Oladimeji Akeem Bolarinwa1*, Adekunle Ganiyu Salaudeen2, Sunday Adedeji Aderibigbe2, Omotoso Ibraheem Musa2, Tanimola Makanjuola Akande2, James Olusegun Bamidele3
1Department of Health Information Management, University of Ilorin, Ilorin, Nigeria
2Department of Epidemiology & Community Health, University of Ilorin, Ilorin, Nigeria
3Department of Community Medicine, Ladoke Akintola University of Technology, Ogbomoso, Nigeria
- *Corresponding Author:
- Dr. Bolarinwa O.A
Dept. of Health Information Management
University of Ilorin , P. O. Box 4228, (240001) Ilorin, Nigeria
Phone no – +234-80-3514-7130
Email: drdeji@yahoo.com
Keywords
Safety, injection, practice, Ilorin, Nigeria
Introduction
Injection safety is defined by WHO as an injection that is administered using appropriate equipment, does no harm to the recipient, does not expose the provider to any avoidable risk and does not result in any waste that is dangerous to other people [1,2]. Since invention of the syringe in 1848, [3] a new channel for pathogens to pass from one person to another was opened and over time while health workers found more conditions to treat and more medications to inject. The awareness regarding blood borne pathogens and hygiene only came over 100 years after the invention [4,5]. Injection therapy was first introduced to developing world population with the mass campaigns against Yaws and Kala-azar in 1920s, [6] and became wide spread after second world war following the introduction of penicillin [6].
Over the last 50 years, scientists have continued to discover new blood borne pathogens associated with unsafe injection use [7,8]. In 1967, the Australian antigen, now known as Hepatitis B Virus surface antigen (HBsAg) was first linked to viral hepatitis. In 1983, human immunodeficiency virus (HIV) was found in blood. In 1989, the hepatitis C virus (HCV) and antibodies were identified. Episodes of transmission of blood borne pathogens through injections are usually linked to the unsafe use of multi-dose vials or preparation of medications in areas potentially contaminated with blood or body fluids [6-8]. After mid-century warnings about hepatitis from injections, Doctors progressively shifted to a sterile syringe and needle for each injection [6-8].
Injection safety practices has been generally improved upon in developed countries with adequate provision of injection equipment and administration of injection under sterile conditions and equipments [7]. In developing countries however, the last half of the 20th century saw enormous increases in number of injections with insufficient care for sterile conditions [7]. Today Injection is one of the most common health care procedures in both the formal and informal heath care sector. Though in some developing countries and especially in tertiary health facilities [10,11] injection safety practices are fair because of provision of injection equipment and training of health workers but in most of the developing countries injection use have exceeded the normal rate [12-15].
Needle recapping which is an important cardinal indicator of unsafe injection practice among health workers is high in developing countries [1]. A cross country survey in Nigeria1 showed 80% prevalent while Studies in Burkina Faso [16], Oman [17] and Swaziland [18] showed 56%, 28% and 31% respectively. Local studies in Nigeria revealed high prevalence of needle recapping [19] in PHC facilities but low prevalence in tertiary health facilities [20]. In Nigeria the incidence is placed at 45% [1] however variation occurs across the country and some state has been reported to be as high as 57.8% among health workers [10]. A similar study in Lagos, Nigeria reported 72.9% [11], Swaziland study revealed more than 30% incidence among nurses, [18] 17.9% in Oman, [17] and 23.5% in Dominican Republic [21].
In Nigeria the injection safety practices is poor according to cross sectional survey on injection safety in 2004 conducted by Federal Ministry of Health (FMoH) in partnership with John Snow Incorporated/ Making Medical Injection Safer in Nigeria (JSI/MMIS) [1]. As far back as 2001 National Programme on Immunization (NPI) has introduced the use of auto-disable syringes and other injection safety equipment in immunization but national injection safety forum held later in 2005 resulted in the production of National policy on injection safety and healthcare waste management in January 2007 [20,22,23]. This policy is still poorly implemented at all levels of health care delivery in Nigeria. This study assessed the injection safety practices among the Primary Health Care Workers (PHCWs) in Ilorin metropolis
Methodology
This is a cross-sectional descriptive study carried out among PHCWs in the 3 LGAs in Ilorin metropolis, kwara state using multi stage sampling techniques. Ethical approval was obtained from Ethical Review Committee of University of Ilorin Teaching Hospital, Ilorin while informed consent was sort from the respondents before been recruited into the study. The 336 respondents were chosen using fitzers’formula [24] while multi-stage sampling techniques was used. This involved the use of simple random sampling using table of random numbers to select 10 Private and Public Primary Health Care (PHC) facilities per Local Government Authority (LGA) from the list of all PHC facilities. At the last stage equal probability systematic random sampling was used to choose the PHCWs with sample interval of between 3 and 4 at the Health facilities.
The study was carried out at the health facilities during the working hours of the week days. The Research instruments used were questionnaire and observational checklist. The questionnaire was semi structured, interviewer administered and pretested. It obtained quantitative data on socio-demography and injection safety practice. The observational checklist was administered in randomly selected health facilities in the 3 LGAs and it collected data on injection practice of health workers, disposal of needle and syringe and availability of injection equipment and supplies. The data generated from the study were manually checked for possible errors and inconsistencies before data entry using EPI-INFO software package. Level of significance was predetermined at p-value of less than 0.05.
Results
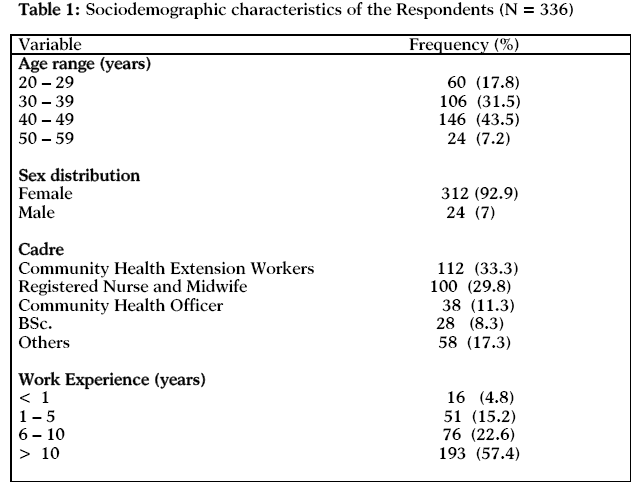
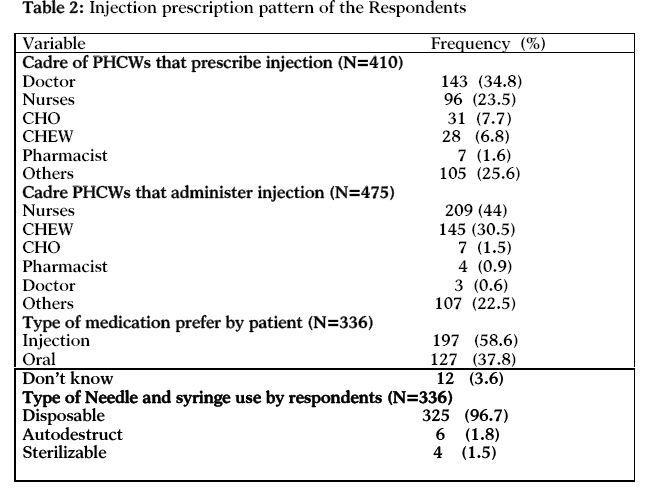
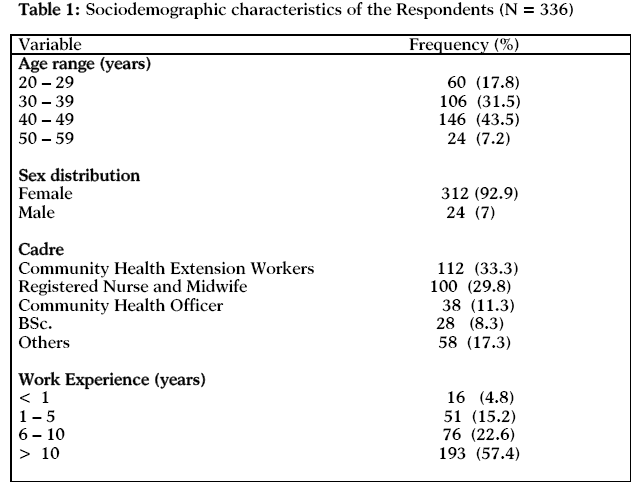
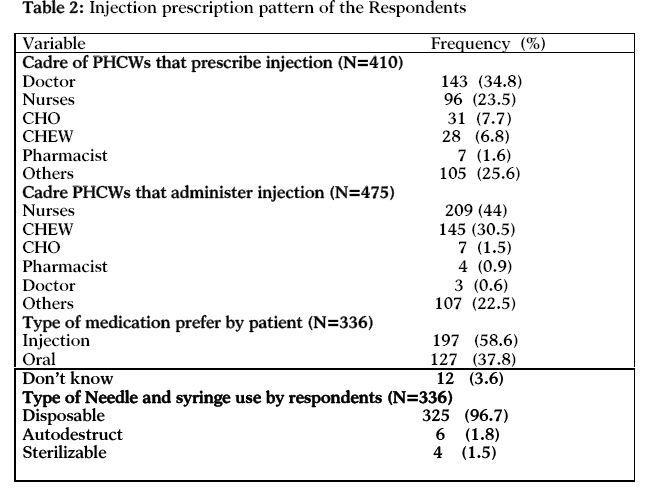
Three quarter, 252 (75%) of the PHCWs in Ilorin was within the age range 30 – 49 years while the remaining 84 (25%) were mainly below 30 years and over 50 years (Table 1). Females predominate 312 (92.9%) while Community Health Extension Workers (CHEW) and the Nurses constitute 212 (63.1%) of the PHC work force (Table 1). PHCWs with over 10 years of work experience constitute more than half (57.4%) of the respondents while those of less than a year of work experience made up of 16 (4.8%) of the respondents. Majority of the injections are prescribed by the Doctors 143 (34.8%) and Nurses 96 (23.5%) while a quarter, 105 (25.6%) of the injections are prescribed by other PHCWs like pharmacist assistance and laboratory technicians (Table 2). Injection is administered mainly by Nurses 209 (44%) and CHEW 145 (30.5%). Injection is preferred in 197 (60%) of the patients attending the PHC facilities while 127 (37.8%) patients preferred Oral medications. Almost all the PHCWs, 325 (96.7%) used disposable needle and syringe (Table 2).
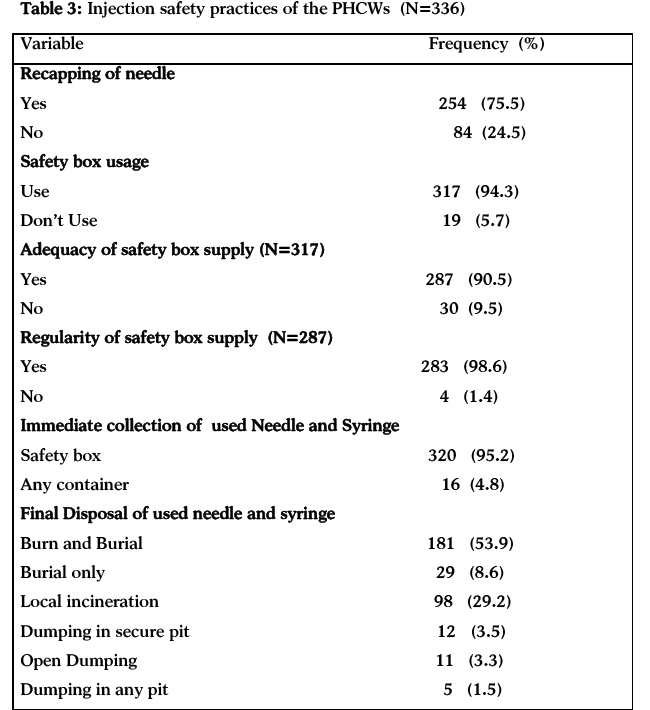
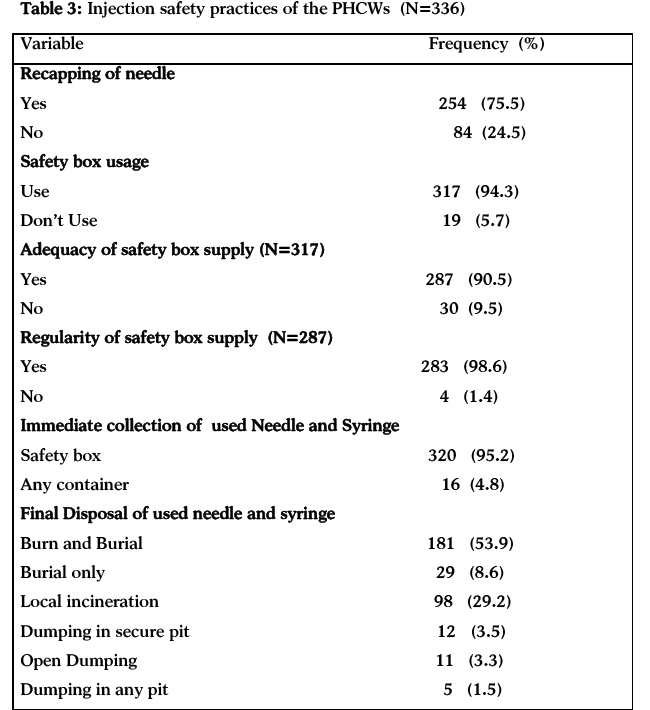
Three quarter 254 (75.5%) of the PHCWs recapped needle after given injection in their respective service units, 317 (93.4%) of them used safety box in their health facilities to collect used needle and 287 (90.5%) of them claimed that the safety box supply was adequate (Table 3). Almost all the respondents 283 (98.6%) that claimed adequacy of the safety box supply agreed that the supply was also regular. Three hundred and twenty (95.2%) of the respondents used safety box for immediate collection of used needles and syringe. One hundred and eighty one (53.9%) of the PHCWs used burn and burial and 98 (29.2%) respondents used local incineration (Table 3). Some of the PHCWs still used unsafe methods like burial 29 (8.6%), open dumping 11 (3.3%) and dumping in any pit 5 (1.5%).
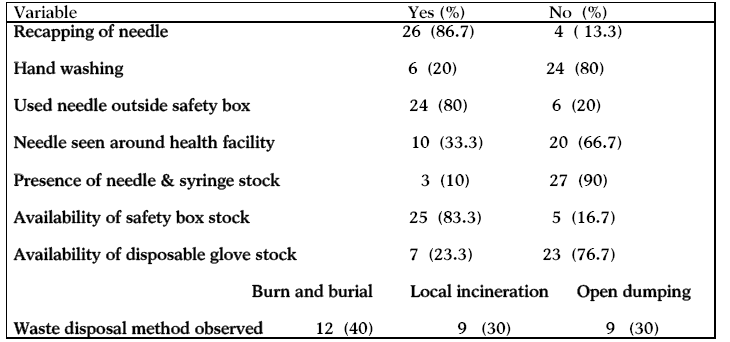
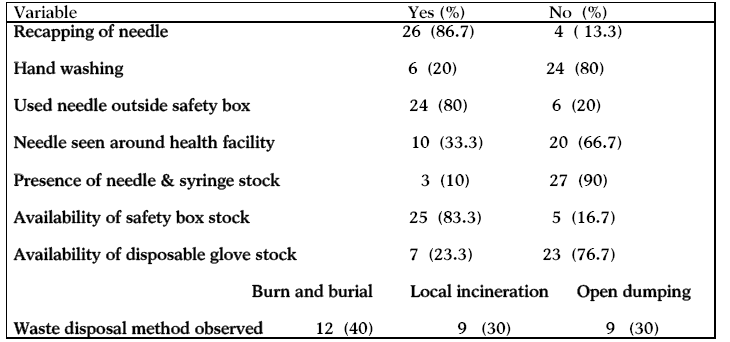
During observational checklist administration, there was needle recapping in 26 (86.7%) health facilities after administration of injection while hand washing practices before and after injection was observed in only 6 (20%) of the health facilities (Table 4). Used needles were observed outside the safety box in 24 (80%) of the health facilities and needles were seen around the health facilities in 10 (33.3%) health facilities. Twenty five (83.3%) health facilities had stock of safety box, only 3 (10%) health facilities had stock of needle and syringe and 7 (23.3%) health facilities had stock of disposable glove. Twelve (40%) health facilities used Burn and burial method for disposal of their wastes, 9 (30%) were seen using local incineration while another 9 (30%) used open dumping (Table 4).

Discussion
The respondents’ age ranged between 20 to 59 years with more than half of respondents falling within 40 to 49 years and a mean age of 39 + 8 years. This showed that majority of the PHCWs in the study area are older within productive age group as reported in a study in Nepal [25] and Ilorin [19]. The female predominates among PHCWs in this study and this corroborated the actual situations of most PHC facilities in Nigeria where nursing professions and other nursing related professions like Community Health Officers (CHO) and Community health Extension Workers (CHEW) are predominantly women.26 More than half, 193 (57.4%) of the PHCWs in the study area had more than 10 years working experience. This reflected that the health workforce in the PHC setting of the study area are made up of older workers who would be involved in administrative role. This implied that the PHC setting in the study area is made up of upper cadre staff and a reflection of inadequate staffing. It also showed a large group of workers that may be less likely involved in injection administrations.
The PHCWs in this study have preference for disposable syringes 325 (96.7%) while the small percentage 6 (1.8%) that used autodestruct was probably for the immunization services injection because of National Programme on Immunization (NPI) that is highly active in the country. There was high safety box usage 317 (94.3%) in this study (Table 3). This could be adduced largely to availability of the injection safety box due to static and fixed immunization services that are rendered in almost all the health facilities and part of the bundling method strategies for immunization equipment logistics that make it mandatory for needle, syringe, injection safety box and other injection equipments to accompany vaccines to the health facilities [27]. This observation was also supported by the observational checklist that revealed up to 83.3% of the health facilities as having injection safety box (Table 4).
This study revealed that 197 (58%) of patients attending the health facilities requested for injection medications (Table 2). This is a major reinforcing factor for unsafe injection practices because of mutually reinforcement that existed between the patients who requested for injection because of cultural beliefs and ignorance and the health workers who prescribe injection for financial and other gains.28 Although in this study Doctors 143 (34.8%) and Nurses 96 (23.5%) prescribed injection in more than half of the health facilities, quite many of injection prescription are still done by CHEW 28 (6.8%) and other technical staffs 105 (25.6%). Similar trends were also observed with administration of injections where over 50% of the injections were administered by these cadres of health workers. This portends danger to safe injection practices in PHC in Nigeria since quite many injections are being prescribed by unqualified health workers who have little or no training on managements of medical conditions that would require injections [26]. The training curriculum of these cadres of health workers do not cover administration of therapeutic injection [26] thereby putting the health workers, the patients and the whole community at risk of unsafe injection.
It was established by this study that there was high level of needle recapping among PHCWs 254 (75.5%) in the study area (Table 3). This finding was corroborated by the observational checklist of the health facilities (Table 4) which saw 26 (86.7%) recapping in the health facilities. These findings were higher than the findings among tertiary health workers in Ilorin, Nigeria,10 and in other developing countries like Burkina Faso, [16] Oman [17] (28%) and Swaziland18 (31%). It was similar to Nigerian cross country survey of 80% needle recapping prevalence [1]. The difference observed with findings form Ilorin, Burkina Faso, Oman and Swaziland were probably because the study populations were taken from a tertiary health institution where there is likely to be safer injection practices [10,11]. However the similar finding with the cross country survey reported in Nigeria (80%) was because the survey involved all the levels of health care in the country. This finding was a reflection of poor injection safety practices that characterized health care practices in the study area and the developing countries in general [12-14]. The implication of this is that the PHC which is the first point of call for over 70% of Nigeria could not guaranteed safe injection.
Despite the high usage 317 (94.3%) (Table 3), availability 25 (83.3%) (Table 4) and adequate supply 287 (90.5%) of injection safety box (Table 3), used needles were still seen in other places outside safety box in almost all the health facilities 24 (80%) observed in this study. This is similar to reports from Burkina Faso [16] and Dominican Republic [21]. This finding showed that availability of injection equipments does not necessarily result in proper usage of these equipments and this buttressed the need for supportive supervision for PHCWs. There were low stock of needles 3 (10%) and disposable gloves 7 (23.3%) in the health facilities (Table 4). This also showed the poor state of other conditions and equipment that could have effect on safe injection practices in the health facilities.
The immediate collection of used needle and syringe was largely by injection safety box. This high level of safety box usage in this study is an opportunity for safe injection practices in the health facility. Contrarily, the final disposal of injection waste (Table 3) was predominantly “dig, burn and burry” 181 (53.9%) and local incineration 98 (29.2%) which was also corroborated by observations of health facilities (Table 4). The implication of this is that while “dig, burn and burying” is desirable for developing countries like Nigeria the use of local incineration and open dumping may not be appropriate [27,28] because of other health hazards that could be associated with such practice [29-31].
Conclusion / Recommendation
Though there is high usage of safety box among PHCWs in Ilorin, there is however high unsafe injection practice among them as evident from high level of needle recapping and risky final waste disposal methods. It is recommended that there should be on the job training and supportive supervision of PHCWs on proper usage of available injection equipments by the health departments of the LGAs and provision of stocks of other injection equipments like needle and syringe and gloves for therapeutic injection administration
5307
References
- Federal Ministry of Health, John Snow Inc./making medical injection safer/Nigeria. Injection safety in the context of infection prevention and control trainer’s Guide. Do no harm Facilitator’s guide. Oct. 2006; pg 2-103.
- Hutin YJ, Hauri AM, Armstrong GL. Use of injection in health care setting worldwide, 2000: literature review and regional estimates. BMJ. 2003; 327 (7423): 1075.
- Drucker E, Alcabes PG, Marx PA. The Injection century: massive unsterile injections and the emergence of human pathogenic. Lancet 2001; 358:1989-1992.
- Bigger JW. Jaudice in syphilitics under treatment. Lancet. 1943; i: 457.
- Mac Callum FO, Bauer J. Homologous serum jaundice: transmission experiments on human volunteers, Lancet. 1944; i: 622-627.
- Nyatt HV. The popularity of injections in the third world: origins and consequences of poliomyelitis. Social science and medicine. 1984; 19: 911-915.
- Hersh B.S. Acquired immunodeficiency syndrome in Romania. Lancet. 1991; 338: 645-649.
- Hutin YJF, Chen RT; Injection safety: A global challenge. Bulletin of the WHO 1999, 77 (10); 787 – 788.
- Hauri AM, Armstrong GL, Hutin YJF. Contaminated injections in health care setting, Comparative Qualification of Health Risks; Global and Regional burdens of disease attributable to selected major risks factors. World Health Organization. Geneva 2003; 22: 1804-1849.
- Medubi SA, Akande TM, Osagbemi GK. Awareness and pattern of needlestick injury among health workers at university teaching hospital Ilorin, Nigeria. AJCEM. 2006; 7(3):183-188.
- Odeyemi K A, Onifade KA, Onifade EU. Needle Stick/Sharp injuries among Doctors and Nurses at the Lagos University Teaching Hospital. NQJHM 2005;15 (2): 50-54.
- Ashwath D. Unnecessary injection given to children under five years. India Journal of paediatrics. 1993; 60:451-454.
- Haile D, Berhane Y. Injection practice in North-western Ethiopia. Ethiopia medical Journal. 1997; 35: 117-125.
- Vos J. Improved injection practices after the introduction of treatment and sterility guideline in Tanzania. Tropical Medicine and International Health. 1998; 3: 291-196.
- Usman HR, Akhtar S, Rahbar MH, Moattar T, Luby SP. Injection in health care settings: a risk factor for acute hepatitis B virus infection in Karachi, Pakistan. Epidemiol Infect. 2003; 130(2): 293 – 300.
- Fitzner J, Aguilera JF, Yameogo A, Duclos P, Hutin YJ. Injection practices in Burkina Faso in 2000. Int J Qual Health Care. 2004 Aug;16(4):303-8.
- Al Awaidy S, Bawikar S, Duclos P. Safe injection practices in a primary health care setting in Oman. East Mediterr Health J. 2006;12Suppl 2:S 207-16.
- Daly AD, Nxumalo MP, Biellik RJ. An assessment of safe injection practices in health facilities in Swaziland. S. Afr Med J. 2004;94(3):194-7.
- Musa IO. Injection Safety Practice among Health Workers in Static ImmunisationCentres in an Urban Community of Nigeria. Niger Postgrad Med J. 2005; 12(3): 162-7.
- Federal Ministry of Health. National injection safety forum. Standard for universal precautions and Health Care waste Management Practice. Abuja, Maxls. 2005: pg 1-13.
- Moro PL, Moore A, Balcacer P, Montero A, Diaz D, Gómez V, Garib Z, Weniger BG. Epidemiology of needlesticks and other sharps injuries and injection safety practices in the Dominican Republic. Am J Infect Control. 2007; 35(8): 552-9.
- Sridhar MKC, Wahab WB, Agboola SB, Badiane A. Health care Waste Management. Handbook for developing countries. University press. Ibadan. 2009: 1-256.
- Federal Ministry of Health. National Policy on injection safety and Health care waste management. Abuja. Jan 2007; pg 1-11
- Araoye MO. Research Methodology with Statistics for Health and Social sciences. 1st edition. Nathadex Publishers. Ilorin, Nigeria. 2003; pg 120.
- Bhattarai MD, Adhikari IP, Kane A, Uprety T, Wittet S. Rapid assessment of perception, knowledge and practices related to immunization injection safety in Nepal. Joint report of Health Nepal, UNICEF and USAID Nepal office. 2001; 1-35.
- Obionu CN. Primary Health Care for developing countries. 2007. 2nd Ed. Enugu. Ezu books Ltd, 1 - 24
- Yan Y, Zhang G, Chen Y, Zhang A, Guan Y, Ao H. Study on the injection practices of health facilities in Jingzhou district, Hubei, China. Indian J Med Sci. 2006; 60(10): 407-16.
- WHO/Safe Injection Global Network (SIGN). A behaviour change to promote the safe and appropriate use of injection. 1st Ed. 2003. Geneva. Who; 2-10.
- WHO Global programme for vaccines and immunization; WHO recommended policy on safety of injection in immunization programmes. WHO document. 1998. WHO/EPI/LHIS/96.05 Rev. 1 Geneva.
- Laurent E, Maher C. Disposal and destruction of syringes and needles in Viet Nam and the Philippines. WHO unpublished document. 1998. WHO/TECHNET.98/WP5. 3-7.
- USAID. Injection safety In: Immunization essentials, A practical field guide. 2003; Usaid. Washington DC. 125 – 138.