Review Article - (2022) Volume 0, Issue 0
Multidisciplinary Approach in the Treatment of Patients with Spinal Injuries
Angel Fabian Leon Chavez,
Eucaris David Graciano,
Jairo Alejandro Alonso Bonilla,
Luisa Fernanda Ospina Caro,
Oswaldo Pérez Cabra and
Juan Felipe Villegas Lora
1Emergency Physician, Fundación Universitaria Ciencias de la Salud, Bogotá, Colombia, Colombia
General Physician, Universidad El Bosque, Bogota, Colombia
General Physician, Universidad Cooperativa de Colombia, Medellin, Colombia
General Physician, Universidad del Tolima, Colombia
General Physician, Corporacion Universitaria Remington, Medellin, Colombia
General Physician, Universidad del Rosario, Bogota, Colombia
General Physician, Universidad del Norte, Barranquilla, Colombia
*Correspondence:
Jhon Fredy Bello Cordero, Emergency Physician, Fundación Universitaria Ciencias de la Salud, Bogotá, Colombia,
Colombia,
Email:
Received: 11-Mar-2022, Manuscript No. Iphsj-22-12660;
Editor assigned: 13-Mar-2022, Pre QC No. PreQc No. Iphsj-22-12660 (PQ);
Reviewed: 27-Mar-2022, QC No. QC No. Iphsj-22-12660;
Revised: 01-Apr-2022, Manuscript No. Iphsj-22-12660(R);
Published:
09-Apr-2022, DOI: 10.36648/1791-809X.16.S6.925
Abstract
A traumatic injury to the spine has consequences on the patient's neurological status that may be irreversible. Its most frequent causes address different reasons, the main cause being automobile accidents, which lead to the combination of primary and secondary mechanisms that give the development of the pathophysiology of spinal cord injury. Therefore, the approach of a multidisciplinary approach is of vital importance for the treatment of a patient with a spinal cord injury in which pharmacological, surgical and physiotherapeutic aspects are considered relevant, carried out by a group of specialists with the aim of comply with a good management of patients in this condition. Therefore, it is important to recognize the different aspects that make up the treatment in order to present changes at the musculoskeletal level that improve the patient's quality of life in the long term.
Keywords
Multidisciplinary approach, Spinal cord injury, Treatment; Prevention, Diagnosis
Introduction
The spinal column supports and protects the spinal cord, its sheaths and roots. For this reason, a traumatic injury to the spine can very likely affect its content and, with it, produce significant neurological damage that can even become irreversible [[1].
A spinal cord injury is defined as any injury that compromises the spine, spinal cord or any supporting structure in general [2]. and is the result of a complex interaction of injuries sustained by the musculoskeletal and nervous systems. It is frequently associated with polytraumatism (long bones, pelvis, and thorax) and traumatic brain injury, which is a cause of disability in the patient, which causes severe physical and psychological damage, and generates enormous economic costs for the system.
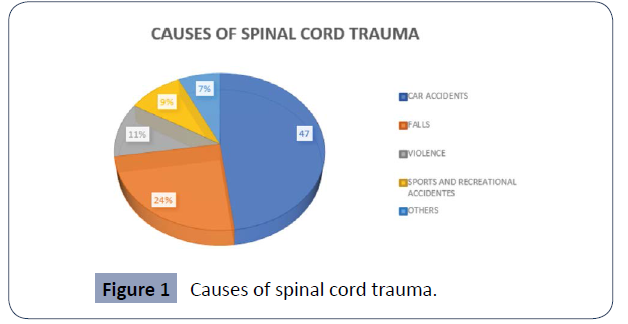
Epidemiologically, TRM is a life-destroying neurological condition globally, affecting between 250,000 and 500,000 people each year; It is estimated that two to three million people worldwide are living with a disability related to MRT. In the United States, the reported incidence of TRM is 12 to 55 patients per million inhabitants per year, with a prevalence of 253,000 people. Male patients are affected in a 4 to 1 ratio with respect to females and more than half of these cases occur in people under 30 years of age [3]. The most frequent causes are car accidents (46.9%- 50.4%), falls (23.7%), violence (11.2%-13.7%), sports accidents and recreational (8.7%-9.0%) and other causes (7%), [4] (Figure 1).
Figure 1 Causes of spinal cord trauma.
In terms of its pathophysiology, TRM (spinal cord injury) is a two-step process involving primary and secondary mechanisms. Any of the four basic mechanisms of primary injury must occur for primary injury to occur, including impact with transient compression, laceration transection, distraction, and impact plus persistent compression.
The first mechanism occurs in patients with degenerative disease of the cervical spine who suffer hyperextension trauma; the laceration-transection may be due to firearm projectiles, dislocated fractures or injuries with short puncture elements; distraction is the forced stretching of the spinal cord secondary to flexion, extension, rotation or dislocation, it is more frequent in people with degenerative disease of the cervical spine; Lastly, the mechanism of impact plus persistent compression is observed in fractures with burst fractures of the vertebral body and retropulsion of bone fragments that exert compression on the spinal cord.
Secondary spinal cord injury begins immediately or minutes after the injury and can last for several days or even weeks. In this, tissue damage increases progressively, affecting the different levels of the spinal cord. In addition, endothelial damage leads to increased permeability and the presence of intracellular edema, this being an important factor for the extravasation of cells of the immune system [5].
In turn, the evolution of this includes several phases: Immediate, Acute, Sub acute, Intermediate and Chronic. The immediate phase takes place between 0 and 2 hours, beginning at the time of trauma with detectable changes such as general swelling in the spinal cord followed by haemorrhage in the central Gray matter. In this, the cells present necrosis due to the mechanical disruption of the membranes and, in turn, an ischemia due to vascular disruption, the acute phase takes place between 2 and 48 hours, in this the primary damage occurs as a direct result of trauma and Once the structural thresholds are exceeded, immediate cellular and biochemical alterations begin to appear. In addition, this phase is marked by systemic and local alterations such as alterations in vascular mechanisms, ionic imbalance, and immune system response, among others. The subacute phase lasts approximately 2 days to 2 weeks, in which the phagocytic response increases in order to achieve a removal of the debrided tissue in the area of the injury, which allows possible axonal regeneration. The intermediate phase lasts approximately 2 weeks to 6 months, characterized by the maturation of the glial scar produced by the late astrocytic response, and during the chronic phase the degenerative process continues and extends to the areas surrounding the lesion, which they presentdepressed electrical and functional activity evolving to what is known as secondary injury and therefore a subsequent loss of neuronal function. Trauma, in addition to producing neuronal death, causes glial cell lysis, destruction of blood vessels and injury to axonal tracts that, since they cannot regenerate, cause the alterations to be permanent [6].
Regarding diagnosis, initially the patient's approach consists of evaluating the "ABCD", prioritizing airway patency, ventilation and circulation, establishing spinal immobilization measures in the required time, since airway management ventilation and the proper administration of mechanical ventilation is highly relevant to maintain homeostasis, by avoiding or reducing the risk of worsening the injury or the development of respiratory complications that together can generate morbidity and mortality by themselves [7]. Subsequently, when the patient is stable, a neurological evaluation is performed. If the patient is unconscious, the presence of spinal cord injury should be considered and suspected if signs of limb paresis or paralysis, loss of sensitivity, difficulty in language, arterial hypotension, diaphragmatic breathing, and pain in the spine, priapism, and urinary incontinence should be considered. And rectal. If the patient is active and alert, a more detailed and specific sensory and motor evaluation is performed [8]. The principle is “not to move it” or, if required, to do it carefully supporting the spine completely and keeping in mind its alignment by supporting the head and making sure that it and the body move in unison. Keeping the spine in alignment means keeping it in the line that, prior to the trauma, was normal for the patient. It should be noted that all patients with neurological injury, it can mask symptoms of injury in other organs due to the absence of pain [9].
Neurological damage is classified as complete or incomplete, depending on the involvement at the sacral level. Sphincter function and persistent perineal sensitivity are associated with incomplete lesions and a favourable prognosis. Lesions located at higher levels of the spinal cord are associated with greater sympathetic autonomic dysfunction, unlike lesions located at lower levels of the spinal column in which parasympathetic autonomic functionality is compromised, generating priapism and loss of the functionality of the urinary bladder and intestine. For its part, the radiological examination generates a more precise diagnosis. Simple radiography is a traditional method; however, helical tomography is more sensitive, more specific and is the type of image of choice. It makes it possible to visualize fractures that may go unnoticed with plain radiographs, it generates a complete projection of the spine with which the invasion of the canal can be better characterized and it is useful in surgical treatment [10].
The first aspect in the management of a patient with a MRT is making a correct diagnosis. In conscious patients who complain of neck and back pain with difficulty moving the extremities, the diagnosis is easy. However, in those individuals who are unconscious as a result of a head injury (TBI) or in the course of a severe trauma in another region of the body, the diagnosis is not so clear. In these latter circumstances, they must be managed as if they had a spinal cord injury until proven otherwise: all patients with a TBI, patients with awareness, people with minor trauma who show discomfort in the neck or back or present symptoms such as tingling, numbness, weakness or paralysis of one or more extremities, abdominal breathing or priapism. The evaluation of the patient will be carried out quickly and accurately through a clinical history that clarifies the probable mechanism of the injury, the state of consciousness and the existence of motor weakness at some point after the trauma [11].
From a multidisciplinary approach, which includes several aspects of the treatment implemented in this type of patient, beginning with the pharmacological one, during which an initial dose of 30 mg/kg of methylprednisolone is administered, followed by 5.4 mg every hour, since it has shown to be beneficial for the recovery of motor and sensory functions, since methylprednisolone is capable of suppressing secondary neuronal death. In turn, surgical treatment focuses on performing spinal decompression to reduce neurological damage as soon as advisable and stabilize the spine to start as soon as possible with an adequate rehabilitation program [12]. which includes upper extremity athletics. (chain of downspouts and extensors) and of the trunk according to the level, maintenance of the integrity of the injured segment, seated balance work according to well-codified and progressive exercises. Once the balance is acquired, the work of all the transfers necessary for its autonomy, first on the Bo bath table, then in a real situation. All of these trunk and extremity athletic goals require traditional physical therapy techniques, but are also greatly aided by sport, a true rehabilitation tool. The choice of chair must be adapted to the level and morphology of the patient, as well as the type of activity that he wishes to carry out. Folding or with rigid frames, they are most often lightened. The adjustment of the seat and the footrest must ensure the distribution of the support zones. The choice of cushion will depend on intrinsic risk factors (orthopaedic imbalance, skin fragility) and seat pressure analysis systems help enormously. As soon as you get in the chair, you should learn the deadlift to alleviate risk areas. The handling of the wheelchair will also be carried out according to a particular hierarchy: exercises on flat ground, periodic "rolling" with the sports monitor, obstacle course, fall learning and readings and dead weight training must be carried out to unload the risk areas [13].
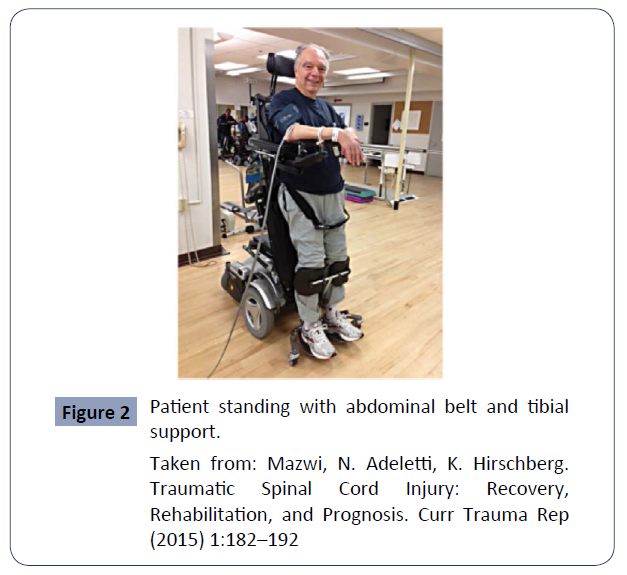
Rehabilitation goals include tolerance to the upright position, which is assessed through exercises to sit up, raise the head of the bed, and use a tilt table or standing frame [14], as seen in Figure 2.
Figure 2 Patient standing with abdominal belt and tibial support.
Taken from: Mazwi, N. Adeletti, K. Hirschberg. Traumatic Spinal Cord Injury: Recovery, Rehabilitation, and Prognosis. Curr Trauma Rep (2015) 1:182â??192
Physiotherapy treatment has medium and short-term objectives: Strengthen gluteus medius muscle, tensor fascia lata, gastrocnemius, soleus, tibialis anterior, tibialis posterior, peroneus longus and brevis, rectus abdominis, oblique and transverse muscles. Re-educate superficial and deep sensitivity, facilitate changes in position from sitting to quadruped and knee, favor transfer from mat to wheelchair, from wheelchair to chair, re-educate gait in the support and swing phases with partial physical support, through modalities physical such as cryotherapy and massage; and kinetic modalities such as the Bobath and Kabat methods [15].
All the deficiencies derived from the injury require specific care that the person and the family must learn during the different stages of comprehensive rehabilitation, guided by the intermediation of interdisciplinary health teams such as health professionals such as physiatrists, physical therapists, occupational therapists , psychologists, psychiatrists, nutritionists and nurses, since this is a process that affects several important aspects in the life of the patient, which requires the presence of comprehensive support, so that in addition to the intervention carried out by these professionals, it is required supplies for health care such as orthopaedic equipment and wheelchairs that facilitate patient mobility, supplies for neurogenic bladder and bowel care, pharmacological treatments for pain control, spasticity, skin care and nutrition [16].
Methodology
In this review article, a detailed bibliographic search of information published since 2010 was carried out in the databases PubMed, Elsevier, Scielo, national and international libraries. We use the following descriptors: multidisciplinary approach, spinal cord injury, treatment, prevention, diagnosis. The data obtained ranges from 2 to 15 records after the use of the keywords. The search for articles was conducted in Spanish and English, limited by year of publication, and studies published since 2010 were used.
Result
In his report and case analysis, Cabezas presents a 58-year-old patient who presents with quadriparesis caused by spinal cord trauma. A complete neurological examination was performed and it was determined that he presented with an H pattern with impaired motor function, peripheral nerve integrity and sensory integrity associated with non-progressive disorders of the spinal cord, related to moderate pain deficiency associated with stabbing pain on passive shoulder movements. , elbow, hip and knee with predominance in the right side of the body; in vestibular functions associated with balance and movement; severe deficiency in functions related to motor reflexes andfunctions related to the gait pattern associated with reflexes generated by exteroceptive stimuli and clumsy or stiff gait, all with the help of third parties. In the musculoskeletal domain, the patient presents pattern F with deficiency in joint mobility, motor function, muscle performance, range of motion and reflex integrity associated with spinal disorders and fracture; where she presents, serious deficiency in functions related to muscle tone due to the fact that she presents hypotonia in all four extremities; severe deficiency in functions related to muscle strength and mobility functions of the joints associated with muscle paresis at the level of the four extremities and joint stiffness at the level of the wrist, ankle and bilateral phalanges. In the integumentary domain, the patient presents pattern B with deficiency in integumentary integrity associated with superficial involvement of the skin; where she presents severe deficiency in protective functions of the skin associated with decubitus ulcers. In relation to the activities and participation in the domain of communication, affect, cognition, language and learning style with respect to the deficiencies within the components of the activities and participation in the 95 construct and capacity qualifier related to the health condition of the patient, presents moderate difficulty to move using some type of equipment; as well as lifting, carrying, and fine hand use, complete difficulty performing single and multitasking, as well as washing (bathing, showering, hand washing), care of body parts (washing teeth), personal hygiene related to the processes of excretion and selfcare, complete difficulty dressing and eating, severe difficulty changing basic body postures, walking, and finally slight difficulty maintaining a standing body position; Continuing with the construct and qualifier of performance of bodily functions related to the environment, it presents moderate difficulty in all the aforementioned difficulties since it has the help of third parties and appropriate materials.
This makes evident the great dependence that the patient acquires, for which her quality of life decreases on a large scale, making it necessary to implement an approach that strengthens each of the aspects affected by the trauma.
Initially, training and instruction was given to the patient and family members; and a physiotherapeutic plan was structured with the aim of reducing pain, through biophysical agents, therapeutic massages; to facilitate voluntary movement, through kinesitherapy exercises; establish muscle re-education using Kabat techniques (PNF); postural control training using the Bobath concept; maintain balance while sitting and bipedal through proprioception exercises and postural control exercises; in this way managing to make changes of position in bed and from seated to bipedal, through 72 sessions, 3 times a week, with a duration of 1 hour per session, for 6 months. In addition, it was recommended that the patient be encouraged to receive comprehensive health care, including follow-up by other health professionals, mainly in the nutritional and psychological aspects. [17].
Ramirez and Vinasco, in their cross-sectional descriptive study, included a sample of 53 people over 18 years of age, men and women without differentiating ethnic group, treated in two institutions in the city of Cali (Spinal Cord Trauma Clinic of the Rehabilitation Unit del Valle University Hospital and Neurorehabilitation Centre "Surgir. In this, the mechanisms used by the person with TRM to access care services by interdisciplinary teams, treatments and technical resources that allow comprehensive rehabilitation are described.
It was inquired in relation to access to care by interdisciplinary teams such as: physical medicine and rehabilitation, physiotherapy, nursing, psychology, psychiatry and occupational therapy. Of these, it was shown that more than 80% of the patients received direct authorization from the EPS for physiotherapy and physical medicine and rehabilitation care. However, deficiencies were found for comprehensive rehabilitation related to psychology and occupational therapy. Thus, for 74% the EPS did not authorize psychological care, and of these, approximately 36% [13]. established a guardianship action, the others did not resort to any other mechanism. Regarding access to pharmacological treatment, it was evidenced that 46 people required pharmacological pain management, 78% of the people the EPS did not directly authorize the supply of these medications and of these 81% [29] filed a tutela action [18]. Due to this, a protection program is necessary for this type of patients, which guarantees them access to all the necessary equipment for their recovery, in addition to the constant administration of the necessary medications to treat the secondary effects of the trauma, such as pain, neurogenic bladder, constipation, among others; which will help them have a better quality of life.
On the other hand, it has been shown that a large percentage of patients with spinal cord trauma develop pressure ulcers located mainly in the sacrum and heels. The frequency of appearance of a pressure ulcer is directly related to the time elapsed between the accident and admission to a spinal cord injury canter and significantly prolongs the stay in the clinic until the start of rehabilitation [19] This is treated in turn with several elements that include preconditioning the ulcer with pressure relief, highly specialized surgical procedures with different flap techniques, and complex Interprofessional interventions that include nursing, nutrition and psychotherapy, physiotherapy, and occupational therapy [20].
Discussion
Spinal cord injury is a relatively rare event that represents a significant medical problem for patients, health care providers Health and the health care system [21]. Thus, there are several phases of care that affect each patient with an acute bone marrow injury, including initial trauma management, acute surgical intervention, and perioperative medical management, thus each phase of care it requires the work of an interdisciplinary team focused on providing effective and efficient medical care to maximize patient outcomes [22].
Given the previous review of the bibliography, it has allowed us to know the different aspects related to the management and treatment of spinal cord injury. In the first place, from a pharmacological point of view, methylprednisolone continues to be an area of controversy, with the aim of reducing the inflammatory response that occurs in the injured area and
limiting secondary damage to the spinal cord [23] since it has been proven that it reduces excitatory amino acid neurotoxicity, inhibits lipid peroxidation, increases blood perfusion to spinal tissue, and slows traumatic ionic changes thus allowing it to have the potential to inhibit inflammatory damage to the spinal cord [24]. But, high-dose methylprednisolone was tested in the National Acute Spinal Cord Injury Study (NASCIS) trials. These trials showed higher rates of pneumonia, sepsis, acute respiratory distress syndrome, gastrointestinal bleeding, and death among patients treated with corticosteroids [25]. Furthermore, recent studies provide evidence that there is a neurological benefit of early surgical decompression and have led to the recognition that the injured spinal cord should be decompressed urgently [26]. The Surgical Timing Study in Acute Spinal Cord Injury (STASCIS) was a prospective multicenter study of 313 patients with cervical spinal cord injury undergoing surgical decompression and instrumentation. In this study, early surgery was defined as less than 24 hours after the initial injury. The researchers found that even after adjusting for preoperative neurological status and steroid administration, patients who underwent early surgery were 2.8 times more likely to have at least a 2-grade improvement in AIS score. Patients who underwent early surgery were significantly more likely to be fully motorized (ASIA grade A/B; 57.7% vs. 38.2%) [27]. So there is a stronger impact on the neurological recovery with early surgery in patients with incomplete injury, and there are data that the sooner surgery is performed, the greater the neurological benefit. Furthermore, exercise not only directly strengthens paralyzed muscles and promotes motor recovery, but also promotes brain remodelling, improves the spinal microenvironment, and protects impaired distal motor neuron functions, at multiple levels and through various channels, promoting thus functional recovery It was shown that exercise after SCI could improve functional prognosis and induce recombination of the cerebral cortex in the somatic region. These observations have been recorded in both animal experiments and clinical studies. By For example, post-SCI exercise rats have shown a higher rate of spontaneous firing of cortical neurons and improved sensory and sensorimotor stimulation of the forelimbs In addition, exercise can affect brain function remodelling after SCI, by generating systemic changes, such as improved blood circulation and neuroendocrine regulation, and reduced spasticity [27].
Conclusion
Spinal cord injury following trauma is the result of a complex interplay of injuries to the musculoskeletal and nervous systems. Therefore, the treatment approach takes into account different multidisciplinary aspects with the aim of improving the patient's condition, therefore the pharmacological, surgical and physiotherapeutic application will allow reducing the inflammatory response that occurs in the injured area and limit the damage. Secondary to the spinal cord, improve neurological decompression and recovery with early intervention, and induce structural and functional changes in the cerebral cortex, spinal cord, and skeletal muscles, thereby improving neural and muscle function after spinal cord injury spinal.
REFERENCES
- Rivero R, Rivero J, Acevedo J, Castro E (2018) Caracterización clínico-quirúrgica de pacientes ingresados por traumatismo raquimedular. Universidad de ciencias médicas de Cienfuegos.
Google Scholar
- Teherán A, Castro O, Laverde L, Incidencia y (2016) Características del Trauma Raquimedular en un Hospital de III Nivel, Bogotá 2011–2014. J Trauma Acute Care Surg 5:140-147.
Indexed at, Google Scholar
- Bustamante R (2021) Traumatismo raquimedular Rev Chil Anest 50:126-158.
Indexed at, Google Scholar, Crossref
- Ho CH, Wuermser L-A, Priebe MM (2007) Spinal cord injury medicine Epidemiology and classification. Arch Phys Med Rehabil 88:S49-S54.
Indexed at, Google Scholar, Crossref
- Mataliotakis GI, Tsirikos AI (2016) Spinal cord trauma pathophysiology, classification of spinal cord injury syndromes, treatment principles and controversies. Orthopaedics and Trauma30:440-9.
Indexed at, Google Scholar, Crossref
- Padilla H, Ramos Y, Alvis H, Joaquin A, Moscote L (2017) Fisiopatología del trauma raquimedular. Revista Mexicana de Neurociencia. 18:46-53.
Google Scholar
- Niño M, Cohen D, Amaya O (2019) Manejo de la vía aérea y ventilación mecánica en trauma craneoencefálico. Trauma craneoencefálico, lo esencial. Sociedad Colombiana de Anestesiologí-Reanimación.
Indexed at, Google Scholar
- Lavanderos J, Muñoz S, Vilches L, Delgado M, Carcamo K et al.(2008)Traumatismo raquimedular. Cuad Cir 22:82-90.
Indexed at, Google Scholar
- Galeiras R, Ferreiro M, Mourelo M, Montoto A, Salvador S (2017) Actualización en lesión medular aguda postraumática. Revista Medicina Intensive 41:237-247.
Google Scholar, Crossref
- Castillo A (2021) Traumatismo raquimedular cervical subaxial en adultos del servicio nacional de neurocirugía del hospital Antonio Lenin Fonseca Martínez, atendidos entre el mes de diciembre 2018- noviembre. Tesis para optar al título de especialista en Neurocirugía. Universidad Nacional Autónoma de Nicaragua.
Indexed at, Google Scholar
- Cruz-Conde R, Castel F, Sánchez J, Ríos B (2010) Abordaje anterior para lesiones traumáticas de la columna cervical baja. Resultados a largo plazo. Rev esp cir ortop traumatol 54:3-12.
Indexed at, Google Scholar, Crossref
- Perrouin B (2005) rééducation réadaptation des blessés médullaires. Bull Acad Natle Méd 189:1159-1174.
Indexed at, Google Scholar, Crossref
- Mazwi N, Adeletti K, Hirschberg (2015) Traumatic Spinal Cord Injury: Recovery, Rehabilitation, and Prognosis. Curr Trauma Rep 1:182-192.
Indexed at, Google Scholar
- Fernandez C, Romero Y, Peñaloza K, Pelaez M, Vasquez Y et al. (2014) Intervención fisioterapéutica en un paciente con trauma raquimedular a nivel de L2. Rev salud mov 6:1-11.
Google Scholar
- Burbano C, Ramirez J, Vinasco Y (2018) Calidad de la atención en salud de las personas con trauma raquimedular según criterios normativos de Colombia. Rev. Salud Pública. 20:655-660.
Indexed at, Google Scholar, Crossref
- Cabezas I (2019) Atención fisioterapéutica en paciente con cuadriparesia por trauma raquimedular en la comunidad de “Carpuela” de la provincia de Imbabura”. Trabajo de Grado. Universidad Técnica del Norte Ibarra Ecuado.
Google Scholar
- Ramirez J Vinasco Y (2016) Normatividad en salud y rehabilitación integral: una mirada desde la persona con trauma raquimedular. Trabajo de grado. Universidad del Valle. Cali, Colombia.
Google Scholar
- Meier C, Boes S, Gemperli A, Gmünder H, Koligi K (2019) Treatment and cost of pressure injury stage III or IV in four patients with spinal cord injury: the Basel Decubitus Concept. Spinal Cord Series and Cases 5:30.
Indexed at, Google Scholar, Crossref
- Ahuja CS, Martin AR, Fehlings M (2016) Avances recientes en el manejo de una lesión de la médula espinal secundaria a un traumatismo. Res. 5: 1-13.
Indexed at, Google Scholar, Crossref
- Gupta R (2010) Advances in the Management of Spinal Cord Injury. American Academy of Orthopaedic Surgeon 18:210-222.
Indexed at, Google Scholar, Crossref
- Rabinstein A (2018) Traumatic Spinal Cord Injury. Continuum (Minneap Minn) 24:551-566.
Indexed at, Google Scholar, Crossref
- Karsy M, Hawryluk G (2019) Manejo médico moderno de la lesión de la médula espinal. Curr Neurol Neurosci Rep 19.
Indexed at, Google Scholar, Crossref
- Fehlings MG, Vaccaro A, Wilson JR (2012) Descompresión temprana versus tardía para la lesión traumática de la médula espinal cervical: resultados del tiempo quirúrgico en el estudio de lesión aguda de la médula espinal 7:e32037.
Google Scholar
- Piazza M, Schuter J (2017) Momento de la cirugía después de una lesión de la médula espinal Neurourg Clin N Am 28:31-39.
- Fu J (2016) Exercise Training Promotes Functional Recovery after Spinal Cord Injury. Neural Plast 1.
Indexed at, Google Scholar, Crossref
- Kao T, Shumsky JS, Knudsen EB, Murray M, Moxon KA (2011) Papel funcional de la organización cortical inducida por el ejercicio de la corteza sensoriomotora después de la sección espinal. Revista de neurofisiología106:2662–2674.
Indexed at, Google Scholar, Crossref
- Rayegani SM (2011) efecto del ciclo eléctrico pasivo sobre la espasticidad en los veteranos de guerra con lesión de la médula espinal. Fronteras en neurología 2:39.
Google Scholar
Citation: Citation: Bello Cordero JF, Zumaque Carrascal AM, Leon Chávez AF, David Graciano E, Alonso Bonilla JA, et al. (2022) Multidisciplinary Approach in the Treatment of Patients with Spinal Injuries. Health Sci J. Vol. 16 No. S6: 925.