Moara Rodrig ues Costa1, Michelly Farias Rocha3, Gabriela Carvalho Jurema Santos3, Wenicios Ferreira Chaves4, Luana Olegário da Silva2, Regina Maria Chaves Escorel Costa7, Hortência Freitas de França8, Caio Ferreira Santos3, Thaliane Mayara Pessoa dos Prazeres6, Rafael dos Santos Henrique5 and Matheus Santos de Sousa Fernandes1*
1Neuropsyquiatry and Behavior Science Postgraduate Program, Federal University of Pernambuco -UFPE, Recife, PE, Brazil
2Nutrition Postgraduate Program, University of Pernambuco – UFPE, Recife, PE, Brazil
3Reference Center in Social Assistance, Vassoural, Caruaru, Pernambuco, Brazil
4Metabolism and Sport Science and Nutrition Postgraduate Program, Universidade Estadual de Campinas –Unicamp, Limeira, SP, Brazil
5Department of Physical Education, Federal University of Pernambuco, Recife, Brazil
6Higher School of Physical Education, University of Pernambuco, Recife, Brazil
7Graduate in Nutrition, University of Pernambuco – UFPE, Recife, PE, Brazil
8Graduate in Nutrition, Universidade Salgado Filho, Brazil
- *Corresponding Author:
- Matheus Santos de Sousa Fernandes
Federal University of Pernambuco- Physical Education Department
Recife, PE, Brazil
Tel: +5581996395116
E-mail: matheus.sfernandes@ufpe
Received Date: August 10, 2020; Accepted Date: August 25, 2020; Published Date: August 31, 2020
Citation: Costa MR, Rocha MF, Santos GCJ, Chaves WF, Silva LO, et al. (2020) Mental Health and COVID-19 Infection: Systematic Review in Human Cross-Sectional Studies. Health Sci J. Sp. Iss 1: 009.
DOI: 10.36648/1791-809X.S1.009
Keywords
Coronavirus; Depression; Anxiety; Stress; Acute infections
Introduction
The outbreak of the new coronavirus (COVID-19) is the most recent global emergency declared by the World Health Organization (WHO) [1-26]. This occurs after infection by the SARS-CoV-2 virus, which has a primary vector still uncertain [23]. Similar to other outbreaks caused by the coronavirus group, such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS), signs of infection appear after an average incubation period of five days [13,27-29]. In severe cases, pneumonia, acute respiratory distress syndrome, multiple organ failure and thousands of deaths around the world are observed [3].
In addition to changes related to physical health, uncertainty, low predictability and the imminent risk of transmission and mortality by COVID-19 has caused changes in mental health [10]. Individuals who have family members belonging to the risk group, as well as frontline health professionals are more susceptible to the development of mental health complications [5,8]. Some studies have shown that the threat and alert state against COVID-19 has triggered negative emotions such as acute stress, anxiety, social disgust, dissatisfaction with life, and depression [24]
These long-term behavioral and emotional changes can cause psychological consequences during the COVID-19 pandemic that could compromise the state of health and quality of life. However it is not clear the impacts of the COVID-19 mental health scenario [11]. Thus, the aim of this systematic review was to analyze the main impacts caused by the current COVID-19 pandemic scenario on mental health outcomes.
Methods and Materials
This systematic review was performed following the guideline of the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [16]. The review protocol was not previously registered.
Search strategy
The search for studies in the scientific literature began in January 2020 to March 2020, using the following databases: PubMed (Medline), Lilacs, and Virtual Health Library (BVS). The following terms: “Nervousness or Social Anxiety or Anxieties, Social or Anxiety, Social or Social Anxieties or Anxiety and Depressions or Depressive Symptoms or Depressive Symptom or Symptom, Depressive or Symptoms, Depressive or Emotional Depression or Depression, Emotional or Depressions, Emotional or Emotional Depressions and Health, Mental or Mental Hygiene or Hygiene, Mental and COVID 19 or Coronavirus, through Medical Subject Headings (MESH), which consists of a nomenclature based on the indexing of articles in the field of health sciences. Articles were included if they fulfilled the following PICOS criteria [20] (Population: COVID-19 patients, Interventions/exposure: COVID-19/coronavirus; Comparisons: no COVID-19/coronavirus patients, Outcomes: mental health Study Design: Cross-sectional studies). Reference lists of all included studies were also reviewed for potentially eligible articles
Eligibility and inclusion criteria
Two reviewers selected the articles according to the following inclusion criteria: 1) written in English, 2) between the years 2015 and 2020, involving studies 3) COVID-19/coronavirus, 4) Mental health, performed in human’s studies. Articles were included if they fulfilled the following PICOS criteria (Participants, Interventions, Comparisons, Outcomes). In the next step of study made the comparison their findings at the end, searched the database, using the terms, and evaluated titles and abstracts in agreement to the eligibility criteria. The abstracts were submitted to second phase of analysis, in which two other independent researchers reviewed the articles completely and, by consensus, excluded articles that did not meet the criteria. Articles considered eligible, data were extracted regarding characteristics of the sample, methodology, and the main results found. There were triple combinations of these terms during the searches, being chosen as inclusion criteria. Were excluded: Reviews, opinions, letters, other languages, and animal’s studies.
Extract data
The reviewers extracted the data studies on pre-established database. The third reviewer was consulted when occurs differences between reviewers. The data were described into a table according to its outcome, being mental health outcomes.
Quality assessment
The included studies were analyzed using a methodological quality assessment (MQA) adapted from the Downs and Black Quality Index [4]. This version consists of eight objective questions (Table 1). Each study was allocated a “1” for “yes” or a “0” for “no” for each question, and responses were summed for a total of eight. A total score ≥6 indicated a high-quality study, a total score of 3-5 indicated moderate quality, and a score<3 indicated low quality. Our analysis of the quality of the articles included demonstrated that all of them had a moderate quality (score=5).
Table 1 Methodological quality assessment scores of the included studies.
| Study |
Questions |
|
|
|
|
|
|
|
Total |
| |
1. Clear objective |
2. Sample Description |
3. Interventions of interest clearly described |
4. Methods to assess clearly described |
5. Adverse events |
6. Sample loss |
7. Results Confounders |
8. Statistical Power |
|
| Gao et al [4] |
1 |
1 |
1 |
1 |
0 |
1 |
0 |
0 |
5 |
| Huang [9] |
1 |
1 |
1 |
1 |
0 |
1 |
0 |
0 |
5 |
| Lai et al [12] |
1 |
1 |
1 |
1 |
0 |
1 |
0 |
0 |
5 |
| Li et al [14] |
1 |
1 |
1 |
1 |
0 |
1 |
0 |
0 |
5 |
| Wang et al [24] |
1 |
1 |
1 |
1 |
0 |
1 |
0 |
0 |
5 |
| Zhang [30] |
1 |
1 |
1 |
1 |
0 |
1 |
0 |
0 |
5 |
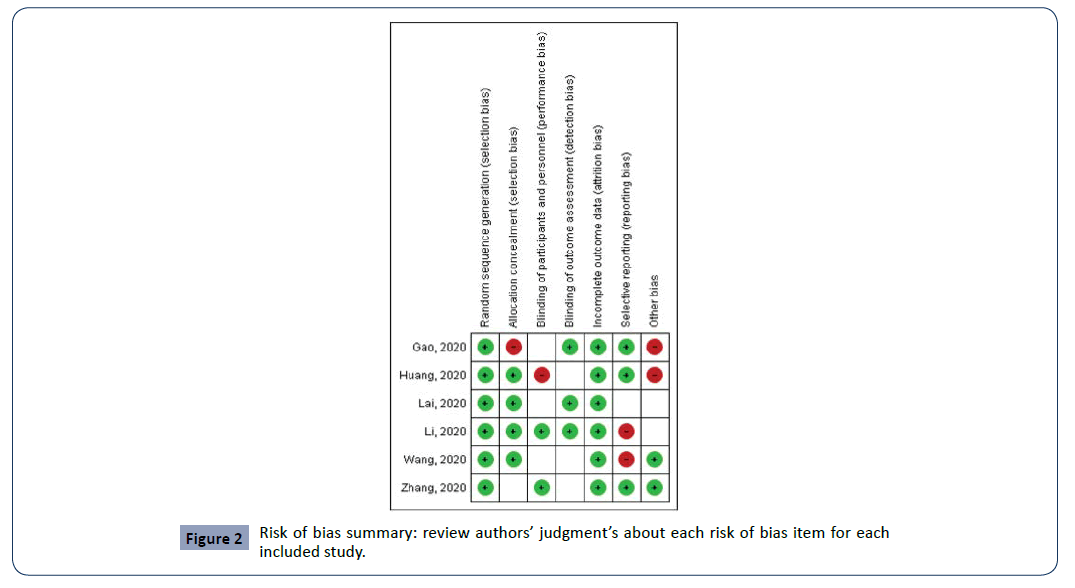
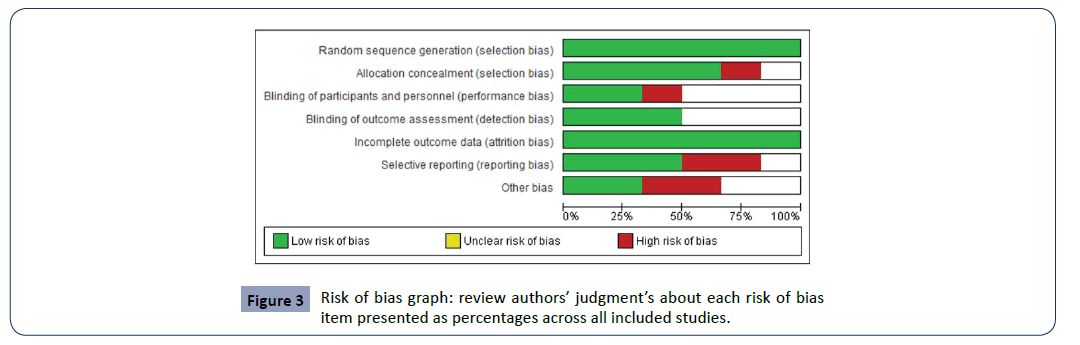
Risk of bias analysis
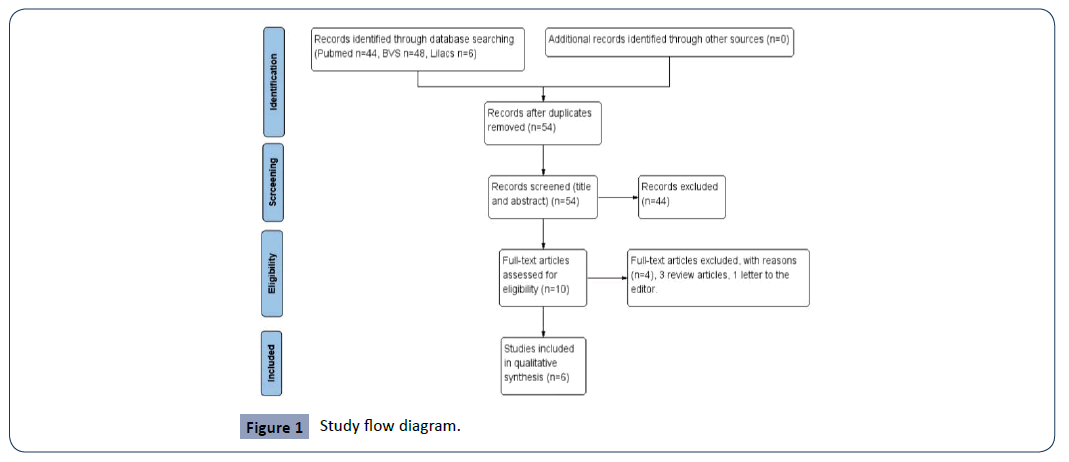
The risk of bias was established through of a critical analysis of authors using seven criteria of a methodological judgment of included studies supplied by software Revman 5.3.0 program the Cochrane Handbook [2], developed for systematic reviews and available for free download (http//ims.cochrane.org/revman/download) were used. Among the criteria that structure the bias assessment are (1) Random sequence generation, (2) Allocation concealment, (3) Blinding of participants and personnel, (4) Blinding of outcome assessment, (5) Incomplete outcome data, (6) Selective reporting and (7) Other bias. The criteria for risk of bias are described in Figure 2 and 3 (Figures 1-3).
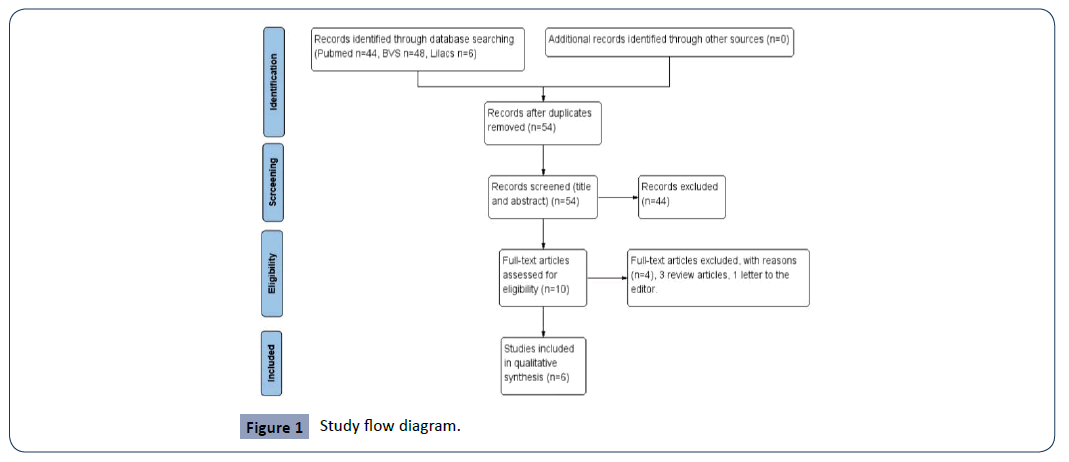
Figure 1: Study flow diagram.
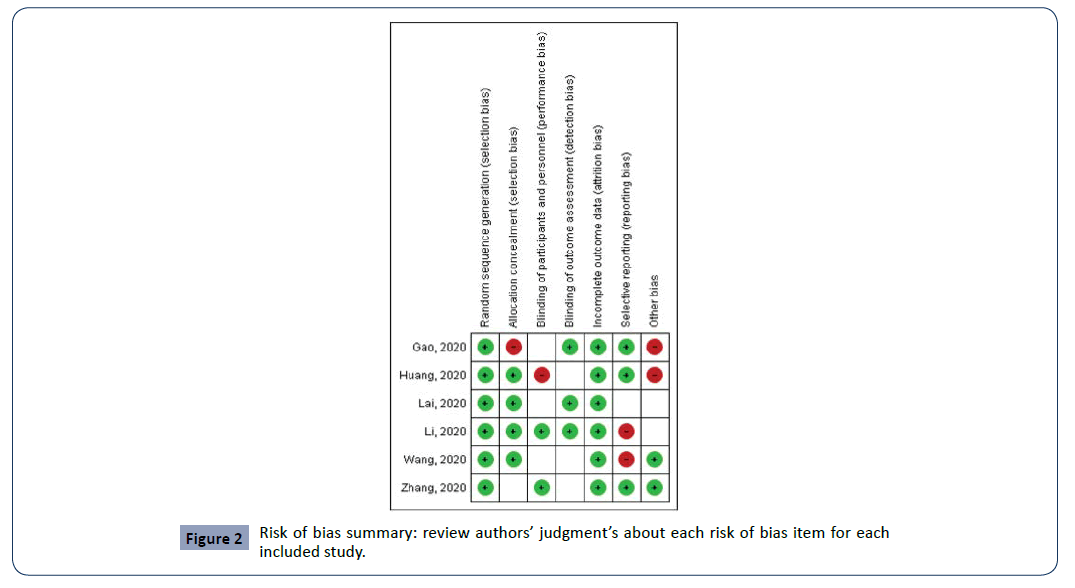
Figure 2: Risk of bias summary: review authors’ judgment’s about each risk of bias item for each included study.
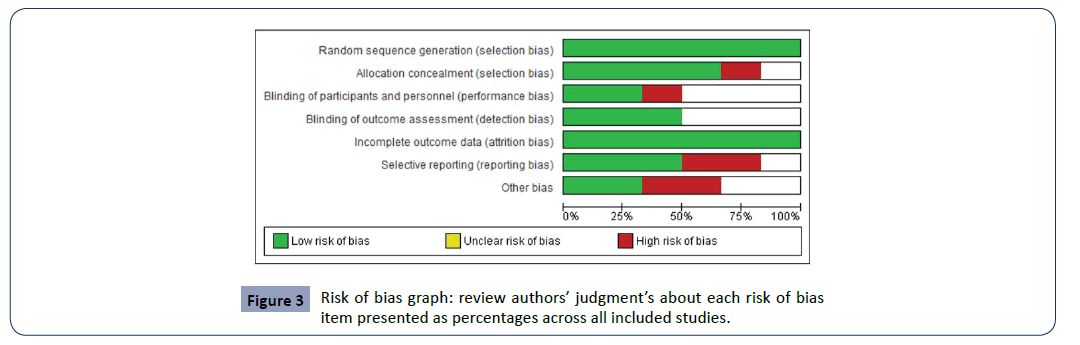
Figure 3: Risk of bias graph: review authors’ judgment’s about each risk of bias item presented as percentages across all included studies.
Results
The flowchart demonstrated the successive steps taken to select studies in present systematic review (Figure 1). We found 98 studies in databases: Pubmed (44), BVS (48) and Lilacs (6). Then, 44 studies were excluded because they did not meet the inclusion criteria. Next, 10 articles remained, of which 3 review articles were excluded and, 1 letter to the editor. At the end of process, 6 studies were included. Table 2 shows the summary of these studies in the mental health outcomes in the COVID-19 period. All six cross-sectional studies were carried out in the Chinese population, with ages ranging from 9 to 59 years of age.
Table 2 Description of the main methodological protocols and results.
| Author, year |
Country |
Objective |
Type of Study |
Sample description |
Study Design |
Mental health Manisfestations |
| Gao et al [6] |
China |
The current study aims to describe the prevalence and distribution of two major mental disorders (anxiety and depression) among the Chinese population and examine their associations with social media exposure during COVID-19 outbreak. |
Cross sectional |
4872 Chinese participants aged 18 years or over from 31 provinces and autonomous regions were evaluated. |
Demographics and (SME) characteristics were evaluated, in addition, depression was assessed by The Chinese version of (WHO-5) and anxiety was assessed by the Chinese version of (GAD-7). |
A prevalence of depression, anxiety, and a (CDA) was found to be 48.3% (95% CI: 46.9% -49.7%), 22.6% (95% CI: 21.4% -23.8%) and 19.4% (95% CI:18.3% -20.6%) during COVID-19 out broke in Wuhan, China. After controlling for covariates, frequently SME was positively associated with high odds of anxiety (OR=1.72, 95% CI: 1.31–2.26) and CDA (OR=1.91, 95% CI: 1.52–2.41) compared with less SME. |
| Huang [9] |
China |
To assess the mental health burden of the public during the COVID-19 outbreak and to identify the high-risk group. |
Cross sectional |
7,236 Chinese men and women participated in the study [3,284 (45.4%) male and 3,952 (54.6%) female] and the average age (standard deviation) of the participants was 35.3 ± 5, 6 years. They were divided into two groups by age at ≤ 35 years and ≥ 35 years. |
Within the design of the study a web-based approach to data collection avoided any risk of the spread of SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus was used. This web-based survey of the COVID-19 was broadcasted on the Internet through the WeChat public platform and the mainstream media. All Chinese public using WeChat, Weibo, or others. For anxiety symptoms, Chinese version of generalized anxiety disorder-7 (GAD-7) scale, and for depressive symptoms analysis was used CES-D in Chinese version. |
The prevalence of anxiety symptoms, depressive symptoms, and poor sleep quality was 35.1%, 20.1%, and 18.2%, respectively. No statistically significant difference was found in the prevalence of mental health burden by gender (p>0.05). The prevalence of anxiety symptoms and depressive symptoms was significantly higher in participants younger than 35 years than in participants aged 35 years or older (p<0.001). |
| Lai et al [12] |
China |
To assess the magnitude of mental health outcomes and associated factors among health care workers treating patients exposed to COVID-19 in China. |
Cross sectional |
1257 health care workers in 34 hospitals from China. |
From 29 January to 3 February 2020, was compared the interregional differences of mental health outcomes among health care workers in China, samples were stratified by their geographic location (i.e., Wuhan, other regions inside Hubei province, and regions outside Hubei province). Were evaluated a total of 20 hospitals in Wuhan, 7 hospitals in other regions of Hubei province, and 7 hospitals from 7 other provinces with a high incidence of COVID-19 (1 hospital from each province) were included. In total, 34 hospitals were involved. Anxiety symptoms was analyzed through GAD-7 scale, patient health questionnaire, insomnia index, and IES-R for depression state. |
Health care workers reported symptoms of depression (n=634 [50.4%]), anxiety (n=560 [44.6%]), insomnia (n=427 [34.0%]), and distress (n=899 [71.5%]). Nurses, the frontline workers, reported experiencing more severe symptom levels of depression, anxiety, insomnia, and distress (eg, severe depression among physicians vs. nurses: 24 [4.9%] vs. 54 [7.1%];p = .01; severe anxiety between men vs. women: 10 [3.4%] vs. 56 [5.8%]; p = .001; severe insomnia among frontline workers vs. second-line workers: 9 [1.7%] vs. 3 [0.4%]; p < .001; severe distress among workers in Wuhan vs. Hubei outside Wuhan and outside Hubei: 96 [12.6%] vs. 19 [7.2%] among those in Hubei outside Wuhan and 17 [7.2%] among those outside Hubei; p <.001). |
| Li et al [14] |
China |
To explore the impacts of COVID-19 on people’s mental health, to assist policymakers to develop actionable policies, and help clinical practitioners (social workers, psychiatrists, and psychologists) provide timely services to affected populations. |
Cross sectional |
Were analyzed the Weibo posts from 17,865 active Weibo users using the approach of (OER) based on several machine-learning predictive models. Age ranging from 9 to 40.1 years old |
Was calculated the word frequency, scores of emotional indicators (e.g., anxiety, depression, indignation, and Oxford happiness) and cognitive indicators (e.g., social risk judgment and life satisfaction) from the collected data. |
The results showed the increase of negative emotions (e.g., anxiety (p<0.000), depression (p<0.000), and indignation (p<0.000) and sensitivity to social risks increased, while the scores of positive emotions (eg, Oxford happiness) and life satisfaction decreased (p<0.0002), as a result of the COVID-19 pandemic. |
| Wang et al [24] |
China |
To survey the general public in China to better understand their levels of psychological impact, anxiety, depression, and stress during the initial stage of the COVID-19 outbreak. |
Cross sectional |
1210 respondents from 194 cities in China were assessed. The majority of respondents were women (67.3%), aged between 21.4 and 30.8 years (53.1%). |
From 31 January to 2 February 2020, was conducted an online survey using snowball sampling techniques. The online survey collected information on demographic data, physical symptoms in the past 14 days, contact history with COVID-19, knowledge, and concerns about COVID-19, precautionary measures against COVID-19, and additional information required with respect to COVID-19. The psychological impact was assessed by the Impact of Event Scale-Revised (IES-R), and mental health status was assessed by DASS-21. |
Among the individuals evaluated, it was observed that 296 (24.5%) reported minimal psychological impact levels (score<23); 263 (21.7%) rated mild psychological impact (scores 24-32); and 651 (53.8%) reported moderate or severe psychological impact (score>33).
Regarding depression, 167 (13.8%) were considered to suffer from mild depression (score: 10–12); 148 (12.2%) were considered moderate depression (score: 13-20); and 52 (4.3%) were considered to be severe sufferers and extremely severe depression (score: 21-42).
For the anxiety, 91 (7.5%) were considered to have mild anxiety (score: 7-9); 247 (20.4%) were considered to have moderate anxiety (score: 10-14); and 102 (8.4%) were considered suffer from severe and extremely severe anxiety (score: 15–42).
For stress, 292 (24.1%) were considered to suffer from stress (score: 11-18); 66 (5.5%) were considered to have moderate stress (score: 19–26); and 31 (2.6%) were considered to have severe and extremely severe stress (score: 27-42). |
| Zhang [30] |
China |
To investigate the immediate impact of the COVID-19 pandemic on mental health and quality of life among local Chinese residents aged ≥ 18 years in Liaoning Province, mainland China |
Cross sectional |
The study included 263 Chinese participants (106 men and 157 women) with an average age of participants between 18 and 30 years old. |
The study was conducted from January 28, 2020 to February 5, 2020. Participants complete an online sociodemographic questionnaire via WeChat and telephone interviews using a modified and validated questionnaire that investigates the impact of the COVID-19 pandemic on lifestyle changes related to mental health (IER-S). |
A slight stressful impact was observed, with no gender differences [p=0.173]. Only the average intrusive score in men was significantly higher than in women (13.0 vs. 12.3) [P=0.027].
A total of 74.5% of participants reported that they did not experience increased stress at home. There was a significant association between different age groups and some of the responses including feeling horrified due to the COVID-19 pandemic [p=0.002]; Feeling apprehensive due to COVID-19 pandemic [p=0.001]; and feeling helpless due to the COVID-19 pandemic [P=0.049]. |
CDA: Combination of Depression and Anxiety; CES-D: Center for Epidemiology Scale for Depression; CI: Confidence Interval; DASS-21: Depression, Anxiety, and Stress Scale; GAD-7: Generalized Anxiety Disorder scale, IES-R: Impact of Event Scale; OER- Online Ecological Recognition; OR: Odds Ratio; SME: Social Media Exposure;WHO-5: WHO-Five Well-Being Index
Regarding the different manifestations in mental health observed in this COVID-19 pandemic scenario. Five studies demonstrate a higher incidence of depression state and anxiety symptoms [6,9,12,14,24].
In the other hand, two studies [9,12], demonstrated negative effects on sleep quality/insomnia during the COVID-19 scenario. Symptoms related to increased stress [12,24,30], sensitivity to social risks [14], and the sensation of horror were also observed [30]. When stratified by the psychiatric impact, high rates of moderate or severe psychological impact (53.8%) were observed [24].To assess to these different of mental health outcomes and its association with the COVID-19 pandemic, were evaluated by strategies. Gao et al [6] analyzed the current health well-being, through the questionnaire through the Five Well-Being Index (WHO-5) and, anxiety by the generalized anxiety disorder scale (GAD-7), both in the Chinese version.
In addition, Huang et al [9] he also used the GAD-7 scale to assess anxiety symptoms and the Center for Epidemiology Scale for Depression (CES-D) to analyze the depressive state. In this sense, Lai et al [12] also carried out the assessment of anxiety using the GAD-7 scale, insomnia questionnaire, and depression by the Impact of event scale revised (IES-R). Zhang et al [30] they also used IES-R in their respective studies, to analyze others psychological impacts (impact of event, stress, anxiety). Moreover, in the Wang et al [24] assessed mental health status through Depression, Anxiety, and Stress Scale (DASS-21). However, Li et al [14] analyzed the word frequency, scores of emotional indicators (e.g., anxiety, depression, indignation, and Oxford happiness) and cognitive indicators (e.g., social risk judgment and life satisfaction.
Discussion
In the present study, we found that the significant impact of the COVID-19 pandemic on mental health outcomes. So, all included studies carried out a diversified assessment of mental health using financially viable instruments (questionnaires, websites). In this perspective, anxiety and depression were the mental disorders that had a higher incidence in the general population and health professionals [15]. Collaborating with this, studies show that there are several factors (physiological, biochemical, behavioral) that influence the genesis of these two disorders affecting the homeostasis of the human mind [1,21,25,27]. The social isolation needed to stem the progress of the COVID-19 pandemic, can lead to adverse emotional and mental disorders, such as anxiety, depression, stress [7]. These changes occur due to the reduction of neuronal metabolism and neuroplasticity in hippocampus, medial prefrontal cortex, ventral tegmental area, and accumbens nucleus shell, associated with a high rate of chronic diseases and mortality [18,31]. Moreover, hospitalization for treatment of COVID-19 and its complications such as SARS contribute to increased levels of insomnia and stress, causing dysfunctions in the immune system [19].
This is in line with our findings, which demonstrate that exposure to COVID-19 provided increased levels of insomnia, social risk and stress associated with reduced mental health because of the impact of traumatic exposure to the pandemic. In this sense, studies demonstrate that prolonged exposure to stress, provides an increase in the levels of the hormone cortisol, reducing the activity of the components of the immune system (immunoglobulin A, neutrophils, anti-inflammatory cytokines), leading to a greater susceptibility to associated infection [19,22]. However, there is a need for further investigation of the mechanisms associated with mental health and its health outcomes for patients and health professionals affected by the COVID-19 pandemic.
Conclusion
Finally, the COVID-19 pandemic scenario is concluded, directly impacting the quality of mental health of the population and their health professionals. Nevertheless, strategies related to lifestyle (nutrition and physical activity), associated with psychological care can be fundamental to improve the mental health of these individuals.
Funding
Not Applicable
Acknowledgements
The authors thank the Federal University of Pernambuco for their support.
Conflict of interest
The Authors declares that there is no conflict of interest.
30699
References
- Daneshzad E, Keshavarz SA, Qorbani M, Larijani B, Azadbakht L (2020) Association between a low-carbohydrate diet and sleep status, depression, anxiety, and stress score. J Sci Food Agric 100: 2946-2952.
- Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1. 0. The Cochrane Collaboration.
- Desforges M, Le Coupanec A, Dubeau P, Bourgouin A, Lajoie L, et al. (2020) Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses 12: 14.
- Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52: 377-384.
- Fiorillo A, Gorwood P (2020) The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry 63: e32.
- Gao J, Zheng P, Jia Y, Chen H, Mao Y, et al. (2020) Mental health problems and social media exposure during COVID-19 outbreak. PloS one 15: e0231924.
- Garcovich S, Bersani FS, Chiricozzi A, De Simone C (2020) Mass quarantine measures in the time of COVID-19 pandemic: psycho-social implications for chronic skin conditions and a call for qualitative studies. J Eur Acad Dermatol Venereol 34: e293-e294.
- Hamza Shuja K, Aqeel M, Jaffar A, Ahmed A (2020) COVID-19 Pandemic and Impending Global Mental Health Implications. Psychiatr Danub 32: 32-35.
- Huang Y, Zhao N (2020) Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychol Health Med pp: 1-12.
- Jakovljevic M, Bjedov S, Jaksic N, Jakovljevic I (2020) COVID-19 Pandemia and Public and Global Mental Health from the Perspective of Global Health Securit. Psychiatr Danub 32: 6-14.
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R (2002) Emotions, morbidity, and mortality: new perspectives from psychoneuroimmunology. Annu Rev Psychol 53: 83-107.
- Lai J, Ma S, Wang Y, Cai Z, Hu J, et al. (2020) Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA network open 3: e203976-e203976.
- Lee N, Hui D, Wu A, Chan P, Cameron P, et al. (2003) A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 348: 1986-1994.
- Li S, Wang Y, Xue J, Zhao N, Zhu T (2020) The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. I Int J Environ Res Public Health 17: 2032.
- McKenzie EL, Brown PM, Mak AS, Chamberlain P (2017) 'Old and ill': death anxiety and coping strategies influencing health professionals' well-being and dementia care. Aging Ment Health 21: 634-641.
- Moher, D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151: 264-269.
- Neto MLR, Almeida HG, Esmeraldo JD, Nobre CB, Pinheiro WR, et al. (2020) When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res 288: 112972.
- Pati S, Sood A, Mukhopadhyay S, Vaidya VA (2018) Acute pharmacogenetic activation of medial prefrontal cortex excitatory neurons regulates anxiety-like behaviour. J Biosci 43: 85-95.
- Pondeljak N, Lugovic-Mihic L (2020) Stress-Induced Interaction of Skin Immune Cells, Hormones, and Neurotransmitters. Clin Ther 42: 757-770.
- Stone PW (2002) Popping the (PICO) question in research and evidence-based practice. Nurs Res 15: 197-198.
- Ulmer-Yaniv A, Djalovski A, Yirmiya K, Halevi G, Zagoory-Sharon O, et al. (2018) Maternal immune and affiliative biomarkers and sensitive parenting mediate the effects of chronic early trauma on child anxiety. Psychol Med 48: 1020-1033.
- Valitutto MT, Aung O, Tun KYN, Vodzak ME, Zimmerman D, et al. (2020) Detection of novel coronaviruses in bats in Myanmar. PloS one 15: e0230802.
- Wang C, Pan R, Wan X, Tan Y, Xu L, et al. (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 17: 1729.
- Wen MC, Chan LL, Tan LC, Tan EK (2016) Depression, anxiety, and apathy in Parkinson's disease: insights from neuroimaging studies. Eur J Neurol 23: 1001-1019.
- Wu YC, Chen CS, Chan YJ (2020) The outbreak of COVID-19: An overview. J Chin Med Assoc 83: 217-220.
- Yeung KS, Hernandez M, Mao JJ, Haviland I, Gubili J (2018) Herbal medicine for depression and anxiety: A systematic review with assessment of potential psycho-oncologic relevance. Phytother Res 32: 865-891.
- Yirmiya K, Djalovski A, Motsan S, Zagoory-Sharon O, Feldman R (2018) Stress and immune biomarkers interact with parenting behavior to shape anxiety symptoms in trauma-exposed youth. Psychoneuroendocrinology 98: 153-160.
- Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA (2012) Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med 367: 1814-1820.
- Zhang Y, Ma ZF (2020) Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int J Environ Res Public Health 17: 2381.
- Zorzo C, Mendez-Lopez M, Mendez M, Arias JL (2019) Adult social isolation leads to anxiety and spatial memory impairment: Brain activity pattern of COx and c-Fos. Behav Brain Res 365: 170-177.