Madhumita Srivastava*,
Gaurav Vishal, Sanjoy
Chowdhury and Pramod
Kumar Biswal
Department of Oral and Maxillofacial Surgery, Bokaro General Hospital,
Jharkhand, India
- *Corresponding Author:
- Madhumita Srivastava
Department of Oral and Maxillofacial
Surgery, Bokaro General Hospital,
Jharkhand, India
Tel: +918986873108
E-mail: dr.madhumitasri.20@gmail.com
Received date: August 06, 2018; Accepted date: September 11, 2018; Published date: September 17, 2018
Citation: Srivastava M, Vishal G, Chowdhury S, Biswal PK (2018) Mental Nerve: An Unpredictable Course and Its Clinical Implication. J Univer Surg. Vol.6 No.2:18
Keywords:
Mental nerve; Mental foramen; Anatomical variation
Background
Mental nerve is the terminal branch of inferior alveolar nerve, which in turn is the branch of mandibular nerve, third division of trigeminal nerve. Maxillofacial surgeons should be vigilant while performing mandibular fractures or elective surgery below the premolar teeth as, just apical to second premolar lie the mental foramen, from which emerges the mental neurovascular bundle. Mental nerve is single, but different branching patterns of this nerve have been reported [1]. In this case report we show the chance discovery of trifurcated mental nerve emerging from single mental foramen. Knowledge of the branching pattern of the mental nerve is an important consideration during performing surgeries in the mandibular parasymphysis region.
Case Report
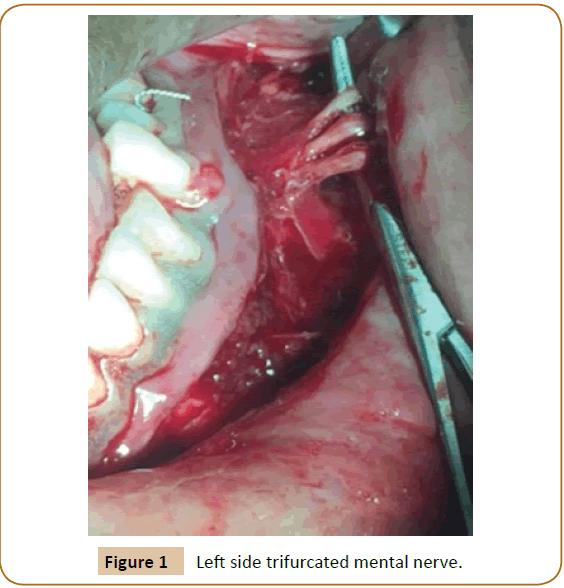
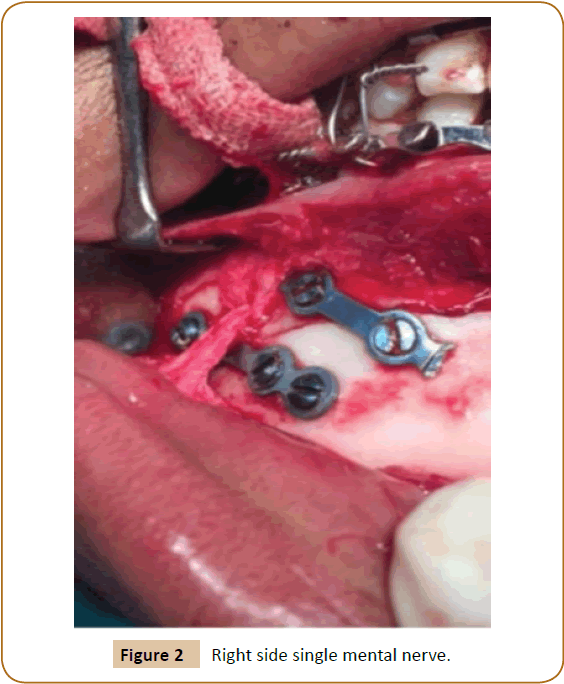
A 25-year-old male driver by profession reported to our Maxillofacial OPD with the chief complaint of pain while mouth opening and bleeding from the same, since two days. Patient was asymptomatic two days back when he met with an accident while driving. He fell on the ground facing his chin. He was taken to nearby health care centre for the same, and was send to our hospital after first aid. Detail history was taken and clinical examination was done. Extra orally patient had swelling and numbness of lower lip and chin. Mouth opening was restricted. Intra oral examination revealed step deformity and sublingual hematoma. A provisional diagnosis of bilateral mandibular symphysis fracture was made. An orthopentomograph (OPG) was advised for the same, which confirmed the diagnosis. So, open reduction and internal fixation via mini plates was planned under general anesthesia, followed by intra maxillary fixation for next fourteen days. For aesthetic reasons a conventional intraoral vestibular incision and subperiosteal dissection was done. During dissection on left side mental foramen was identified, with trifurcated mental nerve (Figure 1) with sub branches. All three branches were almost of the same diameter. It was surmised that the mental nerve was trifurcated just exiting the foramen. Careful dissection was continued freeing the nerves from the underlying bone and soft tissue. Each of them were separated and identified. On right side single mental nerve was there (Figure 2). Further in process, the nerves were protected using a retractor and the plate was passed beneath the nerves for fixation. Postoperative recovery was uneventful. The patient gradually recovered its sensation on the lower lip region.
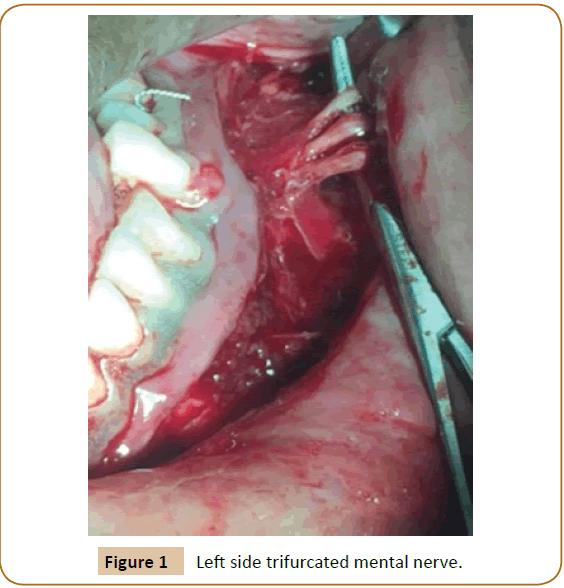
Figure 1: Left side trifurcated mental nerve.
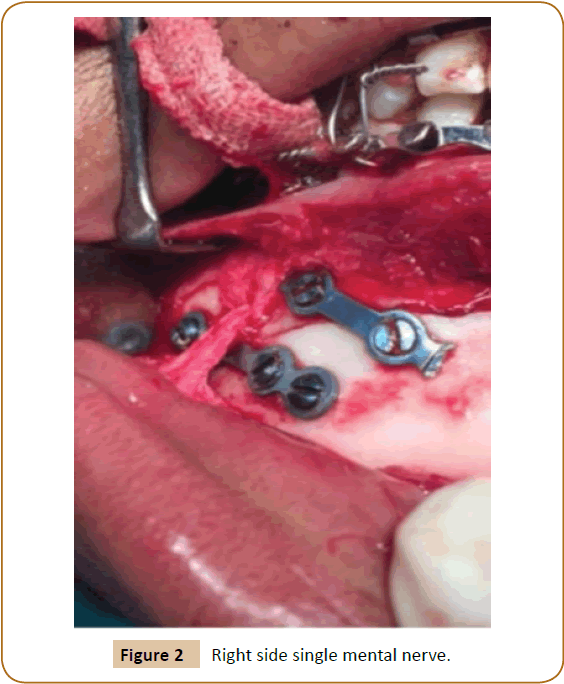
Figure 2: Right side single mental nerve.
Discussion
The mental nerve is the branch of the inferior alveolar nerve which is sensory, originates from the mandibular division of the trigeminal nerve. It arises from the same within the inferior alveolar canal of the mandible. As it exits from the mental foramen, it divides into three branches the mental branch, labial branch, and gingival branch, which supply the chin, lower lip and gingiva, respectively [2].
Mental nerve is vulnerable to injury during surgical procedures of the chin area such as genioplasty, mandibular anterior segmented osteotomy, internal fixation of fracture with reconstructive plates, dental implants etc.
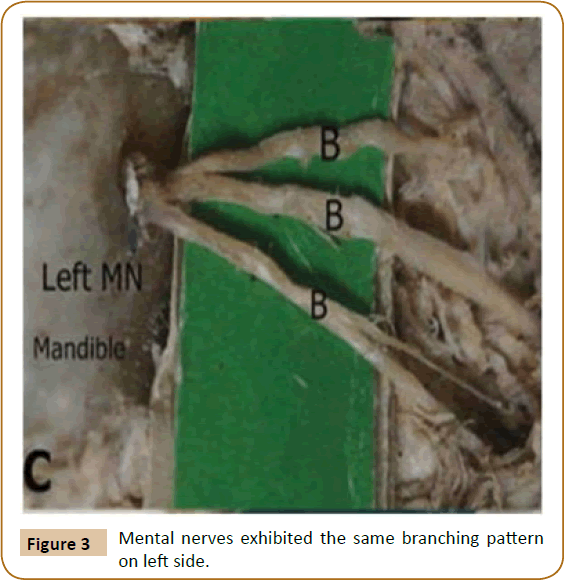
There are, however, several anatomic variations in the number of foramina and the branching patterns of the nerve. In our case we encountered trifurcated mental nerve on left side and single nerve from right side, originating from single mental foramen. This type of asymmetry is not frequently mentioned in literatures. The branching patterns of the mental nerve have been studied extensively. Trifurcated mental nerve branching seen in our case was similar to study done in 2013, shows on 6.25% of the mental nerves exhibited the same branching pattern on left side (Figure 3), [1] where as a study done in 2000 shows 56% homogeneity in branching pattern of the same [3]. Baris sahni et al. presented a trauma case with accidental finding of double mental nerve exiting from two separate mental foramen [4].
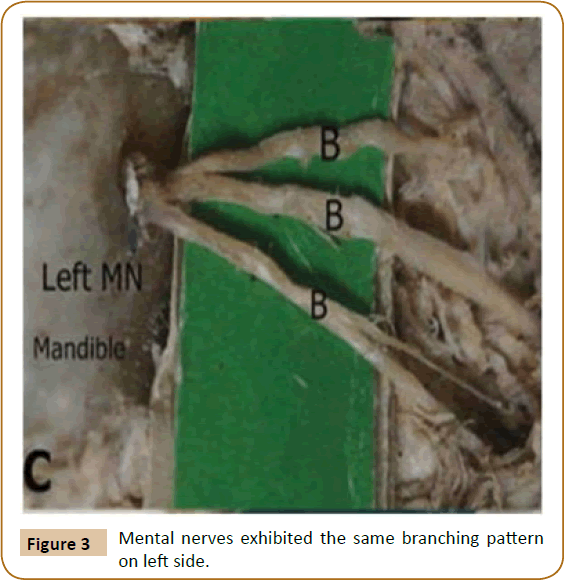
Figure 3: Mental nerves exhibited the same branching pattern on left side.
A cadaveric study done in 2013 inferred that single mental nerve was present in (93.7%) cadavers while double mental nerves occurred in (4.7%) and accessory in (1.6%). Mostly mental nerve was bifurcated (39%) followed by trifurcation (34%), single (19%), and quadrification (8%). The bi and trifurcated nerve branches was further divide into two to three sub branches with diverse patterns [1]. Many articles have been published regarding accessory mental foramen with accessory nerve [3,5-9].
Also it is important to know the branching pattern of the same, as an accessory branch can be used for facial nerve grafting, in biopsy of minor salivary gland, could be helpful in explaining failed anesthesia in the labiomental region etc. Damage to the nerve will lead to labiomental sensory disturbances which produce severe discomfort. Knowledge about the anatomical variability of mental foramen helps in salvaging the vital structures. In orthognathic surgeries these kinds of variations require modi?cations in placement of osteotomy cuts [10]. Thus, it is important to know the normal anatomy along with variations and therefore, preoperative diagnosis of such variations will be of great help for treatment planning.
In the modern era with the availability of cone beam computed tomography (CBCT) one can easily trace out the branching pattern of the nerve and damage to the nerve can be checked. Also with the emergence of navigation technique and CBCT we can plan our surgery accordingly.
Conclusion
This case study clearly deduce that one should be very prudent while operating in the mandibular parasymphysis region, as different branching pattern of mental nerve may be encountered and hence iatrogenic injury can occur. This may ultimately lead to permanent paresthesia of the concerned area. Hence this knowledge about the anatomical variability of mental foramen helps the clinician to avoid nerve damage in connection with surgical procedure and to achieve complete effect of anaesthesia after mental nerve block. It also guides to make appropriate changes in the treatment plan. Also branching pattern on the right and left side should not be treated in the same way during surgical maneuvers in mandibular parasymphysis area.
23353
References
- Loyal PK, Butt F, Ogeng'o JA (2013) Branching Pattern of the extraosseous mental nerve in a kenyan population. Craniomaxillofac Trauma Reconstr 6(4): 251-256.
- Peter D (2005) Surface anatomy of the head and neck, in: Standring S, Berkovitz KB, edition. Gray’s anatomy. 39th edn, Churchill Livingstone, Elsevier, USA.
- Alantar A, Roche Y, Maman L, Carpentier P (2000) The lower labial branches of the mental nerve: Anatomic variations and surgical relevance. J Oral Maxillofac Surg 58: 415-418.
- Baris S, Heval SO, Metin G (2010) An anatomical variation of mental nerve and foramen in a trauma patient. Int J Anat Variations 3: 165-166.
- Sonal S, Suhas V, Kriti K (2010) A Variation in the position of the mental foramen: A case report. J Maxillofac Oral Surg 9(3): 307-309.
- Poornima RP, Elavenil V, Sagnik S, Krishna KR (2017) Anatomical variant of the mental nerve and its foramen. SRM Journal of Research in Dental Sciences 8(2): 85.
- Kieser J, Kuzmanovic D, Payne A, Dennison J, Herbison P (2002) Patterns of emergence of the human mental nerve. Arch Oral Biol 47(10): 743-747.
- Sahoo A, Tripathy R, Padhiary SK, Sahu S (2016) Accessory mental foramen: A case report. Int J Sci Res Pub, 6(1): 490-493.
- Iwanaga J, Watanabe K, Saga T, Tabira Y, Kitashima S, et al. (2016) Accessory mental foramina and nerves: application to periodontal, periapical, and implant surgery. Clin Anat 29: 493-501.
- Wang C, Gui L, Liu J (2015) A practical surgical technique to expose the mental nerve in narrowing genioplasty. Plast Reconstr Surg Glob Open 3(11): 554.