Keywords
Maxillectomy defects; Cheek defects; Anterolateral thigh flap; Titanium mesh; Reconstruction
Introduction
Maxillary defects after tumor resection can lead to the creation of large oronasal and oromaxillary fistulas; loss of lip, cheek, and eye support; loss of midface projection and significant tooth-bearing segments; and impairment of deglutition and speech [1,2]. In addition, most maxillary defects are composite in nature, and they often require skin coverage, bony support, and mucosal lining for reconstruction. So, Maxillary and cheek reconstruction is one of the most challenging tasks for surgeons. Reconstruction of these defects should not only aim at filling in the defect but also include restoration of oronasal functions as well as facial contours [3]. In the reconstruction of maxillary defects, the following goals must be met:
1. Obliteration of the defect.
2. Restoration of essential functions of the midface.
3. Adequate structural support to the midfacial units.
4. Aesthetic reconstruction of the external features [4].
There are many choices for maxillary reconstruction, such as maxillary prostheses, local and regional pedicled flaps with and without bone grafts [5], and titanium mesh(TM) [6]. Many types of tissue flaps have been used for maxillary reconstruction: fibular osteocutaneous flap [7,8] radial forearm flap [9], scapular flap [10], rectus abdominis flap [11], Anterolateral Thigh Flap (ALT) [11,12] and iliac crest flaps [13].
When the patients from a Low Resource Region [LRR], where cancer prevention and control were limited in terms of quantity, quality, and accessibility, came to our hospital, the margin of tumour invasion frequently included the maxillary and the skin of the cheek. So, we used a titanium mesh plate with a folded ALT for maxillary and cheek reconstruction after tumor resection. The combination of titanium mesh and folded ALT is a feasible and acceptable choice. This report introduces our experience treating 16 patients who underwent partial maxillectomy by this method.
Patients and Methods
Our research was approved by the institutional review board of Sun Yat-Sen University. We have read the Helsinki Declaration and have followed the guidelines in this investigation.
Patient characteristics
From October 2010 to May 2013, 16 patients underwent maxillary reconstruction with titanium mesh and folded anterolateral thigh flap after maxilla tumor resection at Sun Yat-Sen University Cancer Center. Data concerning the patient group are summarized in (Table 1). The patients were 2 female and 14 male with ages ranging from 20 to 76 years (mean, 46.5 years). Diagnoses included primary squamous cell carcinoma of the maxillary sinus in 6 cases, osteosarcoma of the maxilla in 3, adenoid cystic carcinoma of the maxillary sinus in 2, adenoid cystic carcinoma of the palate in 1, fibrous sarcoma of the middle face in 2 and Low-grade myofibrosarcoma of the maxillary sinus in 2. In 2 patients, the floor of the orbit was included in the resection and was reconstructed with titanium mesh.
| No. |
Sex |
 Age(years) |
Diagnosis |
DefectType/side |
Postoperativeradiotherapy |
Hospitalstay(days) |
| 1 |
M |
59 |
FS/T3N0M0 |
IIIa/L |
N |
17 |
| 2 |
M |
44 |
ACC/T3N0M1 |
IIa/L |
N |
14 |
| 3 |
M |
37 |
SCC/T4N0M0 |
IIIa/L |
Y |
16 |
| 4 |
M |
45 |
OS/ |
IIIa/R |
Y |
14 |
| 5 |
M |
48 |
LGMS/T2N0M0 |
IIIa/R |
N |
18 |
| 6 |
M |
62 |
ACC/ |
IIa/L |
Y |
20 |
| 7 |
M |
76 |
SCC/ |
IIIa/R |
Y |
24 |
| 8 |
M |
20 |
OS/ |
IIIa/L |
Y |
12 |
| 9 |
F |
34 |
SCC/T3N0M0 |
IIIa/L |
N |
15 |
| 10 |
M |
50 |
SCC/T4N0M0 |
IIIa/R |
N |
19 |
| 11 |
M |
38 |
ACC/ |
IIIa/R |
Y |
18 |
| 12 |
F |
45 |
LGMS/T3N0M0 |
IIIa/L |
Y |
16 |
| 13 |
M |
60 |
SCC/T3N0M0 |
IIa/L |
Y |
17 |
| 14 |
M |
36 |
OS/T3N0M0 |
IIIa/L |
Y |
14 |
| 15 |
M |
47 |
FS/T4N0M0 |
IIa/L |
N |
15 |
| 16 |
M |
44 |
SCC/T3N0M0 |
IIIa/R |
N |
18 |
FS:Fibrous Sarcoma; ACC: Adenoid Cystic Carcinoma;SCC: Squamous Cell Carcinoma; OS:Osteosarcoma;LGMS:Low-Grade Myofibrosarcoma
Table 1: NPS assessment scores for Mr. Rossi compared to the AD control group.
The classification of hard tissue defects, modified from Brown’s classification for maxillectomy defects [14], was as follows.
Class I: maxillary defect without defect of antral mucosa.
Class II: maxillary defect including antral mucosa but without involving orbital floor.
Class III: maxillary defect involving orbital floor.
Class IV: maxillary defect including orbital Exenteration.
According to this classification, there were 4 patients of class IIa and 12 patients of class IIIa in the present study (Table 1).
Surgical procedure
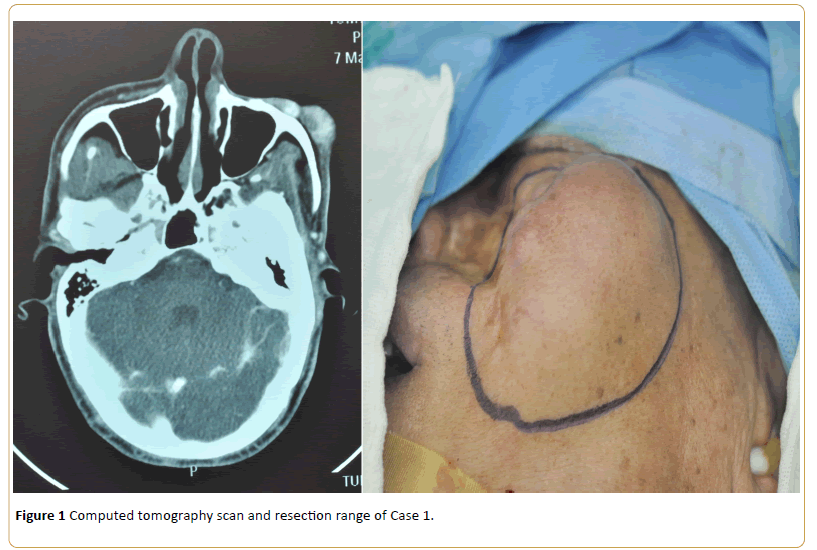
Preoperative CT scanning was performed in all patients. After diagnosis, an individual surgical plan was formulated (Figure 1).
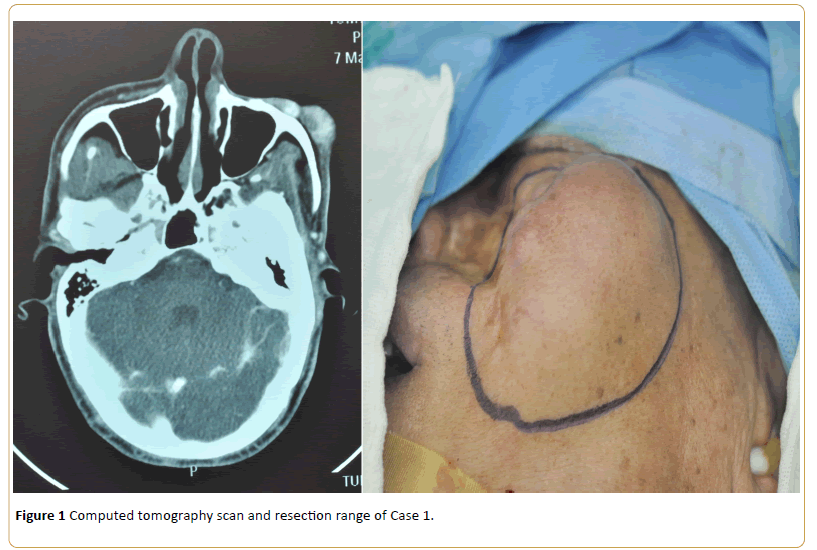
Figure 1: Computed tomography scan and resection range of Case 1.
All of 16 patient’s facial skin was invaded by tumor. We cut off not only the maxilla, but also part of the cheek. While total maxillectomy (including orbital floor resection with preservation of the orbital contents) with the Weber- Fergusson approach was being carried out by the resection team, the ALT flap was harvested by the reconstruction team.
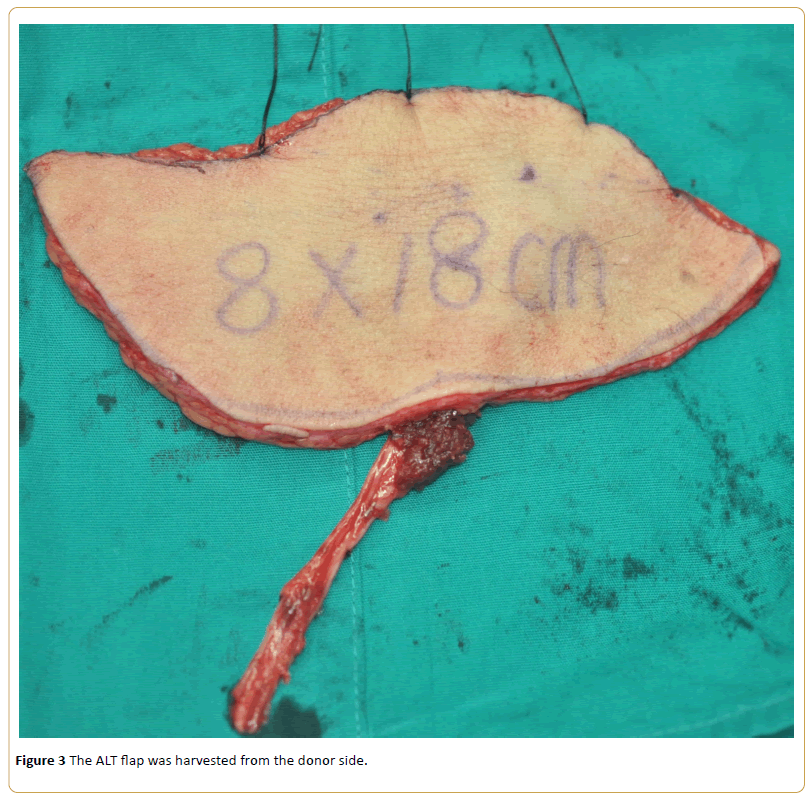
In Case 1, the excision extension concluded unilateral nasal bone, orbital floor, maxillary, palate and the skin of the cheek. After the resection of orbital floor, one arc titanium mesh was fixed to the residual bone of the obital floor and nasal (Figure 2).
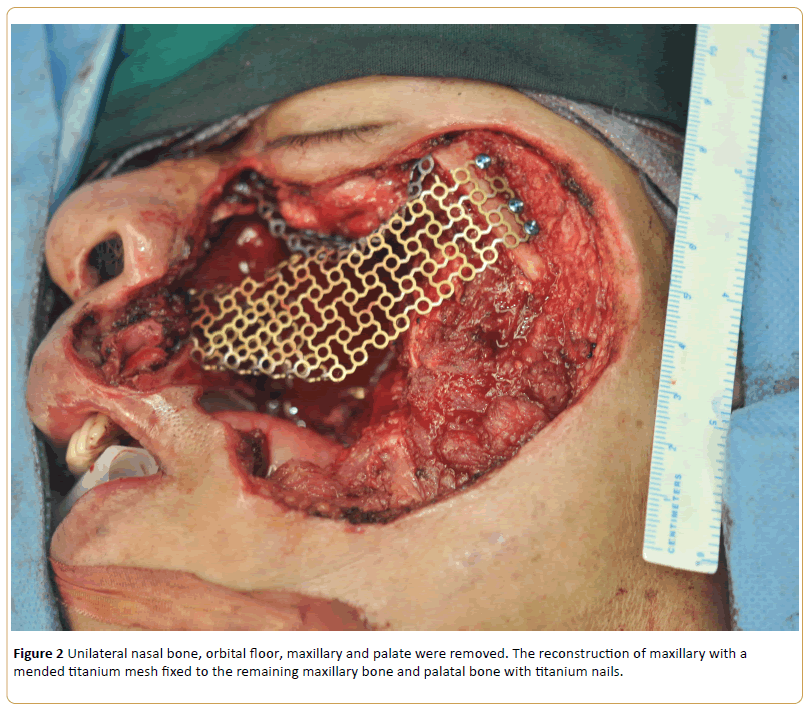
Figure 2: Unilateral nasal bone, orbital floor, maxillary and palate were removed. The reconstruction of maxillary with a mended titanium mesh fixed to the remaining maxillary bone and palatal bone with titanium nails.
Then another titanium mesh was transplanted to the maxillary defect. Before fixation, the titanium mesh was reshaped according to the position and size of the defect to reconstruct the zygoma and the anterior wall of maxillary sinus. Then the titanium mesh was fixed to the remaining maxillary bone and palatal bone with titanium nails (Figure 2). Surgical margins were examined by frozen section.
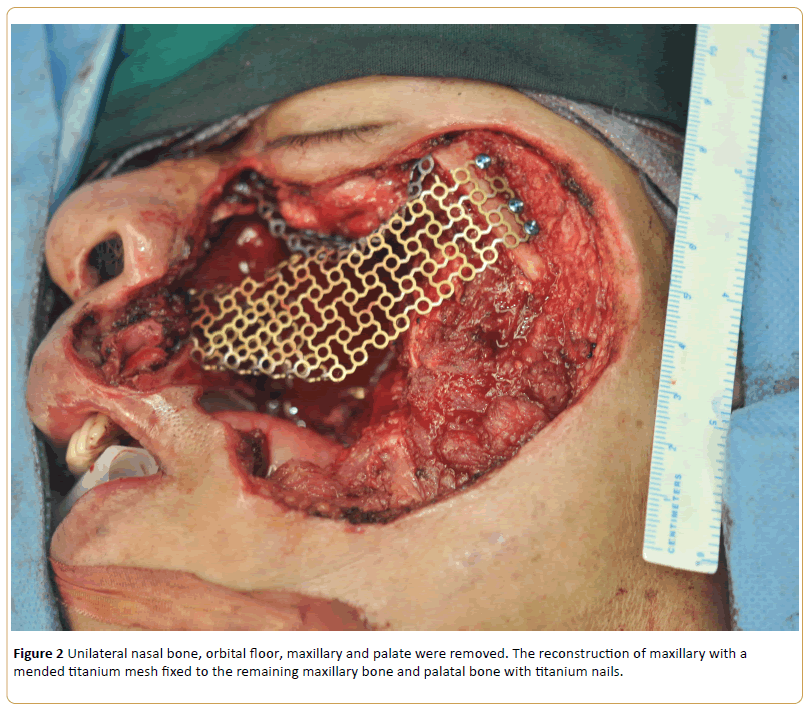
After that, the ALT flap (8×18 cm in size) was harvested from the donor side (Figure 3).
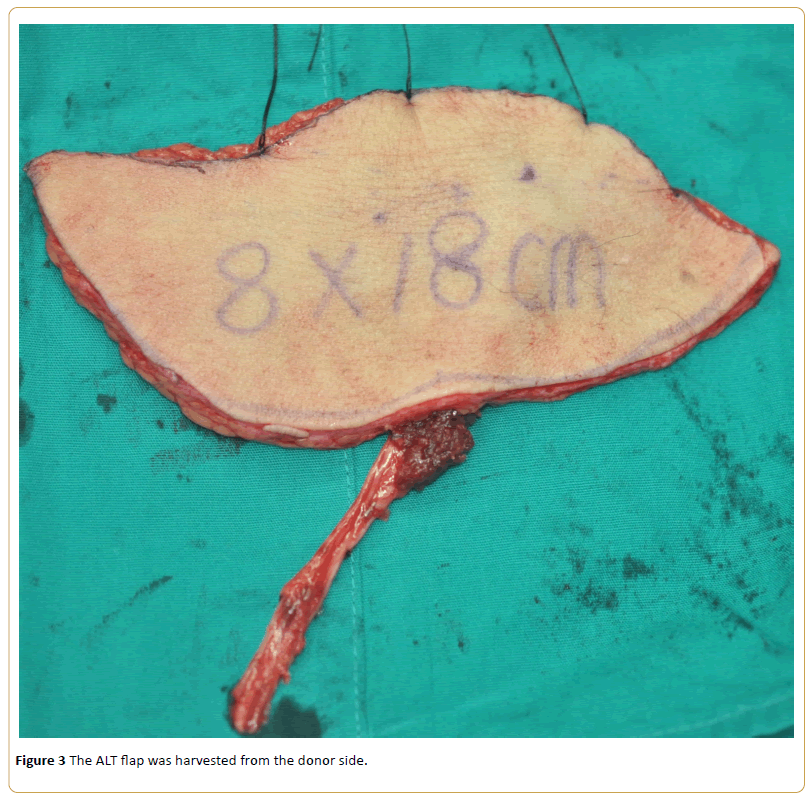
Figure 3: The ALT flap was harvested from the donor side.
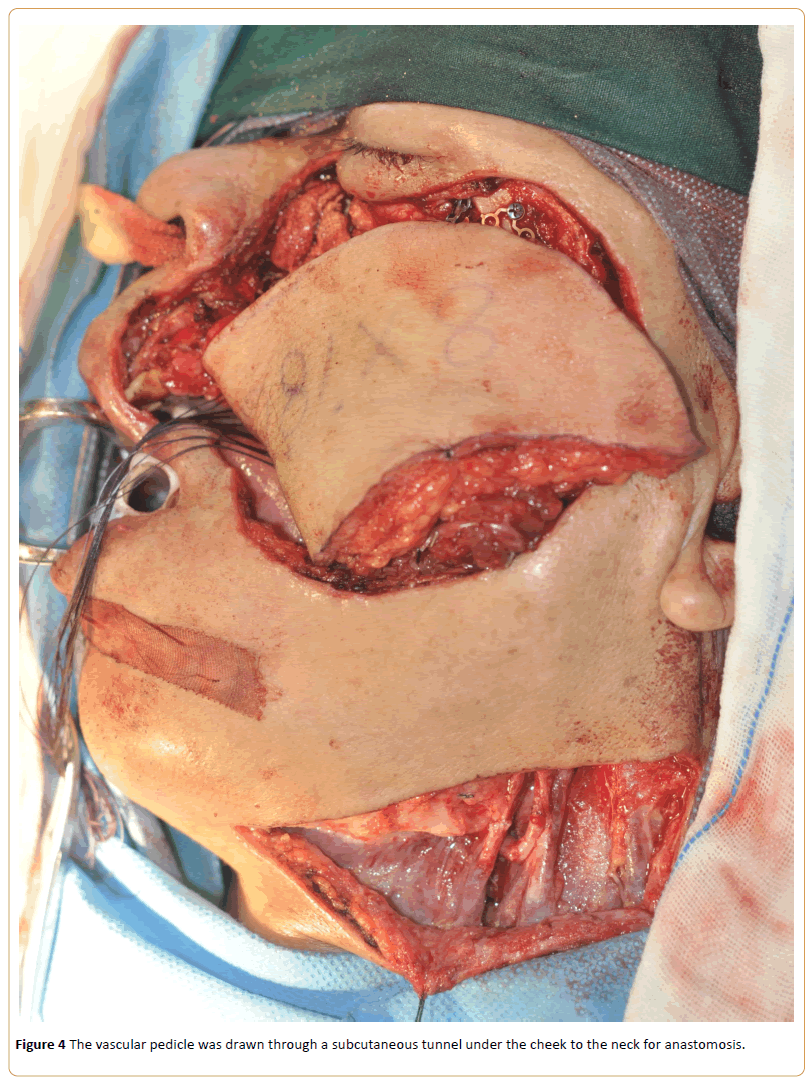
Then, it was transferred to the recipient site and inset into the defect. The vascular pedicle was drawn through a subcutaneous tunnel under the cheek to the neck for anastomosis (Figure 4).
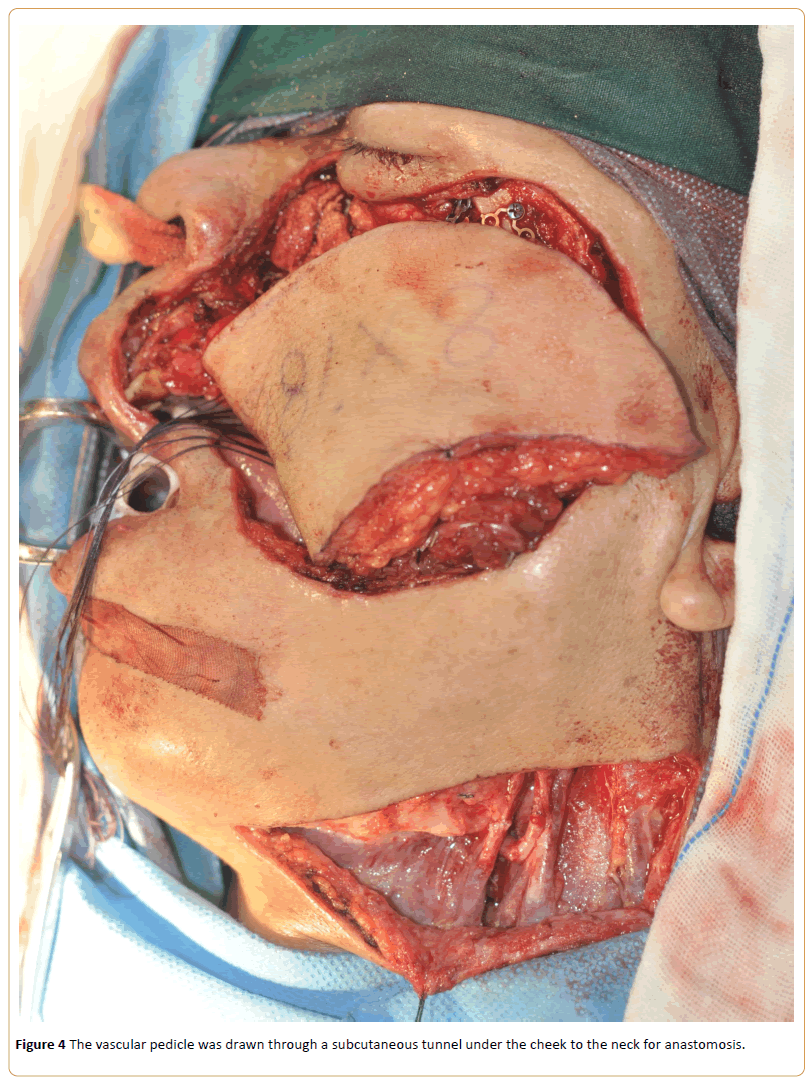
Figure 4: The vascular pedicle was drawn through a subcutaneous tunnel under the cheek to the neck for anastomosis.
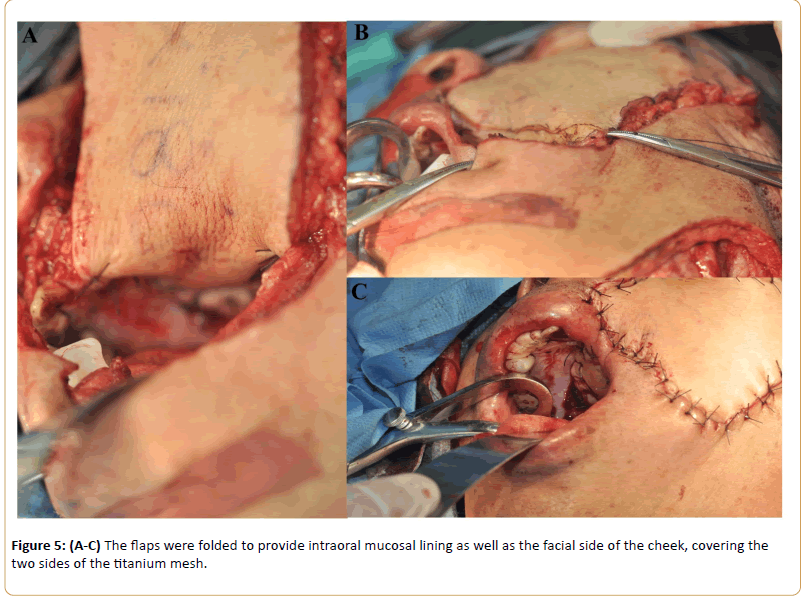
The flaps were folded to provide intraoral mucosal lining as well as the facial side of the cheek, covering the two sides of the titanium mesh. The flap edge closer to perforator was anchored firstly in order to stabilize the perforator and avoid any kinks and compressions. The intervening area was deepithelized and sutured to the inner and outer edge of the defect superiorly (Figure 5). Superior thyroid or facial artery was used as the recipient artery. Internal jugular vein or the facial vein was used as the recipient vein. Several pieces of Gelfoam (Upjohn, Kalamazoo, MI) were packed into the maxillary defect loosely. The donor side defects were sutured directly.
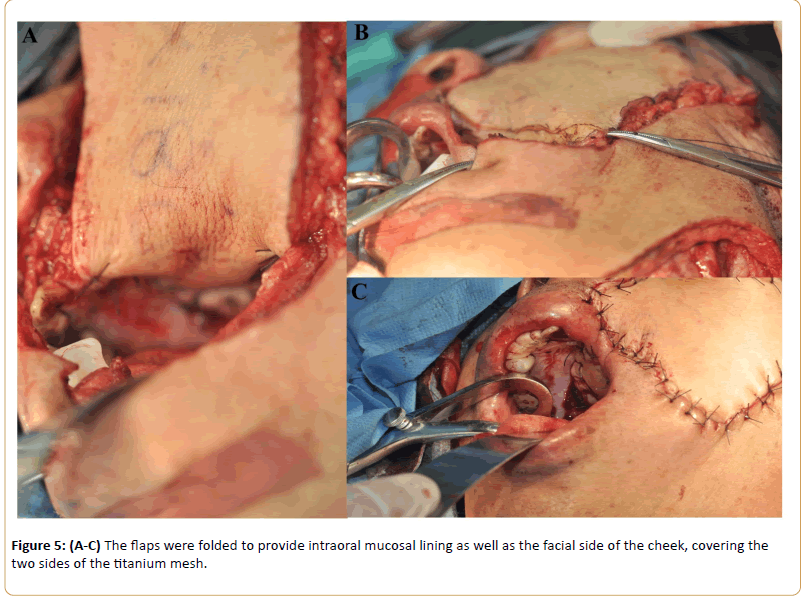
Figure 5: (A-C) The flaps were folded to provide intraoral mucosal lining as well as the facial side of the cheek, covering the two sides of the titanium mesh.
If the facial skin was not invaded by tumor, the flap can be directly used for covering the titanium mesh and repairing the intraoral soft tissue defect. A recipient artery from the neck was used as a superior thyroid artery in 10 cases, facial artery in 6 cases. For the venous anastomosis, we used the facial vein in 9 cases, the internal jugular vein in 7 (Table 2).
| No. |
Flap size (cm) |
Vascular pedicle length(cm) |
Blood loss (ml) |
Arterial anastomosis |
Venous anastomosis |
Surgical time |
| 1 |
8ÃÂâ€â€Â18 |
11 |
800 |
Superior Thyroid Artery |
Internal Jugular Vein |
7h, 30min |
| 2 |
8ÃÂâ€â€Â10 |
10 |
300 |
SuperiorThyroid Artery |
InternalJugular Vein |
9h, 15min |
| 3 |
10ÃÂâ€â€Â10 |
10 |
200 |
Superior Thyroid Artery |
Internal Jugular Vein |
10h, 10min |
| 4 |
6ÃÂâ€â€Â15 |
8 |
400 |
FacialArtery |
Facial Vein |
5h, 30min |
| 5 |
7ÃÂâ€â€Â10 |
8 |
1000 |
Superior Thyroid Artery |
Facial Vein |
9h |
| 6 |
8ÃÂâ€â€Â15 |
15 |
1200 |
FacialArtery |
Facial Vein |
9h, 20min |
| 7 |
9ÃÂâ€â€Â15 |
12 |
1200 |
Superior Thyroid Artery |
Facial Vein |
10h |
| 8 |
7ÃÂâ€â€Â10 |
8 |
1000 |
FacialArtery |
Facial Vein |
11h |
| 9 |
9ÃÂâ€â€Â12 |
10 |
650 |
Superior Thyroid Artery |
Internal Jugular Vein |
8h |
| 10 |
10ÃÂâ€â€Â12 |
12 |
550 |
Superior Thyroid Artery |
Facial Vein |
7h, 30min |
| 11 |
8ÃÂâ€â€Â10 |
9 |
800 |
FacialArtery |
Facial Vein |
6h, 50min |
| 12 |
7ÃÂâ€â€Â12 |
10 |
600 |
FacialArtery |
Internal Jugular Vein |
7h, 40min |
| 13 |
10ÃÂâ€â€Â10 |
8 |
800 |
FacialArtery |
Facial Vein |
8h |
| 14 |
10ÃÂâ€â€Â12 |
10 |
600 |
Superior Thyroid Artery |
Internal Jugular Vein |
7h |
| 15 |
8ÃÂâ€â€Â12 |
10 |
1000 |
Superior Thyroid Artery |
Internal Jugular Vein |
8h, 30min |
| 16 |
9ÃÂâ€â€Â12 |
9 |
700 |
Superior Thyroid Artery |
Facial Vein |
8h, 20min |
Table 2: Surgical characteristics of patients(STA: Superior Thyroid Artery; FA: Facial Artery; IJV:Internal Jugular Vein; FV: Facial Vein).
Follow up
Patients were followed up regularly, every two weeks for one month, every month for three months and then every three months for two years. The duration of follow up ranged from 24 to 48 months (mean duration, 36 months). The patients were followed up to observe the free flap survival, postoperative oral functions, and surgical complications. We will continue to follow up these patients to observe whether complications occurred.
Results
The operative procedure was successfully completed in all patients, with no intra-operative or immediate post-operative complications reported. Except in one patient who developed flap necrosis, all other flaps survived. For the patient with a flap loss, we removed the necrotic tissue and used another ALT flap to fix the defects. No oronasal communication or swallowing impairments developed in any patient.
Nine of 16 patients received postoperative radiotherapy, and other patients refused because of economic problems or inconvenience. During the follow-up period, tumor recurrence was not found in all cases. No exposure of titanium mesh was observed. The final facial appearance was considered acceptable in all cases, for example in Case 1 (Figure 6), with no major complications related to the titanium mesh implant. There were minor enophthalmos and ectropion in the 2 patients who had defects with the orbital floor included, for example in Case 1.

Figure 6: Postoperative facial appearance of Case 1 two years later.
Discussion
In Case 1, the defects of the orbital floor were also reconstructed. But, what we focused on is maxillary and check reconstruction. So, the reconstruction of the orbital floor may be imperfect.
Variety of maxillary reconstruction methods has been reported. However, the reconstruction of maxillectomy defects and the through and through cheek defects using titanium mesh and folded free anterolateral thigh flap has been rarely reported.
The results of this study demonstrate that our method is reliable and satisfactory. The patients could resume a normal oral diet and had clear pronunciation after reconstructive surgery.
The choice of maxillary reconstructive technique depends on the extent of tissue loss and the location of the defect [2]. Using titanium mesh for the reconstruction of maxillary was originally described by Tideman [15] in 1993. Titanium mesh has now become probably the most popular material for maxillary reconstruction worldwide. Compared with Titanium mesh, bone and cartilage frequently used in the autologous reconstruction share common disadvantages like donor graft site morbidity, variable resorption rate, limited quantity, longer operative time, and difficulty in molding into the desired shape, but they all have great resistance to infection, no rejection, and give good structural support.
The principal advantages of titanium for reconstructive surgery are that it is chemically inert and not affected by soft tissues, it provokes little foreign-body or hypersensitivity reaction, it is easy to trim and mold, and it is capable of resisting mechanical strains in thin sections and of producing less artifacts on computed tomography [16]. There is a potential risk of infection and exposure after reconstruction. But, as reported, the rates of minor and major complications did not differ significantly between patients receiving titanium mesh and those receiving vascularized bone [12]. The primary goal of reconstruction after malignant tumor extirpation is different from other types of reconstruction because it is curing the malignancy rather than reconstruction. So, using titanium mesh for reconstruction gives a guarantee of sufficient resection range.
Except these, Titanium mesh implantation for skeletal reconstruction after maxillectomy avoids the need for bone grafting and may be especially beneficial in fragile or aged Patients [11]. Titanium mesh is also a satisfactory choice of the reconstruction of orbital floor. Hashikawa et,al. [16] indicated that using titanium mesh achieved long-lasting, adequate eye position without functional diplopia, and the titanium mesh implant maintained a proper shape and position as an orbital wall without exposing the skin surface or the oral cavity.
The anterolateral thigh flap used for intraoral and facial reconstruction is another crucial and indispensible part of this method. More recently, different kinds of vascularized free flaps are applied to maxillary reconstruction. We prefer to choose anterolateral thigh flap which is thought to be a feasible method in the reconstruction of maxillary defects. Compared with anterolateral thigh flap, the main disadvantage of the iliac crest osteocutaneous flap is that the skin island of it is too bulky for intraoral reconstruction and the pedicle is relatively short. The radial forearm flap leaves behind a conspicuous aesthetic deformity in the forearm, requires the skin graft and sacrifices the major artery of the forearm which may have some potential donor site morbidity [17]. For the fibula osteoseptocutaneous flap, the donor site complications are a main disadvantage. In the literature, the donor site complications and morbidity of this flap have been reported to be from 27% to 60% [18]. The scapular osteocutaneous flap is difficult for a double team to work during flap harvesting for the special positioning.
The advantages of the anterolateral thigh flap include: (1) the ALT flap can be folded to reconstruct the intraoral and facial defects at the same time; (2) the procedure for the ALT flap harvest is simple and this flap has a long vascular pedicle; (3) the donor site can be closed immediately, leaving only a linear scar that is inconspicuous with normal clothing, and no functional defect is left behind. Although ALT flaps have variable vascular anatomical basis, at least one perforating branch artery can be found by searching carefully at the correct scope. Then, the main vessel was sought retrorsely from the branch. 95% patients’ ALT flap was successfully harvest by using this method. However, using softtissue flaps alone does not provide bony reconstruction of maxillary defects or structural support. Long-term results may be poor because of muscular atrophy and gravity [19].
So, the reason why we unite titanium mesh with folded anterolateral thigh flap for the maxillary and the through and through cheek defects reconstruction is that combining both materials promotes the advantages that each one offers individually while, at the same time, cover their own deficiencies. The procedure of this method is easy for surgeons to implement. It perfectly and effectively reproduces maxillary contours thus restoring maxillary volume. This combination leads to reduced operative time and an improvement in functional and aesthetic outcomes of post-traumatic maxillary reconstruction. In addition, it is also convenient to detect local recurrence and does not affect postoperative radiotherapy.
In China, this low cost method might be suitable for the patients from a low resource region.
So, even if maxillary malignancies have a poor prognosis, we must attempt to perform reconstructive surgery that is less invasive and more reliable because a short hospital stay and fewer sequelae may improve the quality of the patients’ remaining life [16].
We achieved a low rate of complications and a high rate of ALT flap survival in these patients. Maybe three year follow-up is short for the patients with post operation radiotherapy who haven't had sufficient time for anticipated complications. We will continue to follow up these patients to observe whether complications occurred.
The limitations of the method used here should also be emphasized. Firstly, one problem is facial deformity, despite the degree of deformity being acceptable for most patients in our series. Secondly, the risk of infection or exposure of the mesh still exists. Thirdly, one drawback of this method is unsuitability for placement of osseointegrated implants.
Conclusion
Reconstruction of maxillectomy defects and the through and through cheek defects using titanium mesh in combination with folded free anterolateral thigh flap is a feasible and acceptable option with a high success rate, a low complication rate, excellent postoperative cosmesis, and well-accepted function.
9957
References
- Triana RJ Jr, Uglesic V, Virag M (2000) Microvascular free flapreconstructive options in patients with partial and total maxillectomydefects. Arch Facial PlastSurg 2: 91-101.
- Futran ND, Wadsworth JT, Villaret D, Farwell DG (2002) Midfacereconstruction with fibula free flap. Arch Otolaryngol HeadNeck Surg 128: 161-166.
- LiuYM, ChenGF, YanJL (2006)Functional reconstruction ofmaxilla with pedicledbuccal fatpad flap, prefabricated titaniummesh and autologous bonegrafts.Int J Oral MaxillofacSurg 35: 1108-1113.
- Muzaffar AR, Adams WP, Hartog JM (1999) Maxillaryreconstruction:Functional and aesthetic considerations. PlasticReconstrSurg 104: 2172-2184.
- Arce K (2007) Buccal fat pad in maxillary reconstruction. Atlas OralMaxillofacSurgClin North Am 15: 23-32.
- Schubert W, Gear AJ, Lee C (2002) Incorporation of titaniummesh in orbital and midface reconstruction. PlastReconstrSurg 110: 1022-1030.
- Yazar S, Cheng MH, Wei FC, Hao SP, Chang KP (2006) Osteomyocutaneousperoneal artery perforator flap for reconstructionof composite maxillary defects. Head Neck 28: 297-304.
- Rodriguez ED, Bluebond-Langer R, Park JE, Manson PN (2008) Preservation of contour in periorbital and midfacial craniofacialmicrosurgery: Reconstruction of the soft-tissue elementsand skeletal buttresses. PlastReconstrSurg 121: 1738-1747.
- Sarukawa S, Sakuraba M, Asano T (2007) Immediate maxillaryreconstruction after malignant tumor extirpation. Eur J SurgOncol 33: 518-523.
- Clark JR, Vesely M, Gilbert R (2008) Scapular angle osteomyogenousflap in postmaxillectomy reconstruction: Defect, reconstruction,shoulder function and harvest technique. HeadNeck 30: 10-20.
- Nakayama B,Hasegawa Y, Hyodo I (2004) Reconstructionusing a three-dimensional orbitozygomatic skeletal model oftitanium mesh plate and soft-tissue free flap transfer followingtotal maxillectomy. PlastReconstrSurg 114: 631-639.
- Sarukawa S, Sakuraba M, Asano T (2007) Immediate maxillaryreconstruction after malignant tumor extirpation. Eur J SurgOncol 33: 518-523.
- Maranzano M,Atzei A (2007) The versatility of vascularized iliaccrest with internal oblique muscle flap for composite uppermaxillary reconstruction. Microsurgery 27: 37-42.
- Brown JS, Rogers SN, McNally DN, Boyle M (2000) A modified classification forthe maxillectomy defect. HeadNeck22: 17-26.
- Tideman H, Sammam N, Cheung LK (1993) Immediate reconstructionfollowing maxillectomy:a new method.Int J Oral MaxillofacSurg 22: 221-225.
- Hashikawa K, Tahara S, Ishida H (2006) Simple reconstruction withtitanium mesh and radial forearm flap after globe-sparing total maxillectomy: A 5-year follow-up study.PlastReconstrSurg 117: 963-967.
- Liu ZM, Wu D, Liu XK(2013)Reconstruction through cheek defects with folded free anterolateral thigh flaps.J Oral MaxillofacSurg 71:960-964.
- Bodde EW, de Visser E, Duysens JE, Hartman EH (2003) Donor-sitemorbidity after free vascularized autogenous fibular transfer:subjective and quantitative analyses.PlastReconstrSurg111: 2237-2242.
- Novak CB, Lipa JE, Noria S, Allison K, Neligan PC, et al. (2007) Comparison of anterolateral thigh and radial forearmfree flap donor site morbidity. Microsurgery 27: 651-654.