinics. The objectives of counselling to highly distressed patients are to enable the expression of their emotions, to identify the causes of distress and to provide interventions to minimize distress and help patients better manage distress [31]. Furthermore, the goal of psychological interventions should be the minimization of identified risk factors for infertility-related distress and the strengthening of protective factors. Clearly, professionals should assess the relationship quality of infertile couple whether or not both members of a couple seek counselling [32].
Identified areas of marital conflict and specifically those involving poor communication regarding infertility problem, infertility related decision-making difficulties and sexual difficulties can be addressed through couples’ therapy techniques [24]. Furthermore, in the face of unsupportive social interactions, professionals should identify ways to enhance social support.
Support groups may provide an opportunity for infertile couples to share concerns and information, to exchange experiences and allowing participants to benefit from the coping experiences of others [24].
Conclusion
Although, the role of social support as a buffer in the context of stressors other than infertility is well documented, infertile women undergoing fertility treatment may feel difficult in discussing infertility issues with others. The quality of the relationship and communication with the partner seems to impact on the emotional status of subfertile women.
The partner is potentially a crucial source of support for men and women who are reluctant to discuss their fertility difficulties with others. In the context of a stigmatizing stressor, the need for the partner for support and emotional well-being may well increase.
Strengths and Limitations
The study has several strengths: a) the questionnaires used in this study have been previously evaluated and have been proved to be reliable and valid measures, b) the response rate was satisfactory (89.3%) ensuring a large sample size (n=404) and c) all items of the questionnaires were answered by almost all the participants. These strengths ensure the reliability of study findings.
The study has a main limitation. The limitation of the current study is that the sample has been drawn only from one public infertility clinic and not from many clinics and this may decreases the generalizability of study findings.
Funding
The Project was co-funded by the European Union – European Social Fund and National Resources - (EPEAEK-II)
3322
References
- Dyer J., Abrahams N., Mokoena N., Lombard C., van der Spuy Z. Psychological distress among women suffering from couple infertility in South Africa: a quantitative assessment. Hum Reprod 2005; 20 (7): 1938-1943.
- Ozkan M and Baysal B. Emotional distress of infertile women in Turkey. Clinical and Expimental Obstetrics and Gynaecology 2006; 33 (1): 44-6
- Wang K, Li J, Zhang J, Zhang L, Yu J, Jiang P. Psychological characteristics and marital quality of infertile women registered for in vitro fertilization -intracytoplasmatic sperm injection in China. Fertil Steril 2007; 87 (4): 792-798
- Lykeridou K., Gourounti K., Deltsidou A., Loutradis D., Vaslamatzis G. The impact of infertility diagnosis on psychological status of women undergoing fertility treatment. J Reprod Infant Psy 2008; 27(3):223-237
- Lazarus RS and Folkman S. Stress, appraisal, and coping. Springer, New York, 1984
- Gourounti K., Anagnostopoulos F., Vaslamatzis G. Psychosocial predictors of infertility related stress: a review. Current Womens Health Reviews 2010 [BSP/CWHR/E-Pub/0017]
- Abbey A, Andrews F, Halman J. The importance of social relationships for infertile couples’ well being. In Stanton AL and Dunkel-Schetter C, eds. Infertility: Perspectives from stress and coping research. New York: Plenum Press 1991: 61-86
- Newton, C., Sherrard, W., Glavac, I. The Infertility Problem Inventory: measuring perceived infertility- related stress. Fertility and Sterilit 1999; 72: 54-62.
- Mindes E, Ingrama K, Kliewera W, James C. Longitudinal analyses of the relationship between unsupportive social interactions and psychological adjustment among women with fertility problems. Soc Sci. Med., 2003; 56: 2165-2180
- Matsabayashi H., Hosaka T., Izumi S., Suzuki T., Kondo A., Makino T. Increased depression and anxiety in infertile Japanese women resulting from lack of husbands support and feelings of stress. General Hospital Psychiatry 2004; 26: 398-404.
- Verhaak C, Smeenk JM, Evers A, Van Minnen A., Kremer J, Kraaimaat FW. Predicting emotional response to unsuccessful fertility treatment: a prospective study. J Behav Med, 2005a; 28(2): 181-190
- Verhaak CM, Smeenk JM, Van Minnen A, Kremer J, Kraaimaat FW. A Longitudinal, prospective study on emotional adjustment before, during and after consecutive fertility treatment cycles. Hum Reprod, 2005b; 8: 2253-2260.
- Lechner L, Bolman C, Van Dalen A. Definite involuntary childlessness: associations between coping, social support and psychological distress. Hum Reprod, 2007; 22 (1): 288-294.
- Slade P, ONeill C, Simpson A, Lashen H. The relationship between perceived stigma, disclosure patterns, support abd distress in new attendees at an infertility clinic. Hum Reprod, 2007; 22(8): 2309-2317.
- Gourounti K., Anagnostopoulos F., Vaslamatzis G. Psychometric properties and factor structure of the Fertility Problem Inventory (FPI) in a sample of infertile women undergoing fertility treatment. Midwifery 2010 (doi:10.1016/j.midw.2010.02.007 ).
- Spielberger C. Anxiety: Current trends in research. Academic Press, London, 1972.
- Radloff, L. The CES-D Scale: A self report depression scale for research in the general population. Applied Psychology Measure, 1977;1: 385-401.
- Schmidt L, Holstein B, Boivin J, Sångren H, Tjørnhøj-Thomsen T, Blaabjerg J, et al. Patients’ attitudes to medical and psychosocial aspects of care in fertility clinics: findings from the Copenhagen Multi-centre Psychosocial Infertility (COMPI) Research Programme. Hum Reprod 2003a; 18: 628-637.
- McDowell I (ed.) Measuring health. A guide to rating scales and questionnaires (3rd Edition), Oxford University Press, Oxford, 2006, pp. 319-327.
- Liakos A., Gianitsi S. The validity and reliability of the revised Greek anxiety scale by Spielberger. Engefalos 1984; 21: 71-76.
- Fountoulakis K., Iacovides A., Kleanthous S., Samolis S., Kaprinis S., Sitzoglou K., et al. 2001. Reliability, validity and psychometric properties of the Greek translation of the Center for Epidemiological Studies-Depression (CES-D) scale. BMC Psychiatry, 2001; 1: 3.
- Schmidt L. Infertility and assisted reproduction in Denmark. Epidemiology and psychosocial consequences. Danish Medical Bulletin 2006; 53: 390-417.
- Schmidt L, Christensen U., Holstein BE. The social epidemiology of coping with infertility. Human Reproduction 2005; 20: 1044-1052.
- Abbey A., Andrews F., Halman J.The importance of social relationships for infertile couples’ well being. In A.L. Stanton, & Dunkel-Schetter (Eds.), Infertility: Perspectives from stress and coping research (pp. 61-86). New York: Plenum Press, 1991.
- Kimani V., Olenja J. Infertility: cultural dimensions and impact on women in selected communities in Kenya. The African Anthropologist, 2001; 8(2): 200-214.
- Donkor E., Sandall J. The impact of perceived stigma and mediating social factors on infertility-related stress among women seeking infertility treatment in Southern Ghana. Social Sciences and Medicine 2007; 6: 1683-1694.
- Papreen N., Sharma A., Sabin K., Begum L., Ahsan S., Baqui A. Living with infertility: experiences among urban slum populations in Bangladesh. Reproductive Health Matters 2000; 8(15): 33-44.
- Okonofua F., Harris D., Odebiyi A., Kane T., Snow R. The social meaning of infertility in Southwest Nigeria. Health Transition Review, 1997; 7: 205-220.
- Benyamini Y. Gefen- Bardarian Y., Gozlan M., Tabiv G., Shiloh S., Kokia E. Coping specificity: the case of women coping with infertility treatments. Psychology and Health 2008; 23(2): 221-241.
- Petok, W. The psychology of gender specific infertility diagnoses. In: S. Covington & L. Burns (Eds), Infertility Counseling (2nd Edition) (pp 37-60). Cambridge University Press, 2006.
- Boivin, J., Appleton, T.C., Baetens, P., Baron J, Bitzer J, Corrigan E., et al. Guidelines for counseling in infertility: outline version. Human Reproduction 2001; 16 (6): 1301-1304.
- Dunkel-Schetter C., Lobel M. Psychological reactions to infertility. In Stanton A. and Dunkel- Schetter C. (eds) Infertility; Perspectives from stress and coping research (pp 29-54). Plenum, New York, 1991.