Keywords
Neuroleptic malignant syndrome; Psychiatry; Autoimmune encephalitis; Emergency medicine; Antipsychotics
Introduction
Though mental illness still remains a stigmatized entity and both awareness and willingness for treatment remain scarce, there is considerable improvement in diagnosis and treatment rates recently. The elderly are more prone to psychiatric illnesses in view of loss of economic and social independence, worsening of physical health, familial discord among many others. Antipsychotics have been increasingly prescribed for conditions like behavioral symptoms of dementia and affective disorders apart from their primary indication being psychotic disorders. In addition, in view of their calming effects, they have been used for many off-label indications like fatigue, anger outbursts, sleep disorders etc. Due to the unchecked and ubiquitous use of these anti psychotics, at inappropriate or excess doses, their adverse effects emerge in a higher number of patients. Neuroleptic Malignant Syndrome is a well described entity and a more serious adverse effect of antipsychotics, but literature about the disease in geriatrics is quite limited. NMS has been associated with most neuroleptics and also with other drugs which interfere in central dopaminergic transmission (dopaminergic antagonists). The common drugs causing NMS are typical neuroleptics like Chlorpromazine, Haloperidol, Fluphenazine, Thioridazine among others, though it can also be caused by atypical antipsychotics like Clozapine, Olanzapine, Risperidone, Quetiapine, and others. Other non-neuroleptics commonly causing NMS include Metoclopramide, Reserpine, tetrabenzene, Droperidol, Amoxapine and Promethazine. Withdrawal of Levodopa and other dopamine agonists and miscellaneous drugs like Lithium, Phenelzine and Dosulepin may cause the disease. The diagnosis of NMS promptly is very essential because, treatment is quite effective and may prevent major complications including death. The close differentials are wide ranging from infections like meningitis and brain abscess to metabolic conditions and environmental like heat stroke, to other drug induced entities like Malignant Hyperthermia, Serotonin Syndrome and anticholinergic toxicity, drug withdrawal syndomes and neuropsychiatric conditions like Parkinsonism, Malignant catatonia and Autoimmune encephalitis and polymyositis. Here we present our case report of NMS which developed in a 69 year old woman, on 200mg Quetiapine for Bipolar Affective disorder, which has many rare and atypical features and how we diagnosed and treated the disease.
Case Report
A 69-year-old lady, belonging to a rural background in North India, educated up to primary school and living with her son and his family, presented to the Emergency with a 10 day history of generalized weakness and fatigue followed by vomiting and trembling of hands for the past week, and fever for the past 5 days. She was initially admitted outside with headache and seizures and was treated with anti-epileptics and discharged. Fever was documented up to 101°F, with 2-3 spikes per day. She also developed rigidity of the body for the past 2 days, to the extent that she was unable to move her limbs. Over the next one day she developed altered sensorium in the form of irrelevant talk and inability to identify relatives along with confusion.
On detailed history taking, it was found that she had been diagnosed as Bipolar Affective disorder 4 years ago, for which she was on desi or herbal medication for the initial 3 years, with nil to poor control of symptoms. However, in view of increasing frequency and severity of the manic episodes, she was taken to a psychiatrist in her town, when she was prescribed Quetiapine, at a starting dose of 100 mg per day. Since her manic state persisted, the dose of Quetiapine was upgraded to 200 mg per day. Within 2 weeks of dose increase, she developed the symptoms of NMS.
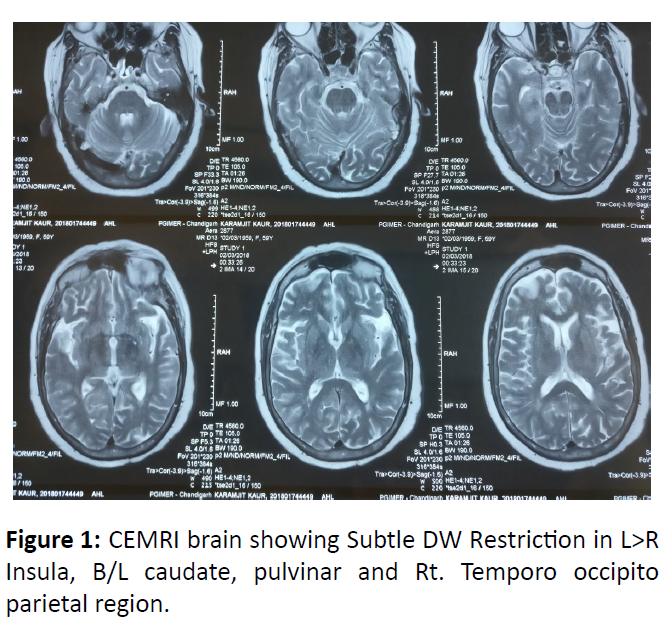
Initially, at the emergency setting, the differential diagnoses considered were metabolic encephalopathy, acute meningoencephalitis, and autoimmune encephalitis. However in view of use of psychotropic drugs and in recent increase in dose, in combination with the array of symptoms at presentation, other disorders like NMS and malignant catatonia were considered. On admission to the emergency ward she was found to be febrile with temperature of 101.4°F, with coarse tremors of all four limbs, was diaphoretic, with tachycardia of 120-130/min and fluctuating BP of 140/100 mm Hg to 100/70 mm Hg, and she was morbidly obese. Physical examination of CVS, respiratory, and abdomen did not reveal any abnormality. In the central nervous examination, there was hypertonia and both the superficial and deep tendon reflexes were absent. On the basis of available history and examination findings, the differential diagnoses of NMS, malignant catatonia and encephalopathy were considered. All the psychotropic medications were discontinued. On examining her mental status, she was drowsy and had irregular and infrequent episodes of delirious and irrelevant talk. There was no history of cough with expectoration, urinary system, heat exposure, abdominal discomfort, diarrhea, use of any other drugs, or any substance of abuse. Laboratory investigations showed a hemoglobin of 9.6 g/dL, total leukocyte count to be 14,400/uL and platelet count of 203,000/mm3. Chest X-Ray, electrocardiogram, and cerebrospinal fluid evaluation did not reveal any abnormality. However CEMRI brain revealed Subtle DW restriction in Left>Right Insula, Bilateral caudate, pulvinar and Right Temporo-occipito parietal region suggestive of auto immune encephalitis (Figure 1).
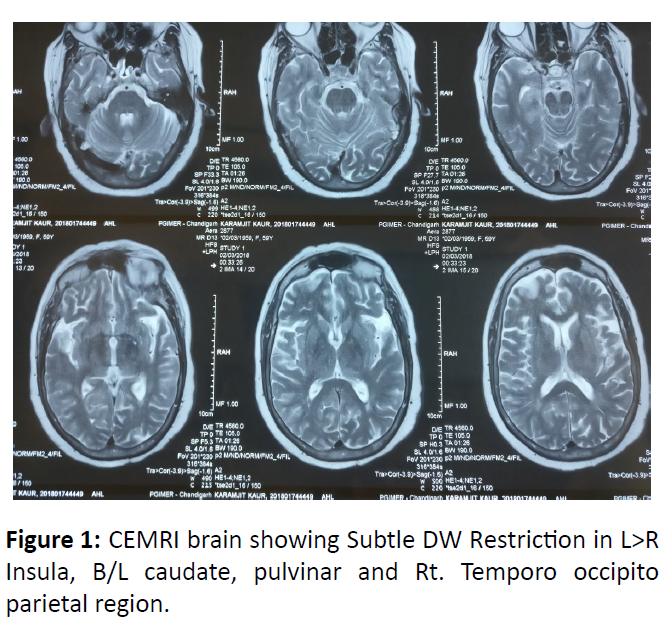
Figure 1: CEMRI brain showing Subtle DW Restriction in L>R Insula, B/L caudate, pulvinar and Rt. Temporo occipito parietal region.
In view of this finding, her auto immune encephalitis workup was sent which included Anti-NMDA, Anti-LG1, Anti- AMP1, AMPA2, Anti-GABAB receptor antibodies which came out to be negative. Creatinine phosphokinase levels were found to be 62 U/L (Normal range being 25-130 U/L). Her cultures, blood fluid examination, including urine and sputum examination, serum electrolytes, renal functions, evaluation for tropical illnesses like dengue and malaria and arterial blood gas analysis did not reveal any abnormality. Adding all the available information to her presentation and clinical examination, a possible diagnosis of NMS was considered. She was started on Bromocriptine 2.5 mg QID (4 times a day) along with continuation of supportive management. Within 2 days of initiation of therapy, her condition began to improve and within 5 days she was asymptomatic. She did not develop any complications and was discharged within a week from the emergency. No psychotropics were started at the time of discharge and she was advised to followup in the psychiatry department as an outpatient.
Discussion
NMS is a very severe idiosyncratic reaction to anti-psychotic agents, characterized by the typical tetrad of fever, rigidity of muscles, altered sensorium and autonomic imbalance [1]. Various diagnostic criteria used for its diagnosis are DSM V and Levenson’s criteria [2]. While Levenson’s criteria holds raised CPK as a major criteria, it’s not so with DSM V [3]. Our patient fit the criteria for NMS by both definitions. Laboratory evaluation may show leukocytosis and elevated serum creatine phosphokinase levels. In many cases, the initial symptoms are only partial and the full blown clinical syndrome develops in 1-2 days. This patient was atypical in more ways than one. She was an old female, NMS being more common in males [4]. She had a staggering course where her symptoms developed over a period of 1 week to 10 days. The next rarity was a normal level of CPK, which is almost always elevated in NMS [5]. Quetiapine being a newer anti-psychotic was considered low risk of causing NMS, and there are only a very few case reports of NMS with Quetiapine [6]. Over the years, many factors have been identified to be associated with the development of the disease, some of which include poor nutrition, being abandoned, underweight, old age, multiple co-morbid illnesses, neuroleptics through parenteral routes, sudden dose elevations, head trauma, dementia, male gender, alcohol ingestion, HIV, and concomitant use of lithium and anticholinergics [7]. 1st generation neuroleptic agents have a greater propensity to cause NMS, though newer anti psychotics can cause NMS too especially in male patients with baseline H/O dehydration, confusion or delirium and erratic dose changes [8]. An early suspicion of the disorder is necessary in making differentials because of two reasons; one being the fact that there are many close differentials for the same and the other reason is that treatment is simple and effective [9]. The index case did not have many of the common predisposing factors, which makes it another atypical feature. Another confusing point in this patient’s management was the clinical symptoms fitting into the picture of autoimmune encephalitis along with imaging suggestive of the same, yet she had more features and the clinical setting pointed more towards NMS and she responded to the treatment, which was wonderfully effective for the same. We followed her up for 1 year with no recurrence of symptoms. The older population has more precipitating factors like other comorbidities, dehydration, multiple medications, brain diseases etc. [10].
Conclusion
Through this case report we would like to highlight that any patient could develop NMS even without any of the typical predisposing factors and the diagnostic dilemma we faced between NMS and Autoimmune encephalitis.
32855
References
- Khouri C, Planès S, Logerot S, Villier C, Mallaret M (2016) Case report: Neuroleptic malignant syndrome and diagnostic difficulties. Encephale 42: 277-280.
- Ambulkar RP, Patil VP, Moiyadi AV (2012) Neuroleptic malignant syndrome: A diagnostic challenge. J Anaesthesiol Clin Pharmacol 28: 517-519.
- Suraweera C, Hanwella R, De Silva V (2016) Second generation antipsychotics causing neuroleptic malignant syndrome. Sri Lanka J Psychiatry 7: 20.
- Nielsen RE, Wallenstein Jensen SO, Nielsen J (2012) Neuroleptic malignant syndrome-An 11-year longitudinal case-control study. Can J Psychiatry 57: 512-518.
- O'Dwyer AM, Sheppard NP (1993) The role of creatine kinase in the diagnosis of neuroleptic malignant syndrome. Psychol Med 23: 323-326.
- Woods G, Taggart C, Boggs R, Cadden I (2013) Neuroleptic malignant syndrome associated with quetiapine and venlafaxine use: A case report and discussion. Ther Adv Psychopharmacol 3: 53-55.
- Jeffrey RS, Paul EK, Stanley NC (2007) Neuroleptic malignant syndrome. American Journal of Psychiatry 164: 870-876.
- Khaldi S, Kornreich C, Choubani Z, Gourevitch R (2008) Neuroleptic malignant syndrome and atypical antipsychotics: A brief review. Encephale 34: 618-624.
- Berman BD (2011) Neuroleptic malignant syndrome: A review for neurohospitalists. Neurohospitalist 1: 41-47.
- Feng Y, Yang X, Huang Y (2013) Two cases of neuroleptic malignant syndrome in elderly patients taking atypical antipsychotics. Shanghai Arch Psychiatry 25: 178-182.