Keywords
Multiple Myeloma; Plasma cells; β2 microglobulin
Introduction
Multiple myeloma (MM) is a plasma cell disorder characterized by clonal proliferation of malignant plasma cells in bone marrow. This can be detected by monoclonal protein in the blood or urine, and dysfunction of associated organs. It is classified as asymptomatic or symptomatic depending on the absence or presence of an organ lesion or dysfunction of the affected organ tissue. Its presentation may vary, which makes the diagnosis harder; especially in early stages where the patient has better prognosis [1-3]. The MM represents 1% of neoplastic diseases and 13% of hematologic cancers [1,3,4]. In Western countries, the adjusted annual age incidence is 5.6 cases per 100,000 people. The average diagnosis age is around 70: 37% of patients are under age 65, 26% are between the ages of 65 and 74, and 37% are 75 years of age or older [1]. The risk of infection in patients with MM increases mainly due to polyclonal hypogammaglobulinemia [4], but there are also other reasons such as: reduction of CD4 + T cells, functional impairment of the natural killer cells, abnormalities in the complement system, and occasional granulopenia [5] which constitutes the leading cause of mortality in these patients. The risk of infection exceeds 7-15 times that of a hospitalized patient for any other reason [4,5]. The diagnosis of multiple myeloma is based on the presence of at least 10% plasma cells in the bone marrow sample and the presence of monoclonal protein in serum or urine. In patients with Nonsecretory myeloma, the diagnosis is based on the presence of 30% plasma cells or evidence of plasmacytoma in the bone marrow [3].
Case Presentation
A 63-years-old male, farmer presents with history of six months of generalized musculoskeletal pain that has gradually increased. He has been treated with oral and intramuscular analgesics without improvements. He also reports an onset of weakness, myalgia, anorexia, and a presence of abscess in left gluteal area. The patient is hospitalized in a Regional Hospital where he receives antibiotic coverage for seven days with no improvements. The musculoskeletal pain persists and limits ambulation, for this reason, he is transferred to the University Hospital.
Past medical history
Hypertension for over a year; currently managed with atenolol, 100 mg a day. Two months ago, history of a stroke without neurologic damage or motor deficit. Pneumonia in two occasions that required antibiotic coverage and hospitalization for more than 21 days.
At hospitalization it presents vital signs
Heart Rate: regular 71 bpm, Respiratory Rate: 18 rpm, Temperature: 37°C, O2 Sat: 98%, Weight: 80 Kg, Height: 5 feet and 7 inches. At physical examination we find a male alert and oriented, cooperative. Poorly nourished with pale and thin skin, with facies of chronic disease and overall clinical deterioration. His gait is slow, with ambulation difficulty due to musculoskeletal pain. The left gluteal area presents an abscess in resorption with scarce purulent material. The rest of the physical examination is normal.
Laboratory findings
Kidney ultrasound findings: The Right kidney measures 121 mm × 64.8 mm. The left kidney measures 118 mm × 68 mm. Kidney parenchyma is normal and corticomedullary relation is normal. Evidence of moderate urinary stasis at the pyelocaliceal region of the left kidney with lithiasis of 7 mm. Bladder without abnormalities (Table 1).
| Complete blood count |
Blood chemistry |
Immunologic |
| Hg |
10.1 g/dl |
Glucose |
143mg/dl |
Protein Immunofluorescence |
| Hct |
32.1% |
BUN |
12mg/dl |
Albumin: 26.9 (55-66%)
Alpha1:5.7%(2.9-4.9)
Alpha2:11.5% (7.1-11.8)
Beta1:3.4%(4.7-7.2)
Beta2:3.7% (3.2-6.5)
Gamma:48.8%(11.1-18.8) |
| MCV |
82 fl |
Creatinine |
2.7mg/dl |
| MCH |
27.3 pg |
AST |
30 U/L |
| Platelets |
229.000 ul |
ALT |
33 U/L |
| Leukocytes |
5730ul |
Sodium |
144 meq/L |
| Neutrophils |
4140ul |
Potassium |
3.9 meq/L |
| Lymphocytes |
1290ul |
LDH |
297 u/L |
Immunoglobulins |
| |
|
Albumin |
1.5g/dl |
IgG: 6948mg/dl
IgE: 22.4Iu/ml
IgM: 16.8 mg/ml
IgA: 18.3mg/dl |
| |
|
Calcium |
8.5mg/dl, |
| |
|
Uric Acid |
8.9 g/dl |
| |
|
|
|
| |
|
|
|
β2microglobulin: 8.82g/dl |
Table 1: Kidney ultrasound findings.
Bone survey: Lateral x-ray of the skull: Multiple well circumscribed lytic lesions with a diameter between 0.5 cm to 2.5 cm. The rest of the study was without abnormalities.
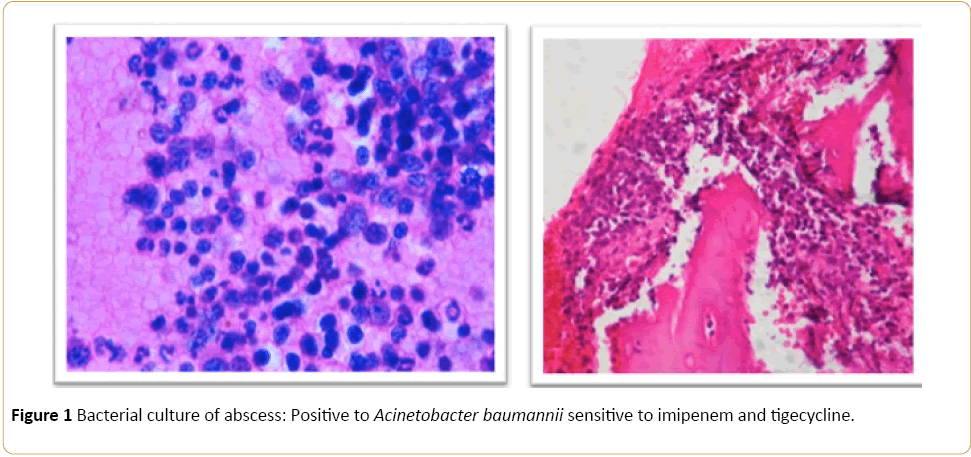
Bacterial culture of abscess: Positive to Acinetobacter baumannii sensitive to imipenem and tigecycline (Figure 1).
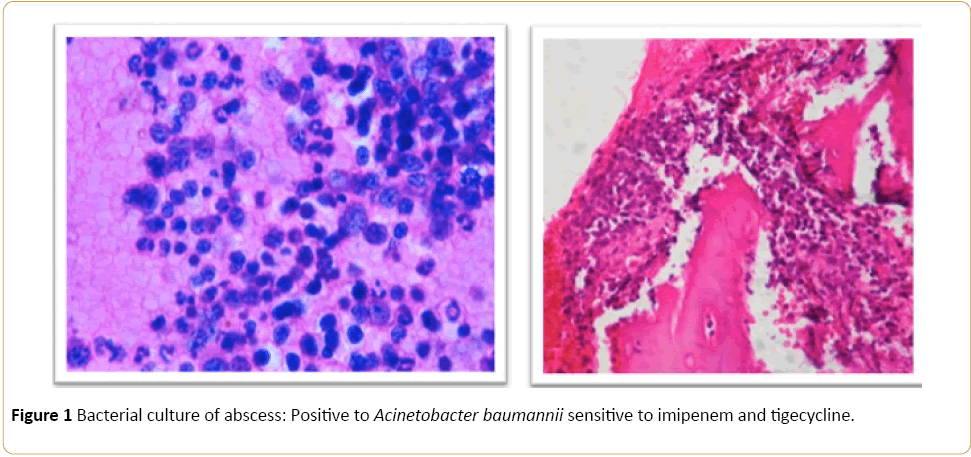
Figure 1: Bone marrow biopsy: Plasma cell infiltration of more than 10%.
Bence-Jones protein: Negative
Urine analysis: Presence of high concentration of calcium oxalate crystals.
Bone marrow biopsy: Plasma cell infiltration of more than 10%.
Discussion
Multiple Myeloma is characterized by a clonal proliferation in the bone marrow that causes a marked hypogammaglobulinemia; which is the main reason for the development of severe infections in immunocompetent patients.
Severe episodes of infections falling between 0.8% to 2.2% of the total Multiple Myeloma diagnosis every year are described as being the leading cause of death in these patients. These cases are most often associated with bacterial infections of the lung and the urinary tract. Nonetheless, there are also reports of viral and fungal infections [5].
The physical examination in these patients is usually normal, with the exception of patients with clonal proliferation in the adjacent bone. This clonal proliferation causes destruction of bone, bone fractures, and pain. Other important features that may occur include: anemia, hypercalcemia, renal failure, susceptibility to infection, coagulation problems, neurologic symptoms, and vascular problems due to hyperviscosity.
Reviewing our case, we have a patient with generalized musculoskeletal pain who develops a gluteal abscess from intramuscular analgesics self-medicated and presents a past medical history in the last year of two episodes of Pneumonia that required hospitalization. However, after adequate management, abscess drainage, and broad antibiotic therapy; the patient symptoms did not improve. The patient therefore, is re-evaluated and transferred to the University hospital in the capital city. Upon arrival, the patient presented with difficulty in ambulation due to generalized pain and marked deterioration of his overall condition.
The latest criteria to diagnose symptomatic Multiple Myeloma requires the presence of organ or tissue damage related to the proliferating tumor defined by the presence of at least one of seven possible manifestations [5]:
• Anemia with a decrease in hemoglobin of at least 2 g/dl compared to the normal value, or a hemoglobin below 10 g/dl.
• Hypercalcemia greater than 10 mg/dl (0.25 mmol/l) above normal or an absolute number greater than 110 mg/dl (2.75 mmol/l) of serum calcium.
• Osteolytic lesions, osteoporosis, or compression fractures with no attributable cause.
• Renal Failure, with creatinine of more than 2 mg/dl or 173 mmol/l
• Symptomatic Hyperviscosity;
• Amyloidosis
Recurrent bacterial infections (>2 severe episodes that required hospitalization over a period of 12 months). The presence of these abnormalities is important because without organ lesion, the asymptomatic forms of Multiple Myeloma will not require treatment; only proper monitoring.
To state prognosis and decide proper management the international system of stratification is used. This stratification system divides Multiple Myeloma in three stages according to the level of serum protein and β2 level [1,6,7].
• Step I: serum β2 - microglobulin <3.5 mg/liter, serum albumin ≥ 3.5 g/dL
• Step II: serum β2 - microglobulin, <3.5 mg/liter, plus serum albumin <3.5 g/dl; or
β2 microglobulin of 3.5 to <5.5 mg/l, irrespective of serum level of serum albumin
• Stage III: serum β2 - microglobulin ≥ 5.5 mg/liter
The laboratory data findings in the patient where: Normochromic normocytic anemia, acute renal failure, and hypoalbuminemia.
The increase in beta-2-microglobulin is indicative of high tumor burden and renal failure is one of the main predictors of the disease [5]. Currently, the median survival does not exceed four years with conventional chemotherapy [4,7].
Our case was classified as Multiple Myeloma Stage III due to the levels of β2 – microglobulin greater than 5.5 mg/liter. The first-line therapy is induction therapy, followed by high dose therapy and autologous hematopoietic stem cell transplant [4]. Our patient was not a candidate for first-line therapy due to his age and his tumor stage. Age is an important marker not only for survival, but also for chemotherapy tolerance [8].
It is estimated that a patient under 65 in stage II has a survival of 50 months, while for patients older than 65 years at a similar stage have a survival rate of only 37 months [4]. New drugs, such as bortezomib, thalidomide or lenalidomide, in combination with traditional chemotherapy are the treatment of choice in this group of patients [4,5,9]. The use of these drugs has significantly improved the complete remission rate and the overall survival in these patients [9]. Induction in these patients should be based on classical treatment schemes, such as mepfalan or high doses of dexamethasone combined with one of the new drugs as thalidomide or bortezomib [5,10]. We used this therapy for our patient with very good response and tolerance. A high dose of 40 mg of dexamethasone plus 100 mg of thalidomide was prescribed daily during the first month. Due to the good response to the initial therapy, the dose of thalidomide was increased to 100 mg twice a day during the second month. The patient currently continues to be monitored in the outpatient clinic of hematology.
9816
References
- Palumbo A, Anderson K (2011) Diagnosis and therapy of multiple myeloma. N Engl J Med 364: 1046-1060
- Robert AK, Ellen DR, Terry MT (2007) Clinical course and prognosis of smoldering (asymptomatic) multiple mieloma. N Engl J Med 356: 25.
- Joan B (2006) Monoclonal gammopathy of undetermined significance. N Engl J Med 355: 26.
- David GA (2009) Guías mexicanas de diagnóstico y recomendaciones terapéuticas para mieloma múltiple. Revi Hematologia 11: 40-62.
- Ramón GS, María VM (2007) Mieloma múltiple, Servicio de Hematología. Hospital Universitario de Salamanca. Centro de Investigación del Cáncer, Salamanca. España. Med Clin (Barc) 129: 104-115.
- Serra-Valdés M, Alfaro-Amigó A, Viera-García M (2013) Síndrome de hiperviscosidad como presentación del mieloma múltiple. Reporte un de caso. Revista Finlay (revista en Internet) 3: 4.
- Bart B, Alan M, Frits van R, Joshua E, Gareth JM, et al. (2014) Curing myeloma at last: defining criteria and providing the evidence. National Center of Biotechnology Medicine Blood 124.
- Heinz L, Brian GM, Vanessa B, Ingemar T (2008) Myeloma in patients younger than age 50 years presents with more favorable features and shows better survival: an analysis of 10,549 patients from the International Myeloma Working Group. Blood 111: 8.
- Philippe M, Michel A, Thierry F (2015) Frontline therapy of multiple myeloma. Blood 125: 20.
- Joan B, Laura R, Carlos FL (2015) How I treat relapsed myeloma. Blood 125: 10.