Key words
Health care, intrahospital transport, non-ICU patients, oxygen therapy
Introduction
Hospital environment is considered safe for every patient admitted to any ward or intensive care unit (ICU) because of the availability of support equipment, technical facilities and trained staff to meet patient’s care needs. [1] However, in many cases, patients have to be transported to other departments of the hospital so as to undergo a clinical examination or invasive procedures. The transfer of patients in the hospital for diagnostic or therapeutic purposes or their transfer to specialized units of the hospital is called intrahospital transport. [2]
Although intrahospital transports are a routine procedure in modern hospitals, they have been also described as high-risk procedures. [3] Specifically, they have been associated with increased incidence of complications and subsequent increased morbidity and mortality, because they expose patients to many risks. These risks may occur due to incorrect handling during the transfer of patients, changes in the position of the patients, changes in ambient temperature, interruption of therapy (oxygen, intravenous therapy, etc.), or improper monitoring. [4]
The intrahospital transport has been of extensive research on an international level. The last 40 years, according to international literature, a large part of research interest has focused on the complications that arise during transport, their causes and the development of strategies to reduce their occurrence.
In 2007, Papson et al., [5] conducted a study for the intrahospital transport of critically ill patients. They found that the majority of adverse events occurred during transports were related to disconnection or malfunction of monitoring equipment, and disconnection of intravenous catheters. The most frequent complications were low saturation of blood oxygen (SatO2), hypotension and bleeding due to disconnection of central arterial or peripheral intravenous catheters.
In 2008, Mazza et al., [6] in their study on the transport of critically ill patients under mechanical ventilation, with measuring hemodynamic and respiratory parameters before and after the intrahospital transport, found that 32.4% of patients had complications such as hypoxemia, hypotension, and increased heart rate and breath rate.
Brokalaki et al., [7] in a study conducted in 1996, found that the disruption of oxygen therapy during the intrahospital transport of critically ill patients causes a significant decrease in PaO2 and SatO2, and an increase in heart rate.
In another study, in 2004, Brokalaki et al., [8] found that 88.6% of the interviewed head nurses of general hospitals in Greece reported that there are no protocols indicating the intrahospital transport procedure. Oxygen therapy started, regulated, and was discontinued from nursing staff without medical directives, while 92.5% of the nursing department’s nebulizers were refilled with tap water. The staff, as demonstrated by the results of the study, lacked adequate education and training on safe intrahospital transport.
Another issue that raises great interest is the creation and constant use of a specialized transport team. According to literature, the use of a specially trained transport team can reduce the rate of adverse events during intrahospital transports. [9] However, the assumption of this responsibility should be undertaken by the appropriate personnel, because as Fanara [10] poses in a study, the critically ill patients who are prepared and accompanied by an incomplete transport team are a dangerous combination. Moreover, according to McLenon [11] the use of highly trained personnel, dedicated to intrahospital transport procedures can decrease the appearance of unexpected events during transport.
In 2009, Pennsylvania patient safety advisory conducted a study for the safety of non-ICU patients undergoing an intrahospital transport. It showed that the lack of communication between staff involved in the transport is likely to cause adverse complications to patients. [12] For this reason they studied strategies for reducing this risk, including a handoff communication tool, which was used by the transport team, to ensure accurate exchange of patient information and provision of care. The results showed that this method was very effective and able to reduce unexpected adverse events.
As indicated above, most studies have dealt with the transport of critically ill patients, and few data are available concerning the transfer of non-ICU patients. For this reason, this study regards the intrahospital transport of patients not admitted to the ICU, but in medical wards. The purpose of the study was to determine the frequency of interruption of the applied treatment (oxygen therapy, intravenous therapy) during transport of non-ICU patients. In addition, SatO2 and respiratory rate were measured as effects of interruption of oxygen therapy during the transport of these patients.
Methodology
Study Design
It was an observational study, conducted in an internal medicine unit of a large general hospital in Athens, from October 2009 to March 2010.
Patients of the Study
The sample of the study consisted of 40 patients (22 men and 18 women) who met the following inclusion criteria:
1. Age ≥ 18 years.
2. Non-ICU patients, without mechanical ventilation.
3. Patients under oxygen therapy as prescribed by the physician.
4. Patients under continuous administration of intravenous therapy As prescribed by the physician
5. Patients undergoing an intrahospital transport for diagnostic tests.
The exclusion criteria were:
1. Age < 18 years.
2. Patients under mechanical ventilation.
3.Patients without oxygen therapy or under oxygen therapy without medical advice.
4. Patients without continuous administration of intravenous therapy.
5. Patients undergoing an intrahospital transport not for diagnostic tests.
Collection of Data
Data were collected using a recording data form, compiled by researchers for the purpose of the study, according to international literature. The form was concerned with the collection of the following data: (a) patient demographics,(b) clinical data (diagnosis, type of oxygen therapy, type of intravenous therapy, patients’ SatO2 before and after transport, patients’ breath frequency before and after transport),(c) parameters of the transport (distance between the nursing department and the department to which the patient was transported, duration of the transport, equipment used during the procedure) and (d) interruption frequency of the applied treatment during transfer (oxygen therapy, intravenous therapy).
The recording data form was completed by the researchers after observing the intrahospital transport procedure. Also, data was collected after examining the patient just before and immediately after the procedure. The same pulse oximeter (Nonin Go2) was used for all patients of the study to measure SatO2.
Ethical issues
The present study was approved by the Medical Ethics Committee of the hospital. The study complied with all ethical principles set by the Declaration of Helsinki. The methods of the study were restricted to recording patient data related to our study aim and no part of standard care was omitted. All patients received all the necessary information by the researcher and gave their informed written consent before entering the study.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences software (SPSS 16.0 for Windows, SPSS Inc., Chicago, IL, USA). The normality assumption was evaluated using both the Kolmogorov-Smirnov criterion (p>0.05 for all variables) and normal probability plots. Categorical data were compared by using x2 analysis, and continuous variables were compared by using t-test. The statistical significance level was defined at p<0.05.
Results
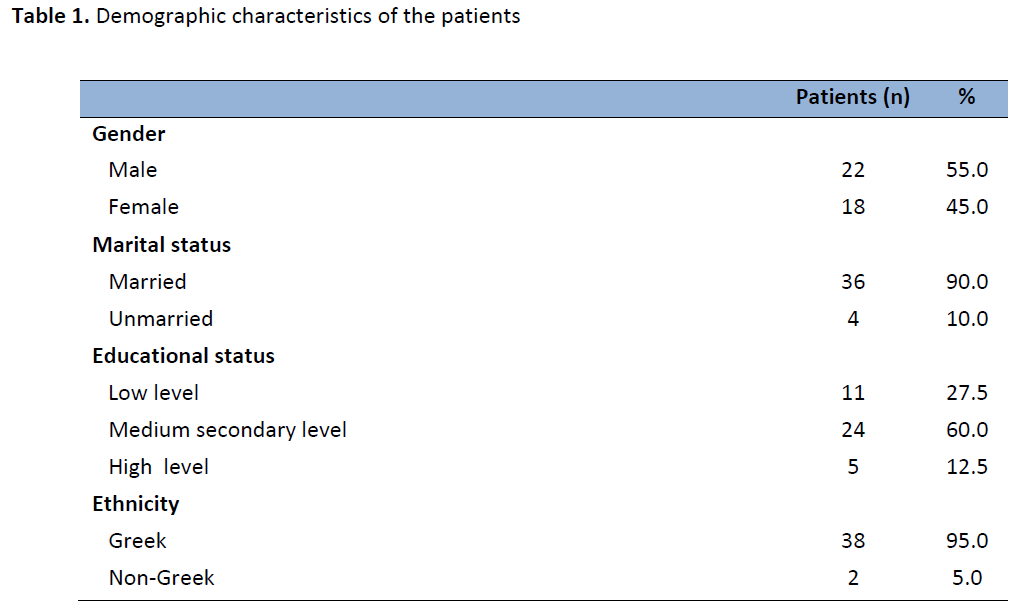
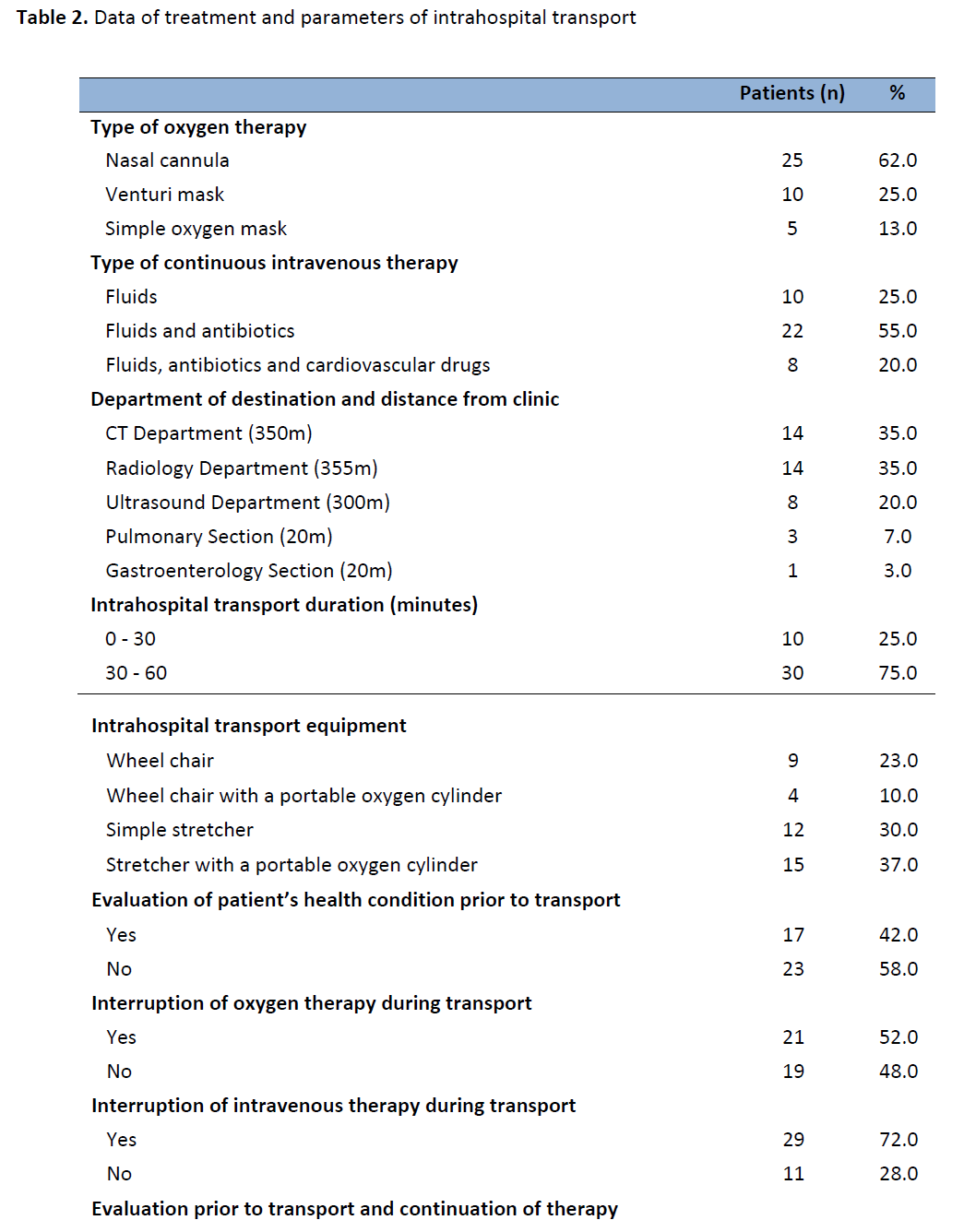
The demographic characteristics of the patients are presented in table 1. The mean age of patients was 79,3 (± 15,3) years. Table 2 summarizes data of treatment and aspects of intrahospital transport of the patients. The majority of patients (62%) received oxygen by nasal cannula. Also, 22 patients (55%) received intravenous fluids with antibiotics, whereas 8 patients (20%) received combined treatment with intravenous fluids, antibiotics and cardiovascular drugs. Most patients were transported to CT department (14 patients) and radiology department (14 patients), which are about 350 meters away from the nursing department. For 30 patients (75%) the transport lasted from 30 to 60 minutes. Most patients (67%) were transported with a stretcher (15 with and 12 without portable oxygen cylinder). Also, 23 patients (58%) left the room without a registered nurse or a doctor to evaluate their health condition before transport and in the majority of patients oxygen therapy was interrupted (21 patients) and intravenous therapy was discontinued (29 patients) prior to transport.
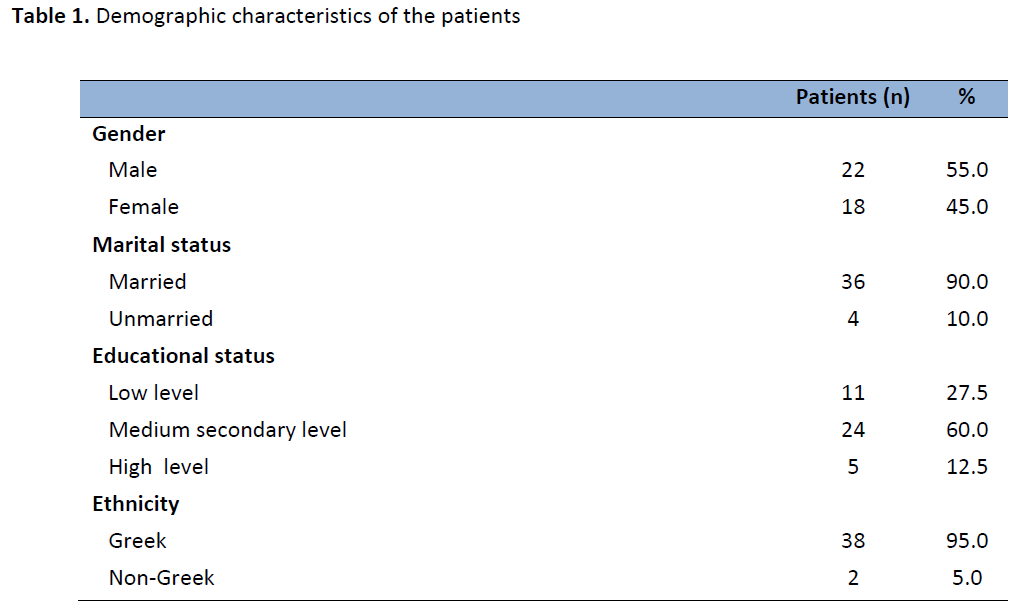
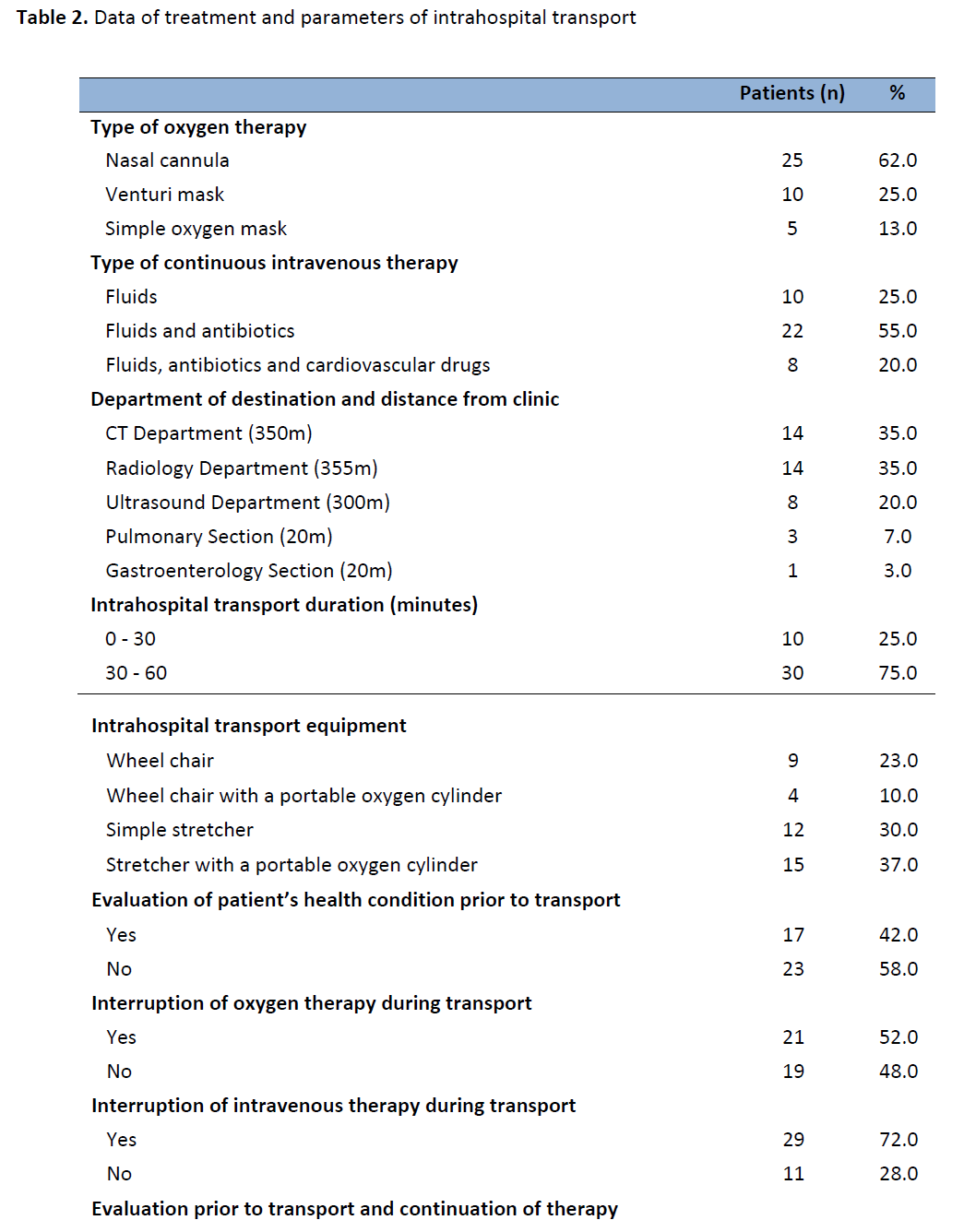
Only in 7 patients (17.5%) did a doctor or a registered nurse evaluate their health condition before transport. In those patients oxygen and intravenous therapy were not interrupted. 5 of these patients were receiving oxygen by venturi mask and 4 were under cardiovascular drugs intravenously.
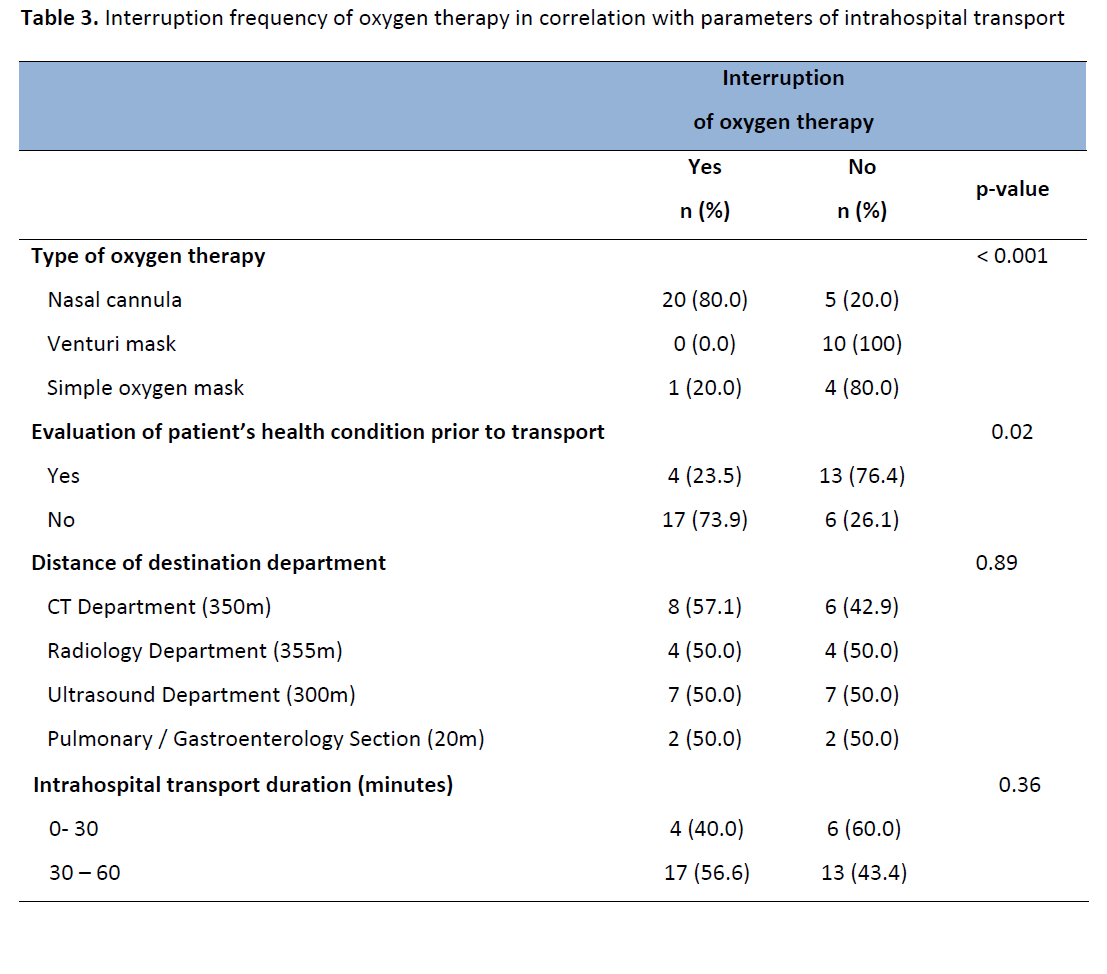
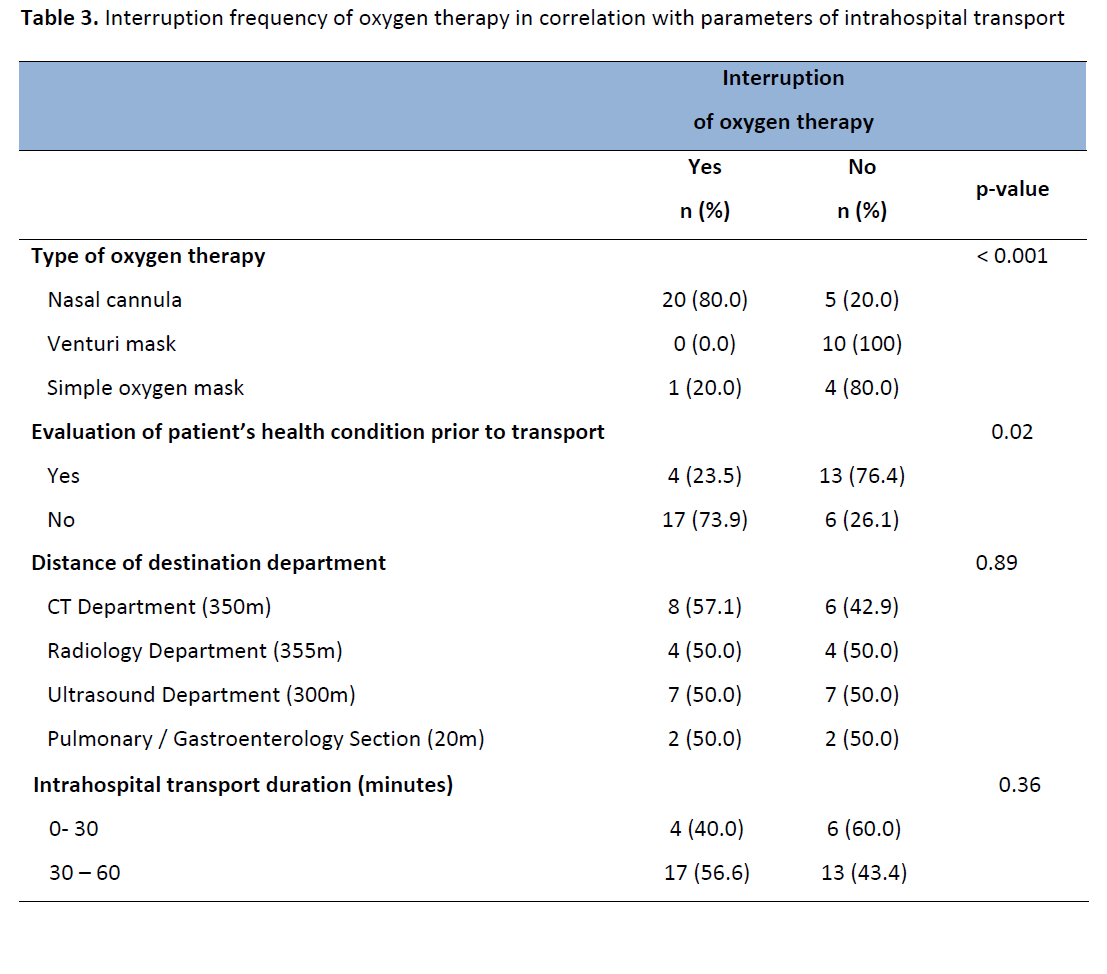
Table 3 lists the results of the correlation of specific parameters of intrahospital transport with the interruption of oxygen therapy. The parameters associated with increased rates of oxygen’s discontinuation were the administration of oxygen by nasal cannula and the absence of evaluation of patient’s health condition prior to transport. Specifically, in patients who received oxygen by nasal cannula, the interruption frequency of oxygen during transport reached 80%, which was higher than the corresponding figure for patients receiving oxygen by Venturi mask or simple face mask (p <0.001). In addition, in patients whose health condition had not been evaluated prior to transport, oxygen supply was interrupted at a higher rate (74%) than in those who did (p = 0.02).
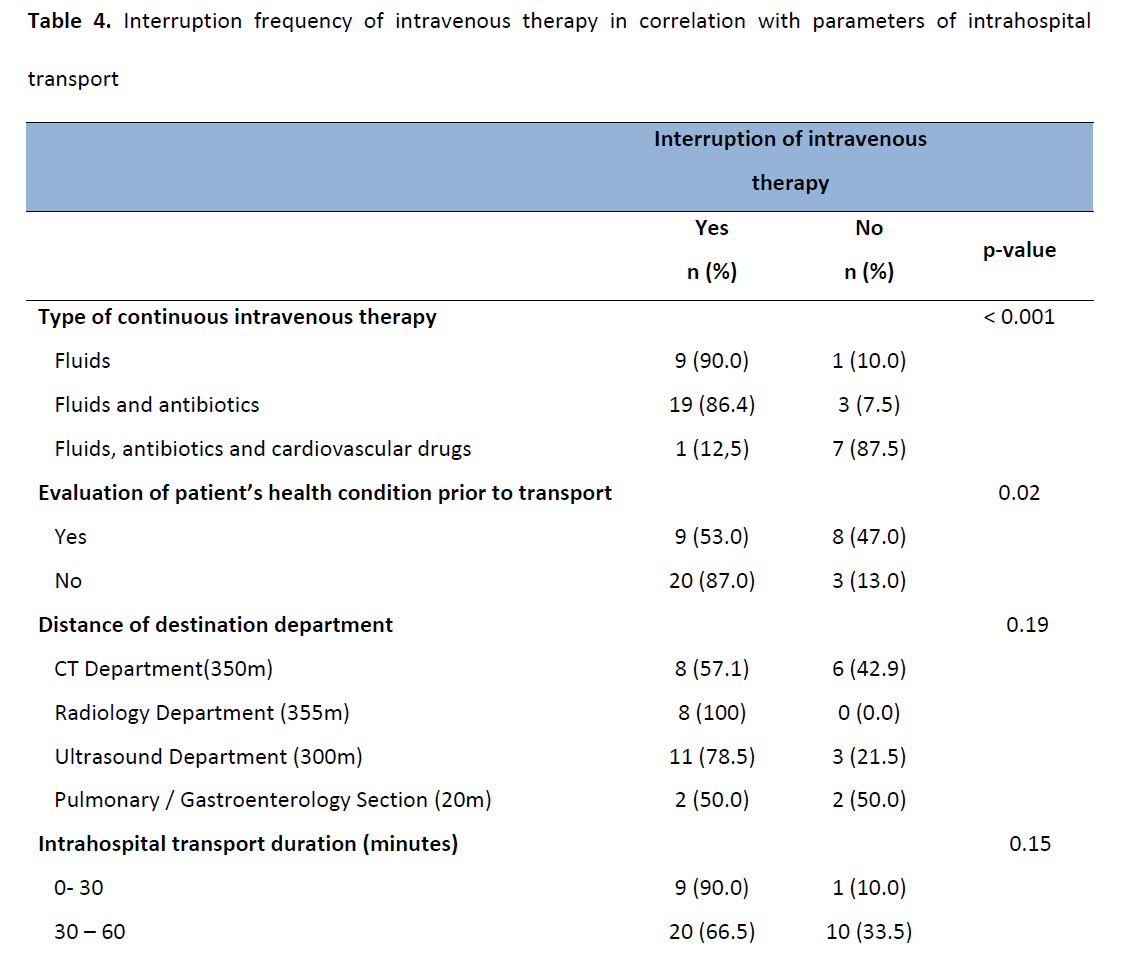
As shown in Table 4, interruption frequency of intravenous therapy was significantly increased in patients receiving only intravenous fluids (p <0.001) and in patients whose health condition was not evaluated before transport (p = 0.02).
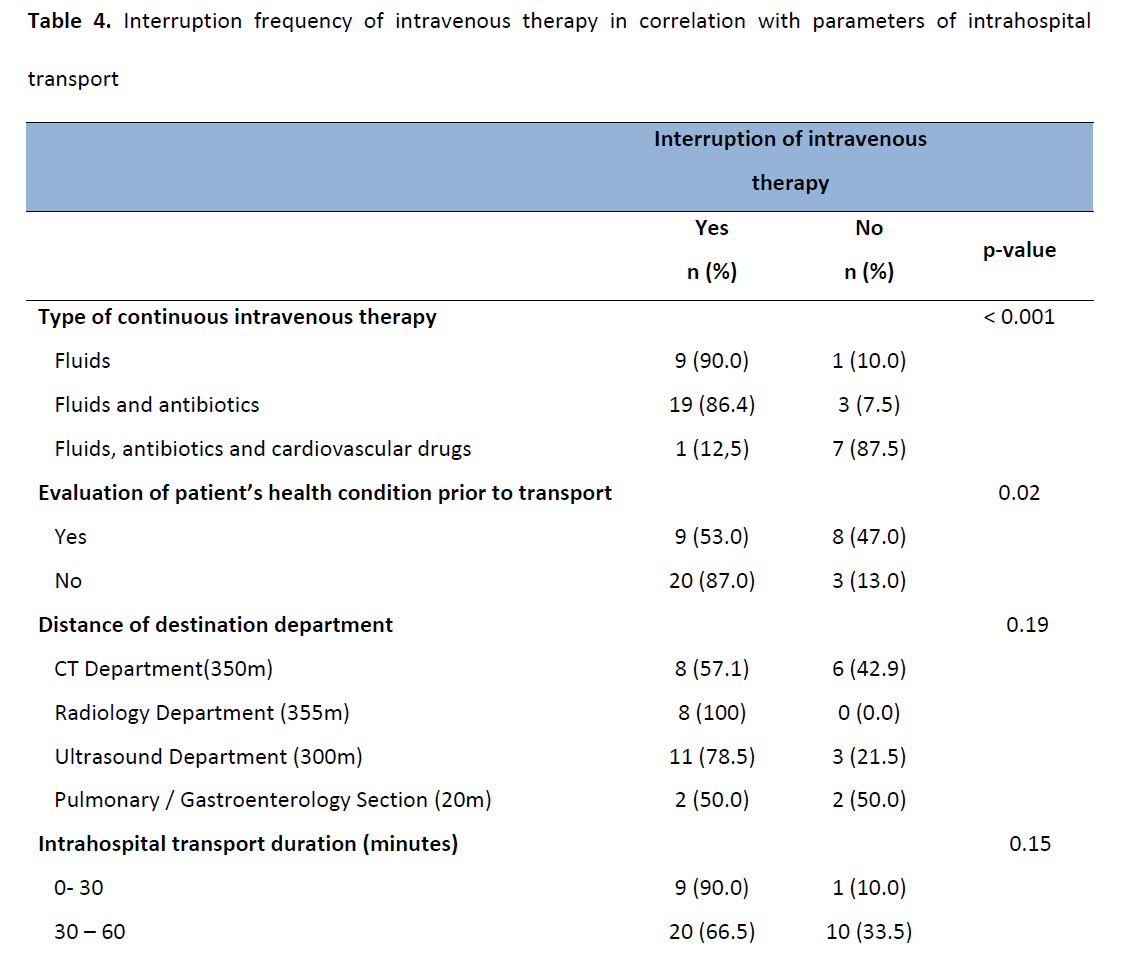
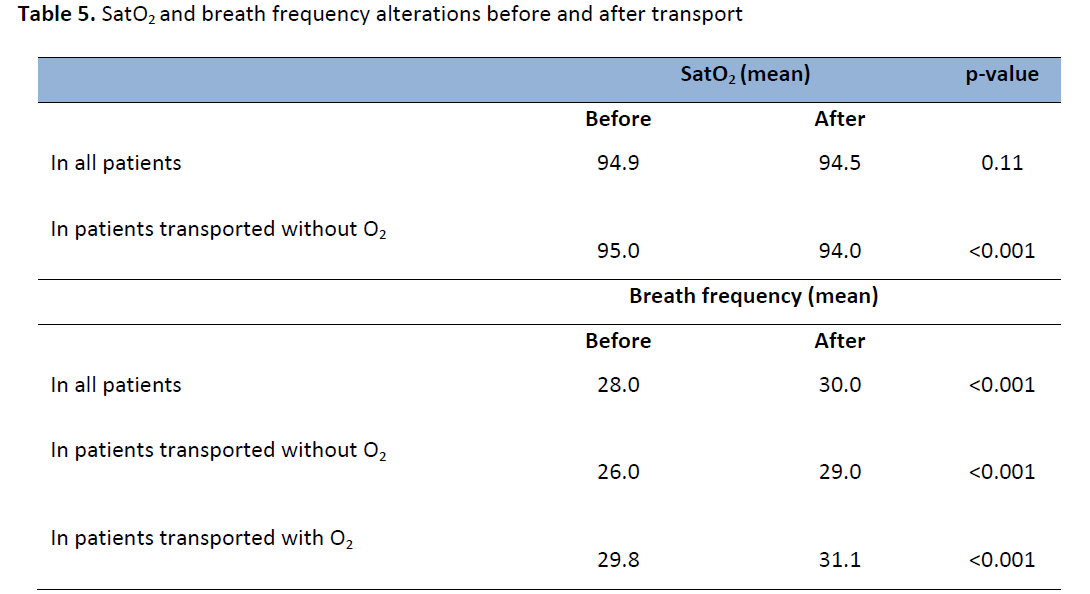
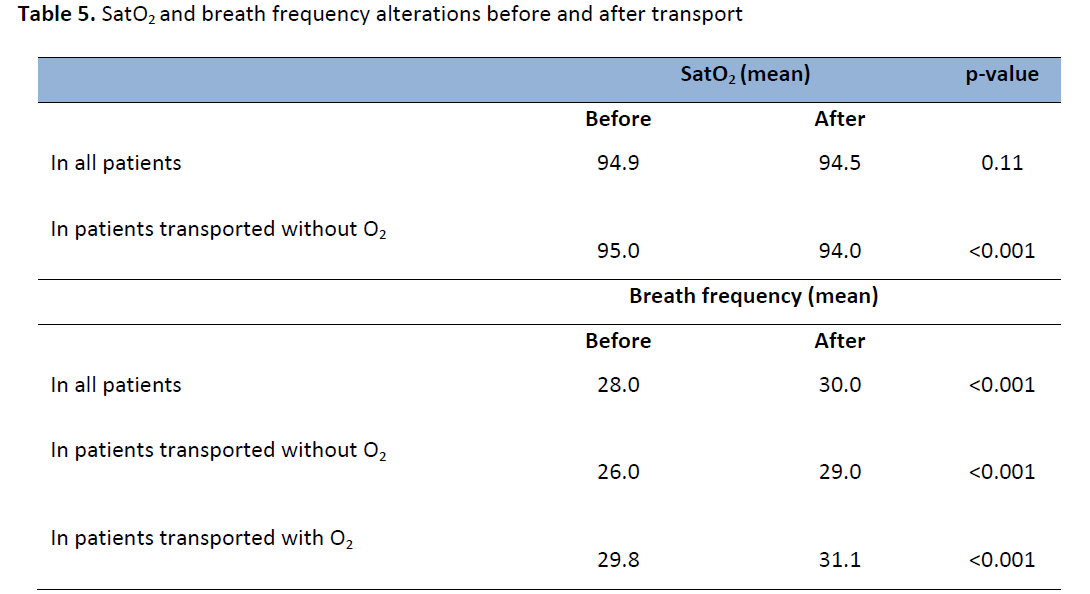
Table 5 lists the alterations in mean SatO2 and in breath frequency of patients before and after transfer. There was a statistically significant decline in SatO2 (p <0.001) and a statistically significant increase in breath rate (p <0.001) after transport in patients who were transported without oxygen. A significant increase in breath frequency of patients who were transported with administered oxygen was also observed (p <0.001).
Discussion
This study showed that the administration of therapy is very often interrupted to patients before they undergo an intrahospital transport. Specifically, 52% of patients were transported into hospital without oxygen supply. In agreement with the results of this study comes the study of Stubbs et al., [13] performed at a hospital in Seattle of U.S.A., according to which only 55% of patients were transported into hospital with oxygen supply.
Also, in 72% of patients, intravenous infusion of fluids and medicines were interrupted prior to transport. Certainly, the discontinuation of intravenous therapy should be done only rarely and after consultation with the attending physician. Even the discontinuation of intravenous administered fluids for hydration, which is the simplest form of intravenous therapy, could lead to significant effects on the health condition of the patient (hypotension, impaired renal function, etc). [7] From international literature research no studies were found regarding the interruption of intravenous therapy before an intrahospital transport.
The number of patients whose health condition was evaluated before the intrahospital transport by a registered nurse or a doctor was very low (n = 17, 42%). In addition, data showed that interruption frequency of health care was significantly higher in patients who were not checked than the corresponding figure for patients who were transported after being evaluated. Specifically, 74% and 87% of patients, who did not undergo a health condition evaluation before transport, were transported without oxygen therapy and intravenous therapy, respectively. It is obvious that the evaluation of patients before transport is necessary in order to ensure the continuation of therapy.
It was also observed that greater attention was given on the continuation of oxygen therapy to encumbered patients. Specifically, all patients under oxygen therapy with Venturi mask continued the oxygen therapy during transport at 100%, while the corresponding rate for patients receiving oxygen by simple oxygen mask was 80% and nasal cannula was only 20%. A similar reasoning was observed regarding the intravenous therapy. The continuation rate of intravenous therapy in patients receiving cardiovascular drugs, whose health condition was impaired, is quite high (87%) compared with the very low continuation rate of intravenous therapy administration in those receiving only intravenous fluids for hydration (10%) or a combination of fluids and antibiotics (14%). Apparently, nurses considered the health condition of some patients to be more serious, based on subjective assessment of their situation and provided full continuation of treatment during transport. According to Pope’s study [14] intrahospital transports of critically ill patients cause severe stress and psychological burden on staff responsible for patients’ care. The staff knowing in advance that the patient is vulnerable during transport and feeling the burden of responsibility for his care ensures the continuation of treatment. However, there have been no similar studies for non-ICU patients.
Patients, who after staff’s evaluation were transported continuing the applied treatment (n =7, 17.5%), were mainly under oxygen therapy with Venturi mask (5 patients out of 7) and intravenous treatment with cardiovascular drugs (4 out of 7), which shows that their health condition was impaired, compared with other patients of the study. It is, therefore, concluded that the review and examination of the patient before transport, by a registered nurse or a doctor, is essential because it provided in a large proportion a safest transport. However, this issue needs further investigation, since the literature is inadequate.
The distance of transport’s destination, on the other hand, did not appear to affect the interruption frequency of patient’s treatment prior to transport. The discontinuation rate is roughly the same, whether the patient is transported into sections separated by a few meters or in sections separated by hundreds of meters from nursing department.
This was, also, observed regarding the duration of the intrahospital transport. The period considered the patient to be absent was not associated with the interruption frequency of the treatment. Discontinuation rate of oxygen therapy and intravenous therapy was high, whether patients were less than 30 minutes away from their unit, or almost an hour.
In the present observational study, the effect of oxygen therapy interruption in the oxygenation of the patients (SatO2) and the number of breaths was also recorded. Patients who were transported without oxygen supply showed a statistically significant reduction on SatO2, and a statistically significant increase in breath rate after transport. This result demonstrates that the process of transport in these patients negatively affected their health status. In agreement with the results of this study, Brokalaki et al., [7] showed that the interruption of oxygen therapy during intrahospital transport caused a significant decrease in PaO2 and SatO2. Moreover, Mazza et al., [6] showed that the transport of critically ill patients is highly associated with the appearance of hypoxaemia and increased breath frequency.
Also, it was found that the hospital where the study was carried out did not follow any policy in intrahospital transport procedure. That could complicate and incommode the work of health professionals involved in the process of transport and expose patients to risk. Considering the above, it becomes necessary to create a written protocol in intrahospital transport, to staff all clinics with qualified personnel and train the non-qualified, in order to reduce complications and provide continuing therapy to all patients during intrahospital transport. To help in the completion of the above Society of Critical Care Medicine [15] has published international guidelines for safe intrahospital transport of critically ill patients, regarding the staffing, the equipment and the preparation of the patient prior to transfer. In addition to these, Australasian College for Emergency Medicine [16] has conducted minimum standards for the transport of critically ill patients, which summarize the most important elements of the intrahospital transport procedure.
In 2009, Low and Jaschinski [17] very characteristic wrote in their study that a “non-transportable” patient is just as unlikely as a “non-anesthetizable” patient, nowadays, implying that there has been great progress in intrahospital transport safety. A year later, Winter [18] conducted a study in Australia, which showed that despite the implementation of guidelines, in 44% of transport, adverse events did occur, the majority of which could have been prevented with more careful planning. Therefore, intrahospital transports, conducted very often in clinical practice, can put patients at risk.
Conclusions
The present study examined the intrahospital transport procedure of non-ICU patients and found that in a very large proportion the administration of therapy was interrupted during transport. This finding is particularly important since the study found that the interruption of oxygen affects the health condition of patients, causing a decrease in SatO2 and an increase of breath frequency. Therefore, the results of this study support the international literature that intrahospital transports can put patients at risk.
The development and maintenance of a written protocol of intrahospital transport procedures in Greek hospitals and education of nurses in minimizing the risks could significantly reduce the incidence of adverse complications and ensure the quality of care provided to patients. Certainly, there is a great need for further study of the intrahospital transports in Greek hospitals, focusing on factors associated with complications and challenges, on the education of nurses and other health professionals, in order safe transports to be performed.
This study involves certain limitations that need to be addressed. Firstly, took place only in one clinic of a large hospital of Athens and patients from other clinics and other hospitals of Athens or the region were not included, which reduces the generalisability of the study results. Second, there was a limited period of data collection in the study and a small number of patients enrolled. However, this study involved non-ICU patients undergoing an intrahospital transport measuring the interruption of oxygen and intravenous therapy, which very few studies have assessed, although various guidelines have proposed the importance of the continuation of applied therapy during transport.
3028
References
- Waydhas C. Intrahospital transport of critically ill patients. Critical Care 1999; 3 (5): R83-R89.
- Martin TE. Handbook of Patient Transportation. Greenwich Medical Media. 2001, 137 Euston Road, London.
- Jarden RJ, Quirke S. Improving safety and documentation in intrahospital transport: development of an intrahospital transport tool for critically ill patients. Intensive and Critical Care Nursing 2010; 26 (2): 101-107.
- Warren J, Fromm EJ, Orr RA, Rotello LC, Horst HM. Guidelines for the inter- and intrahospital transport of critically ill patients. Critical Care Medicine 2004; 32 (1): 256-262.
- Papson PNJ, Russell LK, Taylor D. Unexpected Events during the Intrahospital Transport of Critically ill Patients. Academic Emergency Medicine 2007; 14 (6): 574-577.
- Mazza BF, Amaral JLG, Rosseli H, Carvalho RB, Senna APR, Guimaraes HP. Safety in intrahospital transportation: evaluation of respiratory and hemodynamic parameters. A prospective cohort study. Sao Paulo Medical Journal 2008; 126 (6): 319-322.
- Brokalaki H, Brokalakis JD, Digenis GE, Baltopoulos G, Anthopoulos L, Karvountzis G. Intrahospital transportation: monitoring and risks. Intensive and Critical Care Nursing 1996; 12 (3): 183-186.
- Brokalaki H, Matziou V, Zyga S, Kapella M, Tsaras K, Brokalaki E. Omissions and errors during oxygen therapy of hospitalized patients in a large city of Greece. Intensive and Critical Care Nursing 2004; 20 (6): 352-357.
- Stearly HE. Patients’ outcomes: intrahospital transportation and monitoring of critically ill patients by a specially trained ICU nursing staff. American Journal of Critical Care 1998; 7 (4): 282-287.
- Fanara B, Manzon C, Barbot O, Desmettre T, Capellier G. Recommendations for the intra-hospital transport of critically ill patients. Critical Care 2010; 14 (3): 87.
- McLenon M. Use of a Specialized Transport Team for Intrahospital Transport of Critically ill Patients. Dimensions of Critical Care Nursing 2004; 23 (5): 225-229.
- Patient Safety Authority Commonwealth of Pennsylvania. Safe intrahospital transport of the non-ICU patient using standardized handoff communication. Patient Safety Advisory 2009; 6: 16-19.
- Stubbs CR, Crogan KJ, Pierson DJ. Interruption of oxygen therapy during intrahospital transport of non-ICU patients: elimination of a common problem through caregiver education. Respiratory Care 1994; 39 (10): 968-972.
- Pope B.B. Provide safe passage for patients. Nursing Management 2003; 34 (9): 41-46.
- Society of Critical Care Medicine. Guidelines for the transfer of critically ill patients. Critical Care Medicine 1993; 21 (6): 931-937.
- Australasian College for Emergency Medicine. Minimum standards for transport of critically ill patients. Emergency Medicine 2003; 15 (2): 197-201.
- Löw M, Jaschinski U. Intrahospital transport of critically ill patients. Anaesthesist 2009; 58 (1): 95-105.
- Winter MW. Intrahospital transfer of critically ill patients; a prospective audit within Flinders Medical Centre. Anaesthesia and Intensive Care Journal 2010; 38 (3): 545-549.