Sarah-Jayne Campbell1*, Helen Williams1, Lino Locurcio2 and Alex Creedon2
1DCT-1 Ashford and St. Peters Hospital, London Road, Ashford, Surrey, UK
2Department of Oral Maxillofacial Surgery, Ashford and St Peters hospital, London Road, Ashford, Surrey, UK
*Corresponding Author:
Sarah-Jayne Campbell
DCT-1 Ashford and St. Peters Hospital
London Road, Ashford, Surrey, UK
Tel: 07591128753
Email: sjcampbell06@hotmail.com
Received date: March 22, 2017; Accepted date: April 06, 2017; Published date: April 10, 2017
Citation: Campbell SJ, Williams H, Locurcio L, et al. Isolated Hypoglossal Nerve Palsy: A Case Report. J Neurol Neurosci. 2017, 8:2. doi:10.21767/2171-6625.1000184
Keywords
Hypoglossal nerve; Palsy; Unilateral
Introduction
Innervation of the extrinsic and intrinsic muscles of the tongue, excluding only the palataoglossus, is from the twelfth cranial nerve. The hypoglossal nerve is primarily motor in function and controls tongue movement, meaning palsy of this nerve can result in altered movement and appearance of the tongue, with swallowing and speech difficulties. Hypoglossal nerve palsy usually presents with additional neurological symptoms, its presentation in isolation is rare [1]. This was apparent following review of the literature which revealed mostly single cases in isolation and only a very limited selection of small case series having previously been published [2,3].
Case Report
A 59-year-old gentleman presented to the Oral and Maxillofacial Department at Ashford and St. Peters hospital with a history of decreased tongue mobility. The patient complained of sudden slurred and difficult speech which began four months previously.
Medically the patient had well controlled hypertension and benign prostatic hyperplasia. Recent medical history included pneumonia which had resolved by the time of the first visit. Previous investigations prior to his visit to our department included a normal brain MRI: Magnetic Resonance Imaging, indicating that stroke and TIA: Transient Ischaemic Attack, was ruled out by the investigating specialist team.
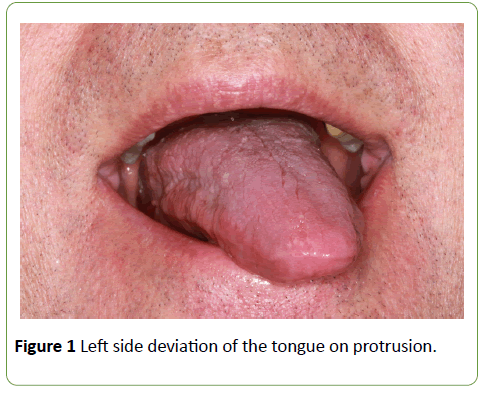
Clinical examination revealed an abnormality of the motor function of the tongue causing left side deviation on protrusion (Figure 1). Sensory function was intact and no other neurological deficits were evident. Following palpation of the left submandibular triangle, a possible mass was detected at level 1b: submandibular nodes, of the neck. Futher investigations included further MRI from base of the skull to the clavicle as well as computerised tomography CT scan of thorax and abdomen. These revealed no mass or lymphadenopathy in the neck, however multiple pulmonary nodules and liver lesions, suggestive of widespread metastatic disease were detected.
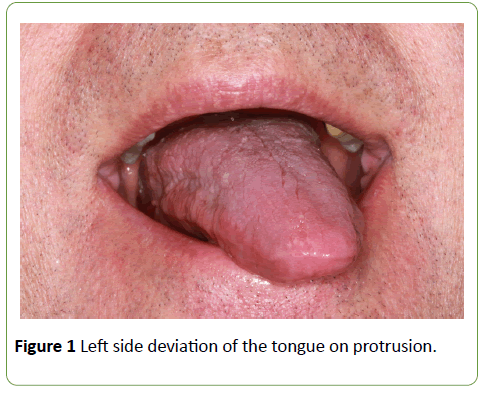
Figure 1:Left side deviation of the tongue on protrusion.
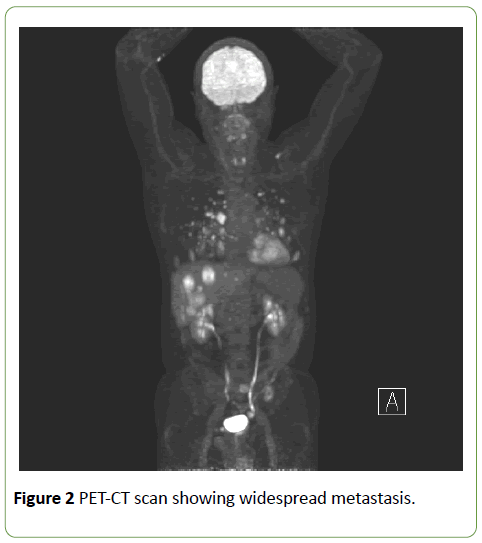
Subsequent investigations with a PET-CT (Positron Emission Tomography–Computed Tomography), confirmed a skull base lesion. The investigations revealed that the right occipital condyle was affected, which is likely to have compromised the right hypoglossal nerve within the hypoglossal canal likely to be the origin of the palsy. Furthermore widespread metastatic lesions in the lungs, liver, bone and muscle were identified (Figure 2).
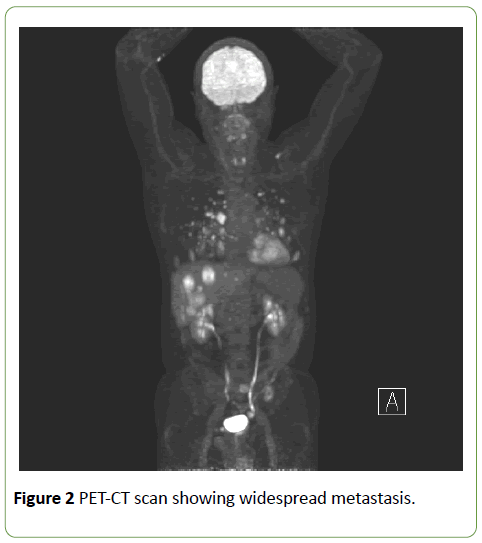
Figure 2:PET-CT scan showing widespread metastasis.
On the PET imaging, a visible FDG (Fluoro-De-Oxyglucose)- avid paravertebral mass at the level of the 9th thoracic vertebra was evident; therefore a core biopsy of this lesion was taken in order to obtain a tissue diagnosis. The tumour was originally thought to be consistent with a high grade sarcoma but following immunohistochemistry and a review of the case, it was confirmed as a grade 2 FNCLCC: Fédération Nationale des Centres de Lutte Contre le Cancer, leiomyosarcoma.
At the time of writing the patient is currently undergoing palliative radiotherapy and a primary malignancy has not been identified.
Conclusion
Hypoglossal nerve palsy tends to occur as a sign rather than a symptom [4] and therefore warrants thorough investigation. When it presents in isolation it can be diagnostically challenging as was evident in this case. Excluding previous surgery, radiotherapy and trauma, 50 per cent of cases of isolated hypoglossal nerve palsy are idiopathic. A further 20 per cent are malignant, 20 per cent are of a vascular cause such as dolichoectasia of the vertebral artery and dissection of extracranial internal carotid artery. The remaining 10 per cent are due to miscellaneous causes [1]. Keane and colleagues carried out the largest case series to date however they also included hypoglossal palsies that were not found in isolation, his results found malignancy to be the cause in 85% of cases. Presentation of an isolated hypoglossal nerve palsy is therefore an ominous sign [1]. Careful imaging of the brain, skull base and cervical spine should be performed, especially if cranial nerve palsy develops [5]. This case highlights the importance of developing a systematic approach in investigation of an isolated hypoglossal nerve palsy in order to prevent the overlook of an underlying sinister cause [4,6].
Conflict of Interest
We have no conflicts of interest
Ethics Statement/Confirmation of Patient’s Permission
The patient gave consent for the use of photographs for this paper.
18910
References
- Khoo S, Ullah I, Wallis F (2007) Isolated hypoglossal nerve palsy: A harbinger of malignancy. J LaryngolOtol 121: 803-805.
- Combarros O, DeArcaya A,Berciano J (1998) Isolated unilateral hypoglossal nerve palsy: Nine cases.J Neurol 245: 98-100.
- Boban M, Brinar V, Habek M(2007) Isolated hypoglossal nerve palsy: A diagnostic challenge. EurNeurol58: 177-181.
- Orliac C,De Champfleur SM, Ducros A (2015) Occipital neuralgia heralding occipital condyle syndrome revealing vesicalleiomyosarcoma skull base metastasis. J NeuRad42: 368-370.
- Ho MW, Fardy MJ, Crean SJ (2004) Persistent idiopathic unilateral isolated hypoglossal nerve palsy: A case report. Br Dent J 196: 205-207.