Keywords
Metallic mercury, intravenous injection, mercury poisoning, clinical manifestations
Introduction
In recent years, the risks to humans and the environment from mercury exposure have been recognised. The World Health Organization, The Agency for Toxic Substances and Disease Registry, the United Nations Environment Programme, have determined that mercury and it's compounds are considered highly toxic to humans, as high exposure can lead to death [1,2].
The mercury toxicity to humans, depends on the chemical structure, the amount absorbed, the route of exposure and the general health of the person exposed [3].
There are several reports in the literature concerning mercury intoxication and its health effects. In most cases, the reported clinical manifestations of metallic mercury exposure, are described by inhalation of mercury vapors: The most commonly reported respiratory symptoms include cough, dyspnea which can progress to pulmonary edema or fibrosis, and tightness or burning pains in the chest. Gastrointestinal effects observed include, abdominal pains, nausea and/or vomiting, diarrhea and stomatitis. Increases in heart rate and blood pressure have been reported [4].
A number of studies [5-10] have reported increases in tremors, muscle fasciculations and myoclonus. Renal effects are included, ranging from mild transient proteinuria, to acute renal failure [11-14]. Visual disturbances were also observed.
The most prominent Central nervous system symptoms include tremors (initially affecting the hands and sometimes spreading to other parts of the body), emotional lability, insomnia, memory loss, neuromuscular changes, headaches, polyneuropathy.
However, the human and animal data are generally limited to inhalation exposure of metallic vapors and oral exposure to inorganic and organic mercury compounds. There is limited dermal exposure information on adverse effects from ointments and creams that contain inorganic mercury compounds [15,16]. Data is extremely limited concerning subcutaneous and intramuscular exposure [17].
Intravenous administration of metallic Hg is a rare occurance that is usually reported in association with suicide attempts, with accidental injection, and with the attempts of drug addicts to develope new ways to become intoxicated.
A total of only 78 cases have been reported in the literature over the period 1923-2000 [18].
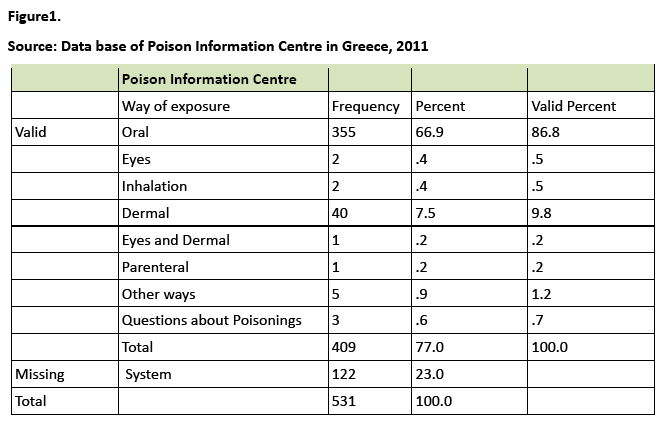
Whereas in Greece, according to the Poison Information Centre data, no cases were reported till 2012 [Figure 1].
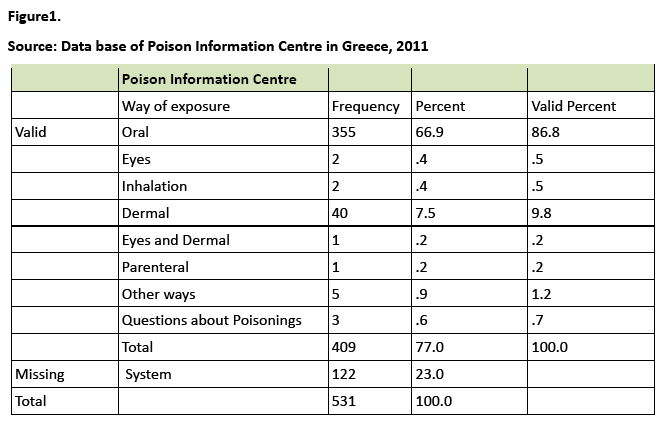
Figure 1: Source: Data base of Poison Information Centre in Greece, 2011
Here in, we report a new case report of the intravenous administration of metallic mercury. The patient was hospitalised in the Intensive Care Unit of a General Greek Hospital.
Description of the Case
We present the case of a 22 years old female patient, with no medical history, that was admitted to the hospital after the self injection of intravenous metallic mercury.
The metallic mercury had been taken from three broken thermometers in an attempt at suicide. The information was obtained from the patient.
The patient was brought to the Emergency Room by her relatives two hours after the self injection.
The Physical examination that took place in the Emergency Room, revealed normal consciousness level, with a GCS:15.
Despite complaining of a tightness in the precordial region, followed by burning pain in the chest, without respiratory distress, her vital signs were as follows: Blood pressure of 120/60mmHg, Heart Rate of 90/min, Temperature of 36.6°C and a Respiratory Rate of 17/min.
The electrocardiogram showed normal sinus rhythm, without other pathological findings.
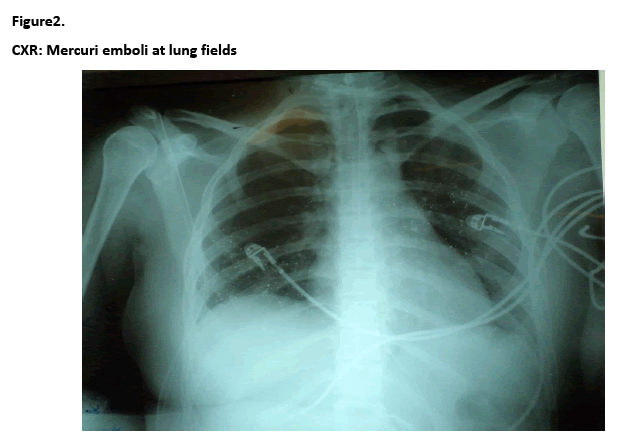
The Chest X -Ray revealed multiple, tiny metallic mercury emboli, more apparent at middle and lower lung fields [Figure 2].
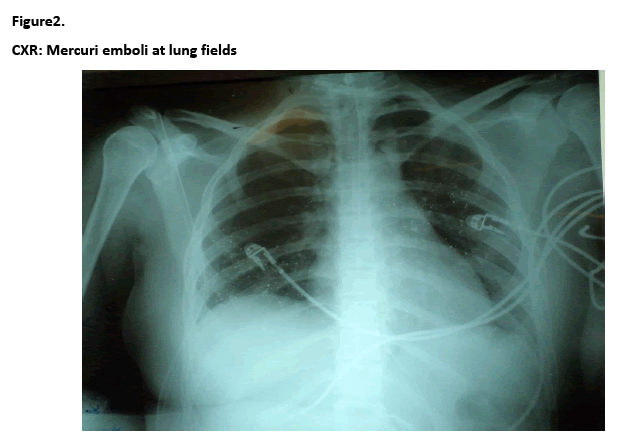
Figure 2: CXR: Mercuri emboli at lung fields
The patient was transported to the Intensive Care Unit for continuing observation and monitoring.
Initial Blood Gases on room air (FiO2 21%) were: PaO2 104mmHg, PCO2 26.5mmHg, pH 7.58, HCO3 25.1mmol/L.
From the laboratory tests, no pathological findings were found.
During the first hours following admission, the patient was awake and completely oriented to stimuli from the environment, with a GCS:15. A few hours later, she presented with a gradually descreasing level of consciousness, followed by tremor, with a GCS:9 (Verbal Response= Incomprehensible Speech: 2, Eye Response Opening= to response to pain: 2, Motor Response= Localizing response to pain: 5).
Subsequent vital signs were without significant changes: Blood Pressure of 120/55mmHg, Heart Rate of 90/min, Temperature 37.4°C and Respiratory Rate 17/min and SpO2 99%.
Therapy
A nasogastric tube was inserted and the patient started oral chelation therapy with the chelating agent DMSA – Dimecaptosuccinic acid/ succimer 800mg every 8 hours, as was recommended by the Local Poison Information Centre, based on patient's weight.
Two hours after the first dose of the chelating agent, she showed a marked improvement in her level of consciousness. She was fully awake and oriented to time and place.
Special laboratory evaluation confirmed toxic Blood and urine mercury levels. Her blood mercury concentration was greater than >35μg/l, when the normal range is below <6μg/l. Her urine mercury concentration was greater than >60μg/l, when the normal range is below <10μg/l. Biochemical parametrers of renal fuction, urea and creatinine, remained normal during her treatment in the ICU. Urea ranged from 15- 23mg/dl and creatinine from 0,66- 0,89mg/dl.
Subsequent radiografic examinations: CT scan of the chest, showed significant volumes of radiopaque foreingn bodies, (deposits of mercury), predominately in the lower and posterior lung fields. A small pleural effusion was observed. No intracardiac and pericardial mercury deposits were detectable. An abdomen CT scan demonstrated similar multiple small spherical opacities of metallic density in the liver, in the right kidney, and in the region of the spleen and the paraspinal muscles. Whereas brain CT scan was found to be normal.
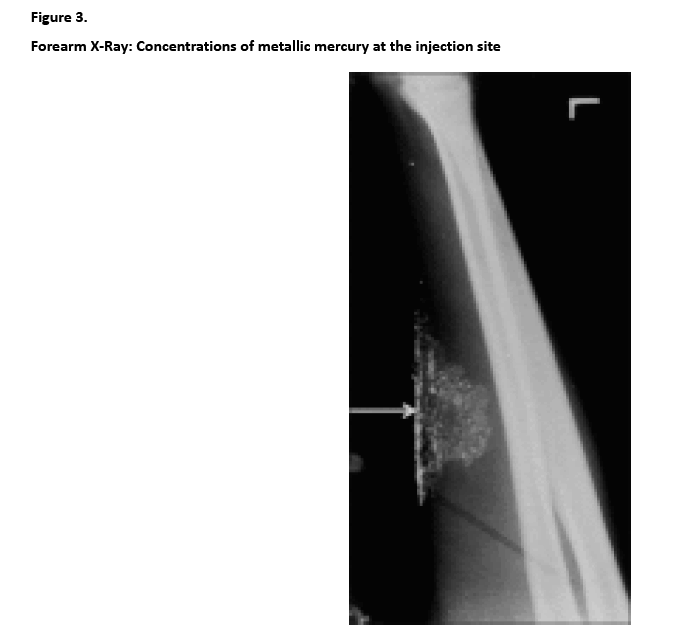
Radiological examination of the forearm, revealed small concentrations of metallic mercury at the injection site, but without the presence of localised inflammation [Figure 3].
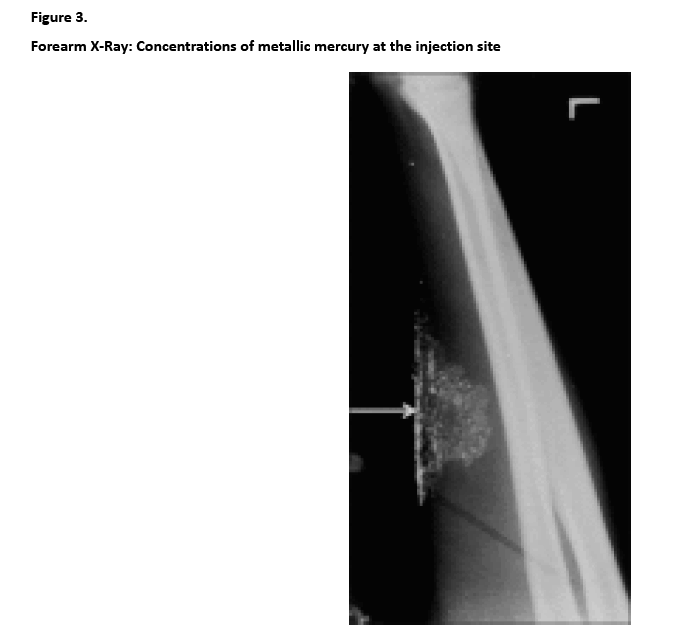
Figure 3: Forearm X-Ray: Concentrations of metallic mercury at the injection site
The patient completed the first 7- day cycle of DMSA/ succimer (800mg x3) therapy and was eventually discharged from the ICU in excellent condition.
It was recommended to continue the second 14- day cycle of DMSA/ succimer (800mg x2) on her transfer to the medical ward.
A psychiatric assessment was also recommended and further follow up of blood and urine mercury levels, in order to rule out the possibility of chronic mercury toxicity.
Discussion
Μetallic mercury, when injected intravenously, can cause a variety presentations: from a total lack of symptoms, [19] to respiratory failure, kidney damage, liver damage, neurologic symptoms, [20] and even death. Μurray and Hedgepeth [21] and De Palma et al., [22] reported the death of two patients caused by acute renal and hepatic failure, and Acute Respiratory Distress Syndrom.
Our patient, made a full clinical recovery and did not show any renal, hepatic, or pulmonary sequelae. Our observation is most in concordance with that of Bruce et al., [20] who described a patient with a gradually descreasing level of consciousness, without any other symptoms of mercury toxicity. It is important to emphasize, that it is the only case reported with this particular clinical picture.
The most common respiratory manifestations reported, are dyspnea and tightness in the chest, [20,23-25] as was found in our case.
In the present case, as in many others, alterations in liver, kidney and lung function were absent, although considerable amounts of mercury could be detected.
Radiographic examinations of most cases, describe multiple tiny metallic mercury deposits in functional organs, [20,23,26-30] as in our patient.
The usage of chelation agents in the treatment of mercury exposure is recommended. Although, in cases of intravenous exposure, its use is controversial [25,31] In the present case, the chelation theraphy with DMSA/ succimer was considered necessary.
Conclusions
Owing to the apparent rarity of the phenomenon, the immediate and long term health effects are uncertain and inconclusive.
Intravenous administration of metallic Hg is considered as an emergency condition that can cause widely varying presentations from a total lack of symptoms to respiratory failure, kindey damage, liver damage, neurological symptoms and even death. Chelation therapy is considered necessary.
Prolonged monitoring of the patient's clinical status is required to prevent early and late reactions of acute or/and chronic Hg intoxication.
2614
References
- World Health Organization (WHO). Elemental Mercury and Inorganic Mercury Compounds: Human Health Aspects. 2003
- Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Mercury. U.S. Department of Health and Human Services. Public Health Service. 1999; 1-43.Available at: https://www.atsdr.cdc.gov/toxprofiles/tp46.html. Date of access: 10.07.2012
- United Nations Environment Programme (UNEP). Global Mercury Assessment. 2002; 27 Available at: https://www.chem.unep.ch/mercury/default.htm. Date of access: 24.06.2012
- Agency for Toxic Substances and Disease Registry (ATSDR). Managing Hazardous Materials Incidents. Mercury (Hg). World Health Organization. 2006; 5-8. Available at: https://www.atsdr.cdc.gov/mhmi/mmg.46pdf. Date of access: 17.07.2012
- Fagala G.E, Wigg C.L. Psychiatric manifestations of mercury poisoning. Journal of the Amercian Academy of Child and Adolescent Psychiatry 1992; 31:306-311.
- Taueg C, Sanfilippo D, Rowens B. Acute and chronic poisoning from residential exposures to elemental mercury. Journal of Toxicology-Clinical Toxicology 1992; 30:63-67.
- Ehrenberg R.L., Vogt R.L., Smith, A.B. Effects of elemental mercury exposure at a thermometer plant. American Journal of Industrial Medicine 1991; 19: 495-507.
- Albers J.W., Kallenbach L.R., Fine L.J., Langolf G.D., Wolfe, R.A., Donofrio P.D., et al. Neurological abnormalities associated with remote occupational elemental mercury exposure. Annals of Neurology 24: 651-659.
- Mathiesen T, Ellingsen D, Kjuus H. Neuropsychological effects associated with exposure to mercury vapor among former chloralkali workers. Scandinavian Journal of Work, Environment and Health 1999; 5: 342-250.
- Letz R, Gerr F, Cragle D, Green C, Watkins J, Fidler A. Residual Neurologic Deficits 30 Years after Occupational Exposure to Elemental Mercury, Neurotoxicology 2000; 21: 459-474.
- Buchet J, Roels H, Bernard A, Lauwerys R. Assessment of renal function of workers exposed to inorganic lead, cadmium, or mercury vapor. Journal of Occupational Medicine 1980; 22:741-750.
- Langworth S, Almkvist O, Soderman, E, Wikström B. Effects of occupational exposure to mercury vapor on the ventral nervous system. British Journal of Industrial Medicine 1992; 49:545-555.
- Ellingsen D, Efskind J, Haug E, Thomassen Y, Martinsen I, Gaarder P. Effects of low mercury vapour exposure on the thyroid function in chloralkali workers. Journal of Applied Toxicology 2000b;20:483-489.
- Barregard L, Quelquejeu G, Sallsten G, Haguenoer J, Nisse C. Dose-dependent elimination kinetics for mercury in urine - observations in subjects with brief but high exposure. International Archives of Occupationaland Environmental Health 68: 345-348.
- Bourgeois M, Dooms-Goossens A, Knockaert D, Spregners D, Van Boven M, Van Tittelboom T. Mercury intoxication after topical application of a metallic mercury ointment. Dermatologica 1986;172:48-51.
- De Bont B, Lauwerys R, Govaerts H, Moulin D. Yellow mercuricoxide ointment and mercury intoxication. Eur J Pediatr 1986;145:217-8.
- Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Mercury. U.S. Department of Health and Human Services. Public Health Service. 1999; 170-171. Available at: https://www.atsdr.cdc.gov/toxprofiles/tp46.html. Date of access: 10.07.2012
- Winker R, Schaffer AW, Konnaris C, Barth A, Giovanoli A, Osterode W, et al. Health consequences of an intravenous injection of metallic mercury. Int Arch Occup Environ Health 2002; 75(8):581-6.
- Chitkara R, Seriff NS, Kinas HY. Intravenous self-administration of metallic mercury in attempted suicide. Report of a case with serial roentgenographic and physiologic studies over an 18-month period. Chest 1978; 73(2):234-6.
- Bruce A, Shaffer M, Wolfgang W. Multiple small opacities of metallic density in the lung. 21. American College of Chest Physicians 1989;96(5):1179-1181.
- Murray KM, Hedgepeth JC. Intravenous self-administration of elemental mercury: efficacy of dimercaprol therapy. Drug Intell Clin Pharm 1988; 22(12):972-5.
- De Palma G, Mariotti O, Lonati D, Goldoni M, Catalani S, Mutti A, et al. Toxicokinetics and toxicodynamics of elemental mercury following self-administration. Clin Toxicol (Phila) 2008; 46(9):869-76
- Maniatis V, Zois G, Stringaris K. I.v. Mercury self-injection: CT imaging. AJR Am J Roentgenol 1997;169(4):1197-8.
- Giombetti RJ, Rosen DH, Kuczmierczyk AR, Marsh DO. Repeated suicide attempts by the intravenous injection of elemental mercury. Int J Psychiatry Med 1988;18(2):153-67.
- Wale J, Pankaj K Yadav, Shairy G. Intravenous administration/infusion of metallic mercury. Case report and literature review. Indian J Radiol Imaging 2010;(2):147–149.
- Kedziora A, Duflou J. Attempted suicide by intravenous injection of mercury: a rare cause of cardiac granulomas. A case report. Am J Forensic Med Pathol 1995;16(2):172-6
- McFee RB, Caraccio TR. Intravenous mercury injection and ingestion: clinical manifestations and management. J Toxicol Clin Toxicol 2001;39(7):733-8.
- Kedziora A, Duflou J. Attempted suicide by intravenous injection of mercury: a rare cause of cardiac granulomas. A case report. Am J Forensic Med Pathol 1995;16(2):172-6.
- Dell' Omo M, Muzi G, Bernard A, Filiberto S, Lauwerys RR, Abbritti G. Long-term pulmonary and systemic toxicity following intravenous mercury injection. Arch Toxicol 1997; 72(1):59-62.
- Peterson N, Harvey- Smith W, Rohrmann CA. Radiographic aspects of metallic mercury embolism. Am J Radiol 1980; 135:1079-81.
- Gopalakrishna A, Pavan Kumar T. Intravenous injection of elemental mercury: A report of two cases. Indian J Plast Surg 2008;41(2):214–218.