Introduction
The incidence of myelomeningocele associated with hydrocephalus is still high compared to the western world. The effectiveness of their management is determined by so many factors like how aggressive is the hydrocephalus, the site of myelomeningocele, the extent of the neural tissue involved, the size of the defect and the timing of surgery for both the shunting as well as the myelomeningocele repair.
The incidence of hydrocephalus requiring shunts in children with myelomeningocele (MMC) is reported to be very high [1]. Previous reports have suggested that 80% to 85% of patients who have a myelomeningocele (MMC) and undergo surgical repair after birth develop hydrocephalus and require the placement of a ventricular shunt [2].
Myelomeningocele (MMC) is a common birth defect that is associated with significant lifelong morbidity. Little progress has been made in the postnatal surgical management of the child with spina bifida. Postnatal surgery is aimed at covering the exposed spinal cord, preventing infection, and treating hydrocephalus with a ventricular shunt. In utero repair of open spina bifida is now performed in selected patients and presents an additional therapeutic alternative for expectant mothers carrying a fetus with MMC. Early fetal intervention may improve neurologic outcome and reduce the hindbrain herniation associated with the Arnold-Chiari II malformation. These changes may improve long-term neurologic function and limit requirements for shunt placements and other surgical interventions. Further research is needed to better understand the pathophysiology of MMC, the ideal timing and technique of repair, and the long-term impact of in utero intervention [3].
In Sudan there is limited number of neurosurgeons and there is only one center to treat all myelomeningocele cases from all over the country. As Sudan is a large country of about 2 million square kilometer and about 30 million population, we frequently see a large number of cases with late presentations either because of difficulties of traveling from the site where they live to our centre or due to financial difficulties facing the families of these patients or because of the long waiting lists. This makes surgical procedures for myelomeningocele repair often difficult and complicated; the anatomical structures can be deformed in complex and unpredictable ways. However the sever lower limb deformities in which the foot is being adherent to the site of myelomeningocele is very rare; to our knowledge and no similar cases have been reported. We report a case of lumbosacral myelomeningocele with congenital hydrocephalus associated with sever bilateral lower extremities deformities the right one is adherent to the site of myelomeningocele with sever flexion deformity of the knee joint and the left one is having congenital talipes equinovarus deformity. The optimum management is being discussed below.
Case report
A 15 months old female child presented to us with increase head size and bilateral lower extremities deformities with the right one is being attached to her back since birth.
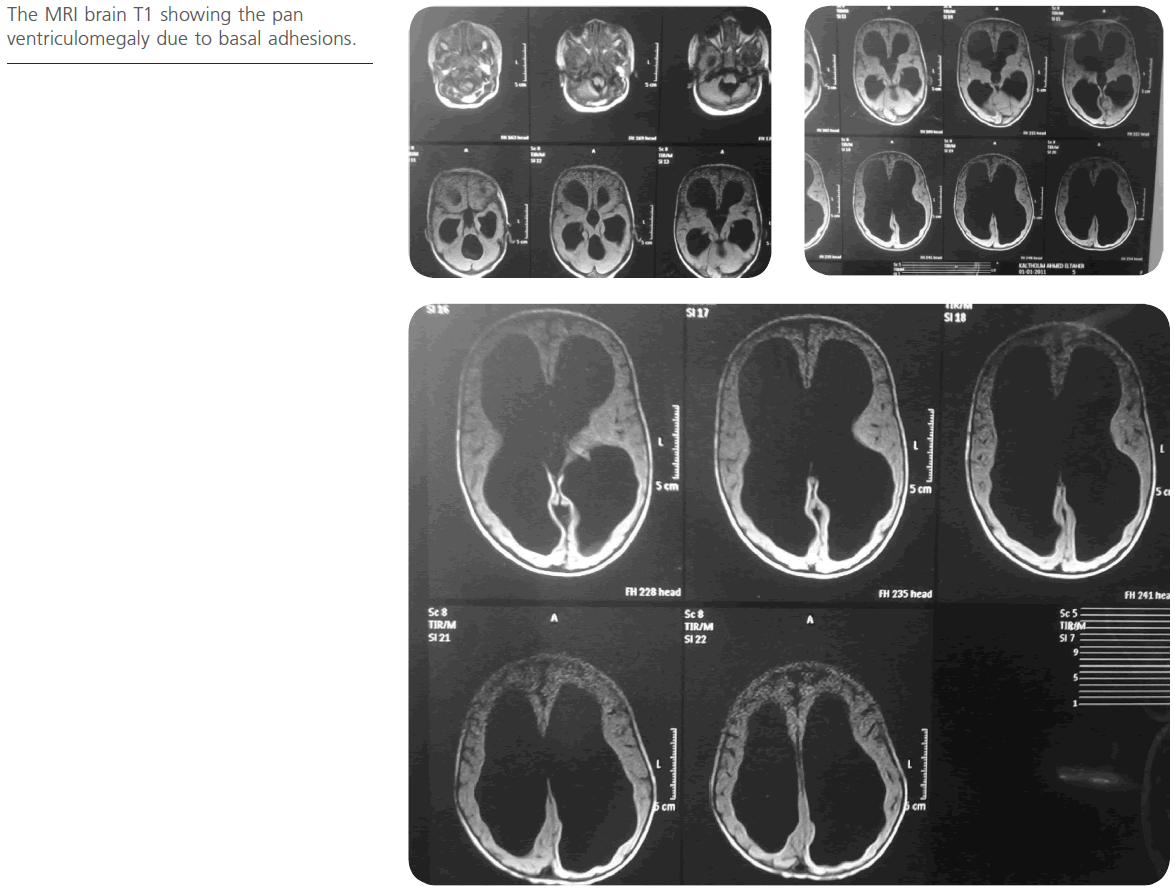
The MRI brain T1 showing the pan ventriculomegaly due to basal adhesions.
She is an outcome of emergency C/S because of failure to progress. Intra-operatively after opening the uterus the fetus was found adherent to the uterine wall by her back which then detached. The baby was post-term, cried and breastfed immediately. Dressing for the back wound was done till it became dry. The baby’s family is from West of Sudan in an area called Abo jibeaha. They have been referred to the National Center of Neurosurgery in Khartoum, but they came late because of financial problems.
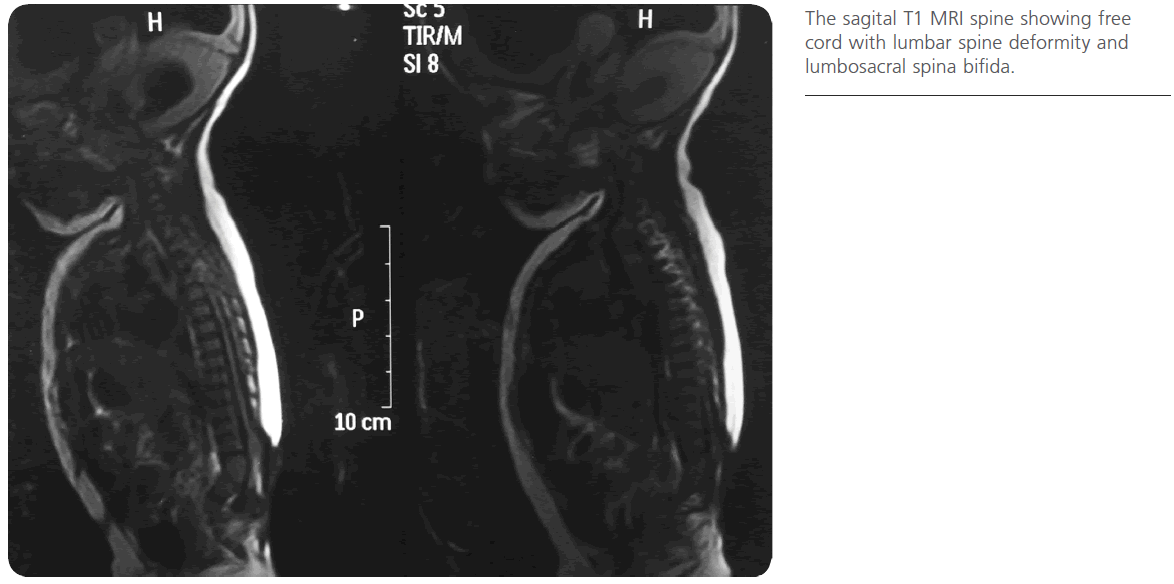
We have seen the patient for the first time in the refer clinic in the third of May 2012 MRI brain and lumbosacral spine requested together with the x-rays for the pelvis and the lower extremities. Images showed pan-ventriculomegaly due to basal adhesions with lower lumbar spine kyphotic deformity, the cord was not fixed and congenital absence of the fibula and patella of the right lower extremity.
The patient admitted for the first time in 14th of May 2012, neurological examination revealed that the patient was fully conscious GCS was 5/5 with large head and widely opened anterior fontanelle. The head circumference was 54 cm in diameter. The back examination revealed dorsolumbar scar with the foot of the right lower extremity firmly attached and adherent to the back just below the scar with mild flexion deformity of the knee joint and talipes equinovarus deformity. The patient can move both lower extremities with good power
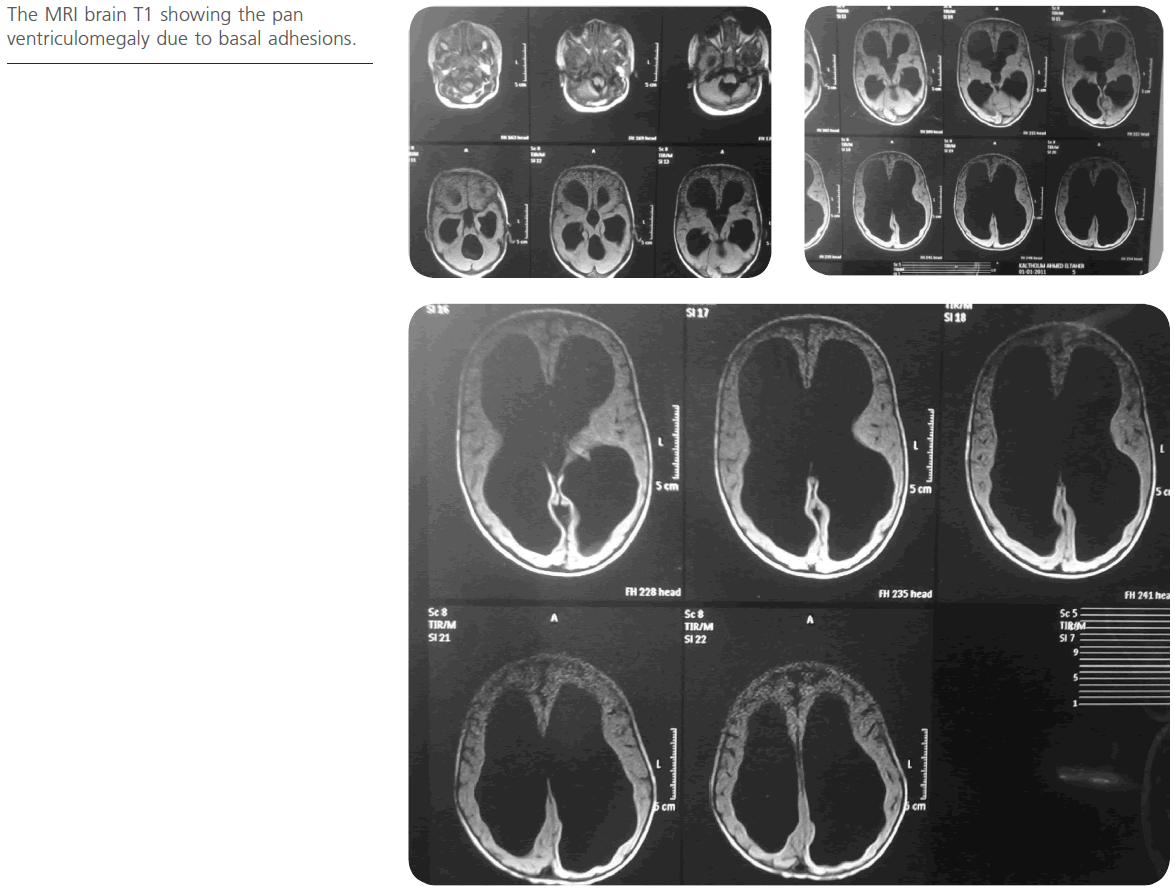
Figure 1:The MRI brain T1 showing the pan ventriculomegaly due to basal adhesions.
The photos of the patient showing the scarred skin at the site of spina bifida and the foot invaginated below it.
The patient was scheduled for ventriculoperotineal shunt first which was done in 16th of May 2012. The patient operated by a medium pressure ventricloperotineal shunt right posterior approach with Chabra shunt system. Postoperative course passed smooth without complications, the patient experienced signs of improvement like depressed anterior fontanelle and becoming more reactive.
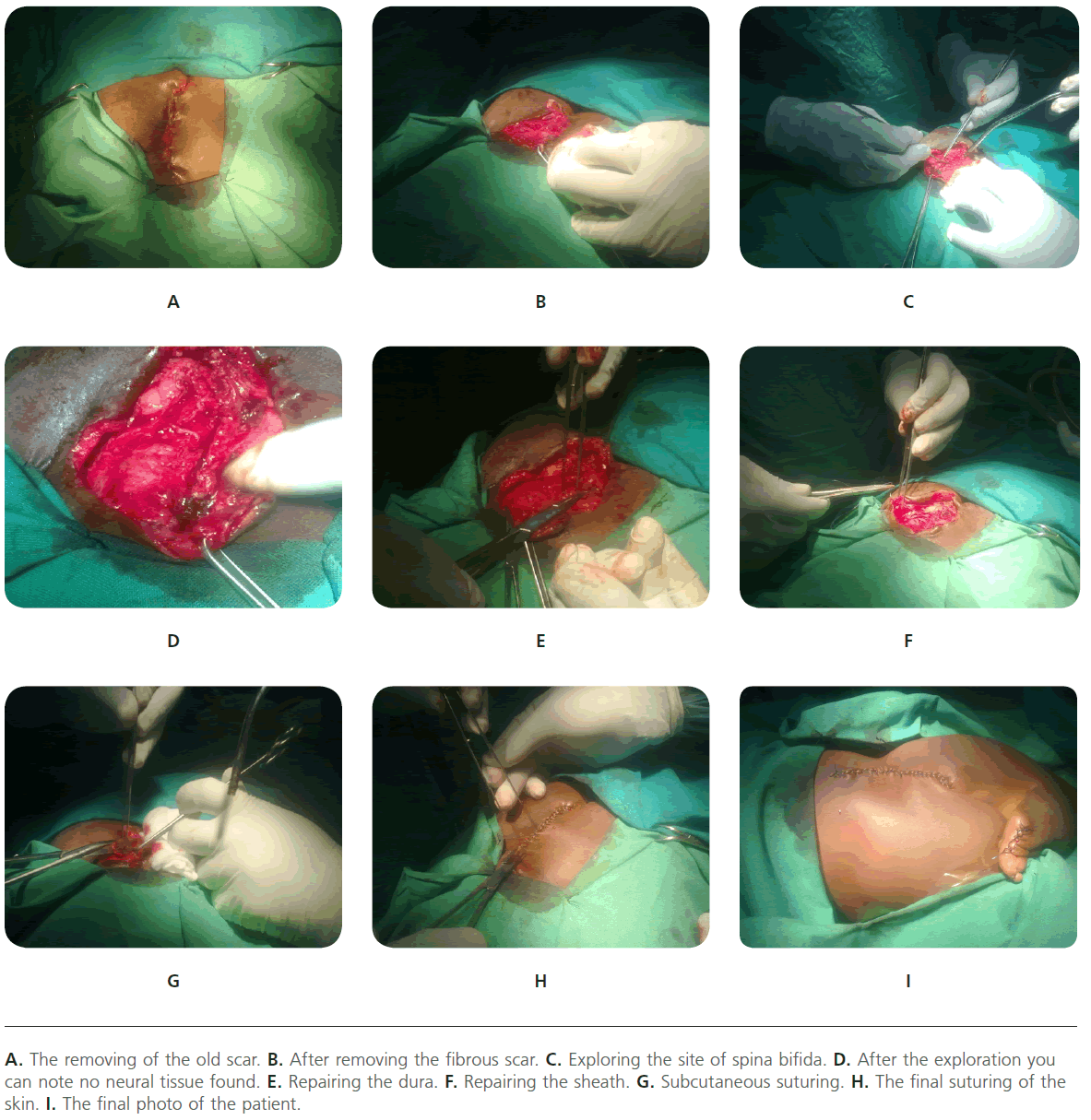
Within the same admission 7 days later the patient underwent the 2nd stage operation which was release of the adherent food and exploration of the site of spina bifida and refashioning of skin. Intra-operatively the foot found to be invaginated between the two buttocks with patent anal orifice and attached to the back by a piece of skin connecting the lateral side of the foot with the back just below the scar. The area of the scar removed first and the area of the spinal defect explored, no neural tissue found which then repaired anatomically with the dura closed first watertight followed with the sheath and the skin closed by the simple undermining technique, tension free closure. The postoperative course passed free and the patient discharged at the 4th postoperative day with oral antibiotics and analgesia.

Figure 2: The Plan X-ray showing the congenital absence of the fibula and the patella.
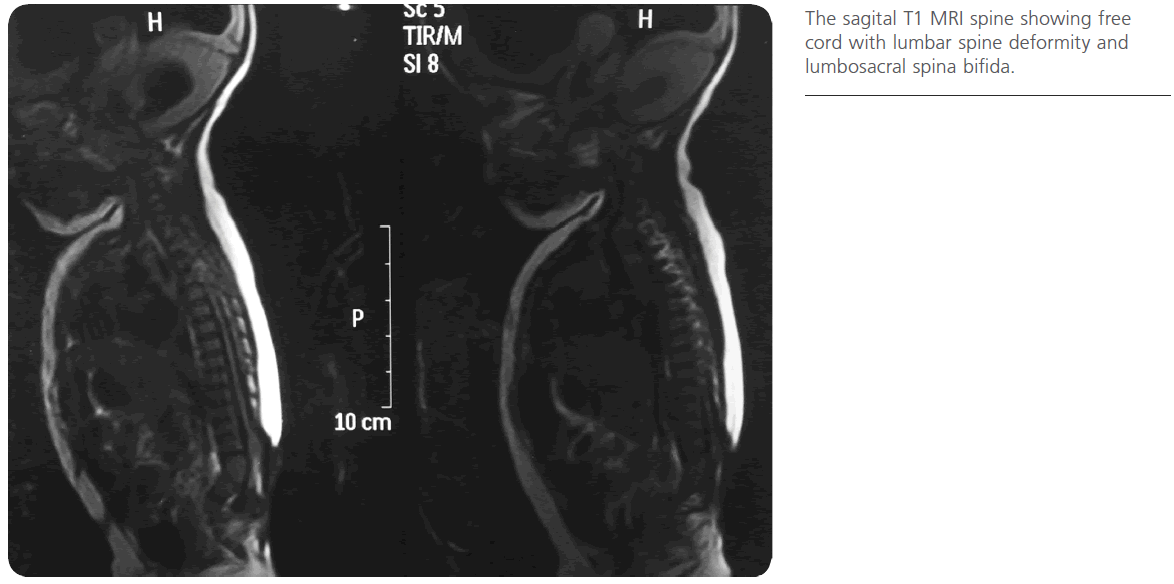
Figure 3: The sagital T1 MRI spine showing free cord with lumbar spine deformity and lumbosacral spina bifida.

Figure 4: Axial T2 MRI spine showing free cord with posterior vertebral arch bony defect.
The patient then referred to the pediatric orthopedics department for her lower extremities deformities.
Discussion
Myelomeningocele is a congenital condition characterized by a protrusion of the meninges and spinal cord through a defect in the posterior part of vertebral column resulting in varying degrees of neurological dysfunction like lower extremities weakness, bowel and bladder dysfunction as well as spinal and lower extremities deformities. Hydrocephalus might associate myelomeningocele whether before or after surgical closure of the defect that might requires the placement of a ventricular shunt to prevent additional mental dysfunction due to cerebral damage.
As myelomeningocele is a common congenital anomaly of the central nervous system worldwide and more in the developing countries and as it is associated with a number of other anomalies of the nervous system beside other unrelated non-neural congenital anomalies, its early and precise surgical management represent a real challenge for all of the neurosurgeons worldwide who might face this condition.
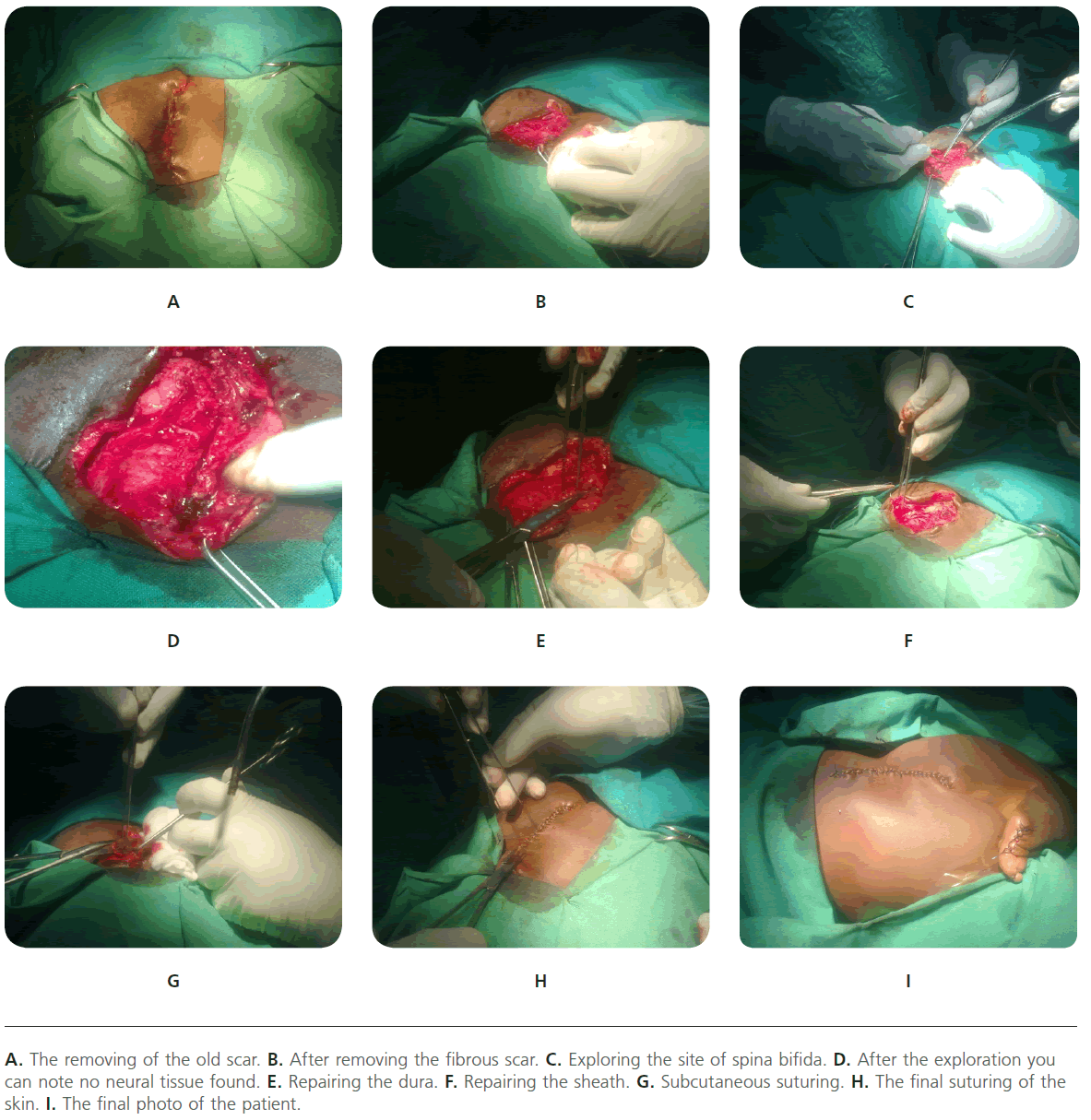
Figure 5: A. The removing of the old scar. B. After removing the fibrous scar. C. Exploring the site of spina bifida. D. After the exploration you can note no neural tissue found. E. Repairing the dura. F. Repairing the sheath. G. Subcutaneous suturing. H. The final suturing of the skin. I. The final photo of the patient.
Timing of shunt insertion in infants with myelomeningocele and hydrocephalus has been debated [4]. However some prefer repairing the MM then observe for the secondary hydrocephalus while others prefer shunt insertion before MM repair.
In our center we used to do the shunt operation first for the associated hydrocephalus then schedule the patient for myelomeningocele operation three to six weeks later. This is because that we think hydrocephalus treatment might be more important so as to prevent further cerebral damage in a patient with irreversible spinal nerves lesion. Also we have noted that placing the V.P. shunt before repair makes the repair much easier with less tension and complications of the wound like dehiscence and CSF leakage or fistula post-repair.
The scenario of this case has proved that in myelomeningocele patients the neurosurgeon can expect any congenital anomalies to take place. Their management needs a multidisciplinary approach to achieve the best outcome and to alleviate the patients suffering as well as the suffering of the parents as those patients grow older.
2076
References
- Adzick, NS., Walsh, DS. Myelomeningocele: Prenatal diagnosis, pathophysiology and management. Semin. Pediatr. Surg. 2003; 12 (3): 168-74.
- Arslan, M., Eseoglu, M., Gudu, BO., Demir, I., Kozan, A. et al. Comparison of simultaneous shunting to delayed shunting in infants with myelomeningocele in terms of shunt infection rate. Turk. Neurosurg. 2011; 21 (3): 397-402.
- Rintoul, NE., Sutton, LN., Hubbard, AM., Cohen, B., Melchionni, J. et al. A new look at myelomeningoceles: Functional level, vertebral level, shunting, and the implications for fetal intervention. Pediatrics 2002; 109 (3): 409-13.
- Sankhla, S., Khan, GM. Reducing CSF shunt placement in patients with spinal myelomeningocele. J. Pediatr. Neurosci. 2009; 4 (1): 2-9.