Laghi FA1, Gumani G1,2 and Casserly B1,2*
1University of Limerick, Limerick, Ireland
2Division of General Medicine, Pulmonary and Sleep Medicine, University Hospital Limerick, Limerick, Ireland
Corresponding Author:
Casserly B
Division of General Medicine
Pulmonary and Sleep Medicine
University Hospital Limerick, St Nessan's Rd
Dooradoyle, Co. Limerick, Ireland
Tel: +353860454909
E-mail: brian.casserly@hse.ie
Received date: November 29, 2016; Accepted date: December 05, 2016; Published date: December 13, 2016
Citation: Laghi FA, Gumani G, Casserly B, et al. Large Thoracic Teratoma with Gastro-intestinal Presentation. Arch Med. 2016, 8:6 doi: 10.21767/1989-5216.1000180
Copyright: © 2016 Laghi FA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Keywords
Diarrhea; Tumors; Hernia; Gastritis
Case Report
Intrathoracic teratomas are extremely rare germ-cell tumors. They typically occur in the anterior mediastinum. Intrathoracic teratomas can rupture into the tracheobronchial tree and can undergo malignant transformation. For these reasons, surgical resection is the treatment of choice. Here, we report the case of a 27-year-old woman with an intrathoracic mature teratoma, presenting with abdominal discomfort and diarrhea erroneously considered to be caused by coeliac disease.
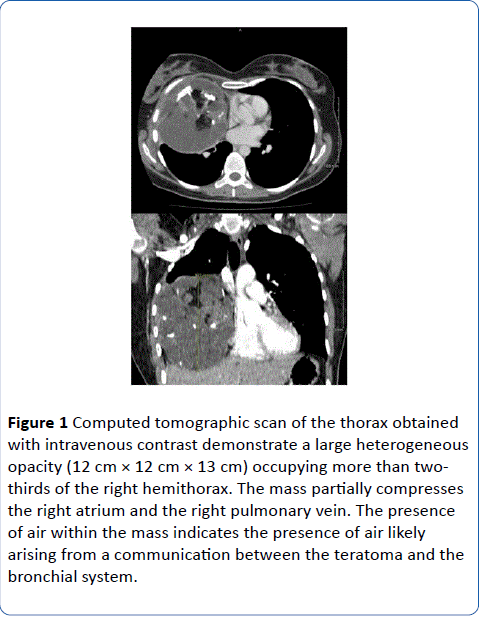
A 27-year-old woman with no past medical history was admitted to the hospital for evaluation of nausea, epigastric discomfort and loose stools. Her physical exam was unremarkable. On the suspicion of coeliac disease, the patients underwent upper endoscopy revealing only a hiatal hernia and gastritis. She also underwent colonoscopy which was unremarkable, as were multiple biopsies of the upper and lower gastrointestinal tract. Diagnosis of coeliac disease was excluded. The patient was treated with proton pump inhibitors yet her symptoms persisted. Accordingly, she underwent computer tomography (CT) of the abdomen that incompletely visualized a large mass above the right hemi diaphragm. This finding prompted respiratory team consultation. A dedicated CT of the thorax was performed. The latter demonstrated a large rightsided mediastinal mass (Figure 1).
Figure 1: Computed tomographic scan of the thorax obtained with intravenous contrast demonstrate a large heterogeneous opacity (12 cm × 12 cm × 13 cm) occupying more than twothirds of the right hemithorax. The mass partially compresses the right atrium and the right pulmonary vein. The presence of air within the mass indicates the presence of air likely arising from a communication between the teratoma and the bronchial system.
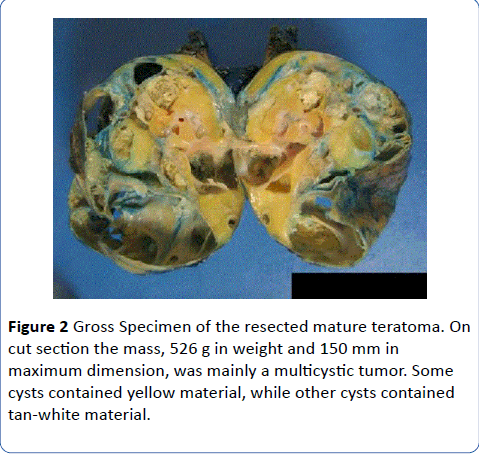
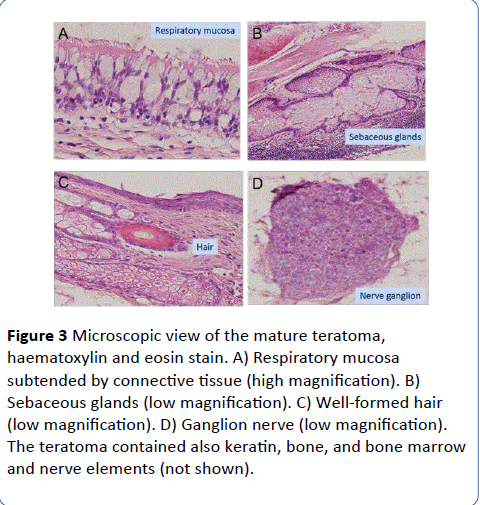
The mediastinal mass, arising adjacent to the thymus, was resected (Figure 2), and a mature benign teratoma with components of all three germ-cell layers was diagnosed on pathological evaluation (Figure 3). No immature elements or germ cells or somatic malignancy was identified. A resected mediastinal lymph node had no evidence of malignancy. Following surgery, the patient made an excellent recovery. Epigastric discomfort and loose stools resolved post-operatively.
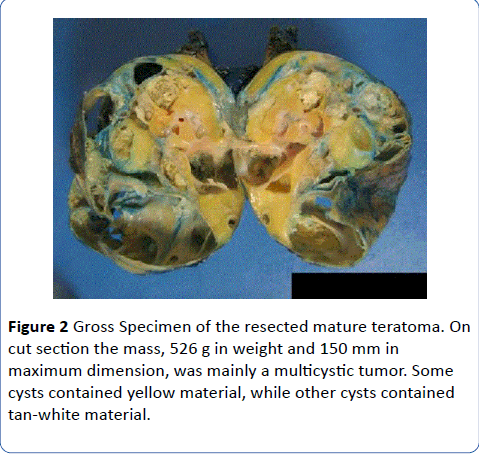
Figure 2: Gross Specimen of the resected mature teratoma. On cut section the mass, 526 g in weight and 150 mm in maximum dimension, was mainly a multicystic tumor. Some cysts contained yellow material, while other cysts contained tan-white material.
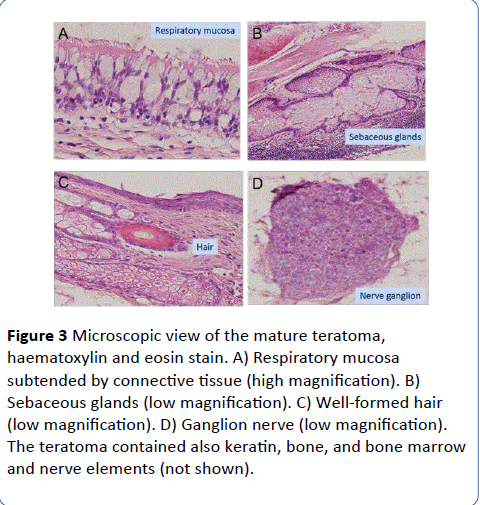
Figure 3: Microscopic view of the mature teratoma, haematoxylin and eosin stain. A) Respiratory mucosa subtended by connective tissue (high magnification). B) Sebaceous glands (low magnification). C) Well-formed hair (low magnification). D) Ganglion nerve (low magnification). The teratoma contained also keratin, bone, and bone marrow and nerve elements (not shown).
Discussion
Teratomas, the commonest type of germ cell tumor, arise during the early stages of embryonic development. Due to their slow growth, teratomas are usually diagnosed between the second and fourth decade of life [1]. Whether the site of primordial origin is the third bronchial cleft or from nests of germinal cells along the urogenital ridge remains controversial [2,3].
Histologically, teratomas can be classified as immature and mature [4]. Immature teratomas, which account for approximately one third of all mediastinal germ cell tumors [5], contain fetal and neuroendocrine tissue [4]. Mature teratomas, which account for approximately two thirds of all mediastinal germ cell tumors [6], contain at least two of the three germ layers found in embryonic life: ectoderm, mesoderm and endoderm [2]. Immature teratomas are usually malignant in nature. In contrast, less than 1% to 2% of mature teratomas undergo malignant transformation [2,7,8], including transformation to sarcomas [9] and adenocarcinomas [8]. Two mechanisms may be involved with malignant transformation. In some patients, particularly if elderly, cells in the teratoma spontaneously become malignant. In other patients, particularly younger ones, the malignant transformation may be triggered by administration of chemotherapy or radiotherapy [10].
Teratomas are usually located in or near the anatomical midline-gonads, retroperitoneum and sacrococcygeal region [11], the path of germinal cell migration during embryogenesis [3]. Less than 3% are located in the mediastinum [4]. Most teratomas in the mediastinum are mature teratomas, and they account for approximately 10% of all mediastinal tumors [4]. Half of all patients diagnosed with a mediastinal teratoma are asymptomatic [12]. When present, symptoms may include dyspnea, back or shoulder pain, bulging of the anterior chest wall, hemoptysis, recurrent pneumonia and, rarely, superior vena cava syndrome [7]. Mature mediastinal teratomas can occasionally invade the surrounding structures or they can rupture into the mediastinum or pleura. Rupture of a mature teratoma into an airway can trigger expectoration of sebum or the pathognomonic expectoration of hair (trichoptysis) [4]. Bronchiectasis secondary to exocrine secretions form the tumor have been described in patients with mature teratomas containing pancreatic acinar tissue [9].
Typical in the presentation of our patient was her age, 27 years, the mean age at diagnosis of mature teratomas [7]. Epigastric pain and diarrhea, however, are unusual. Indeed, to the best of our knowledge, epigastric pain and diarrhea have never been described as the presenting symptom in patients with mediastinal teratomas.
Nearly 40% of mediastinal teratomas rupture, most frequently into the lung and bronchial tree, followed by the pleural space, pericardial space with secondary tamponade, or great vessels [13]. None of this occurred in our patient. Accordingly, none of these complications could have been responsible of the patient’s symptoms. Teratomas tend to accelerate in growth during adolescence and early adulthood [6]. Whether accelerated growth contributed to our patient’s symptoms is impossible to determine considering the lack of chest imaging before her clinical presentation.
In this patient, the close proximity of the mature teratoma to the thymus, which was included in the surgical resection, could be a clue that the teratoma derived from the third endodermal pharyngeal pouch where the initial clustering of embryonic cells or analge for the thymus reside [14].
Typically, as was the case in our patient, CT images of mature teratomas demonstrate a heterogeneous soft-tissue rounded mass with sharp margins in the anterior mediastinum that combines soft tissue, punctate calcification, fat attenuation and fluid-containing cysts. Only occasionally magnetic resonance imaging, bronchoscopy and CT-guided biopsy are necessary in the diagnostic workup of suspected mature teratomas [4]. When the teratoma ruptures into a bronchus, hair-like material may be seen during bronchoscopy [12]. Laboratory exams are usually noncontributory yet; a Japanese patient with mediastinal mature teratoma containing benign pancreatic tissue had increased serum levels of CA 19-9, a protein that can be elevated in pancreatic cancer [15]. Human chorionic gonadotropin and alpha-fetoprotein are not increased in patients with mature teratomas.
For several reasons, aggressive surgical intervention should always be pursued in the treatment of mature teratomas. First, it allows definitive confirmation of the diagnosis. Second, it addresses presenting symptoms. Third, it prevents future complications-including life threatening hemoptysis and malignant transformation. When it occurs, malignant transformation, now referred to as germ cell tumor with somatic-type malignancy [8], can be difficult to diagnose in its early stages because malignancy may be restricted to localized area(s) and may affect only one of the tissue components of an otherwise benign-looking tumor [8,16]. Most mature teratomas can be excised en block as local invasion is rare yet described [17]. In the absence of local invasion, recurrences are rare [18-20]. When local invasion occurs, subtotal resection is worth pursuing as it can provide symptomatic relief [2].
17925
References
- Smith CJ (1967) A teratoma of the lung containing teeth.Ann R CollSurgEngl 41: 413-422.
- Duwe BV, Sterman DH, Musani AI (2005) Tumors of the mediastinum.Chest 128: 2893-2909.
- Raoufi M, Herrak L, Benali A, Achaachi L, El Ftouh M, et al. (2016) Mediastinal Mature Teratoma Revealed by Empyema.Case Rep Pulmonol 2016: 7869476.
- Murray J, Amin F, Shah S, Cooper S (2013) Mature teratoma of the thymus.
- Zenker D, Aleksic I (2004) Intrapulmonary cystic benign teratoma: a case report and review of the literature.Ann ThoracCardiovascSurg 10: 290-292.
- Machuca JS, Tejwani D, Niazi M, Diaz-Fuentes G (2010) A large ruptured mediastinal cystic teratoma.J BronchologyIntervPulmonol 17: 269-272.
- Stella F, Davoli F (2011) Giant mediastinal mature teratoma with increased exocrine pancreatic activity presenting in a young woman: a case report. J Med Case Rep 5: 238.
- Muramatsu T, Nishii T, Ohmori K, Shiono M (2011) Mature cystic teratoma with malignant transformation to adenocarcinoma.Ann ThoracSurg 91: 1971-1973.
- Sawant AC, Kandra A, Narra SR (2012) Intrapulmonary cystic teratoma mimicking malignant pulmonary neoplasm.
- Morinaga S, Nomori H, Kobayashi R, Atsumi Y (1994) Well-differentiated adenocarcinoma arising from mature cystic teratoma of the mediastinum (teratoma with malignant transformation). Report of a surgical case. Am J ClinPathol 101: 531-534.
- Agarwal G, Kar DK (2008) Teratoma of the anterior mediastinum presenting as a cystic neck mass: a case report.J Med Case Rep 2: 23.
- Chen RF, Chang TH, Chang CC, Lee CN (2010) Mediastinalteratoma with pulmonary involvement presenting as massive hemoptysis inpatients. Respir Care 55: 1094-1096.
- Sasaka K, Kurihara Y, Nakajima Y, Seto Y, Endo I, et al. (1998) Spontaneous rupture: a complication of benign mature teratomas of the mediastinum.AJR Am J Roentgenol 170: 323-328.
- Schlumberger HG (1946) Teratoma of the anterior mediastinum in the group of military age; a study of 16 cases, and a review of theories of genesis.Arch Pathol (Chic) 41: 398-444.
- Minami H, Itoyanagi N, Kubota F, Nakamura Y (1994) A case of mediastinal mature teratoma presenting increased serum CA19-9 level. Nihon KyobuGekaGakkaiZasshi 42: 2139-2143.
- Gautam HP (1969) Intrapulmonary malignant teratoma.Am Rev Respir Dis 100: 863-865.
- Yalagachin GH (2013) Anterior mediastinalteratoma- a case report with review of literature.Indian J Surg 75: 182-184.
- Dulmet EM, Macchiarini P, Suc B, Verley JM (1993) Germ cell tumors of the mediastinum. A 30-year experience.Cancer 72: 1894-1901.
- Allen MS (2002) Presentation and management of benign mediastinalteratomas.Chest SurgClin N Am 12: 659-664.
- Lakhoo K, Boyle M, Drake DP (1993) Mediastinalteratomas: review of 15 pediatric cases.J PediatrSurg 28: 1161-1164.