Vikram VK*
ACPM Medical College, Nagpur, Maharashtra, India
*Corresponding Author:
Vikram Vilasrao Kadu
Acpm Medical College
Orthopaedics, Kadu House
Friends Colony, Nagpur
Maharashtra 440013, India
Tel: +91-8554917127
E-mail: vikram1065@gmail.com
Citation: Vikram VK. Neuropathic Shoulder Joint Due to Syringomyelia of Cervical Spine – A Case Report. J Neurol Neurosci. 2016, 6:3. doi: 10.21767/2171-6625.100027
Received Date: September 11, 2015; Accepted Date: November 10, 2015; Published Date: November 14, 2015
Keywords
Neuropathic arthropathy; Syringomyelia; Shoulder
Introduction
Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in pain, paralysis, weakness [1], and stiffness in the back, shoulders, and extremities. Syringomyelia has a prevalence estimated at 8.4 cases per 100,000 people [2] with symptoms usually beginning in young adulthood.
Case Presentation
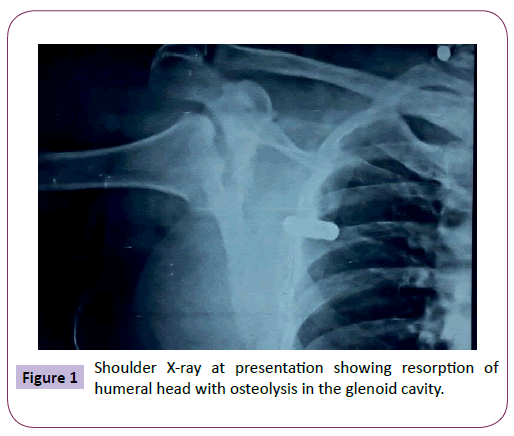
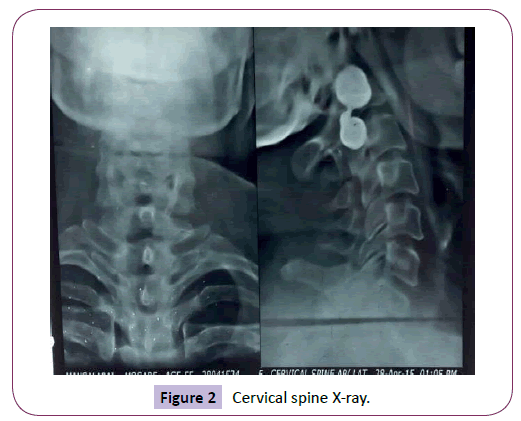
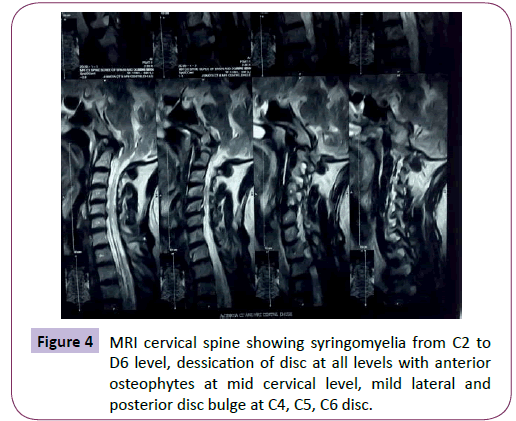
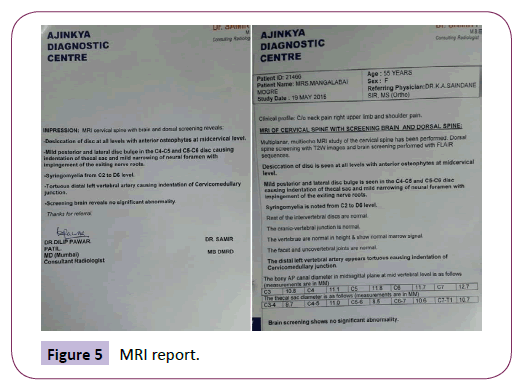
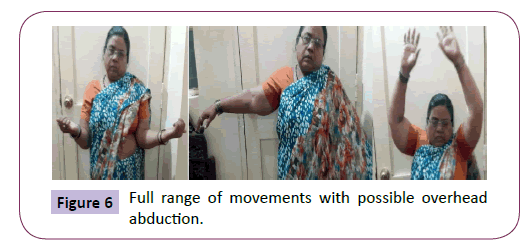
45 yrs old female presented to OPD with pain over nape of neck radiating to right shoulder. Clinically the movements of right arm were restricted. The patient was investigated in the form of cervical spine and shoulder X-ray. Shoulder X-ray showed destroyed joint (resorption of humeral head with osteolysis in the glenoid cavity) (Figure 1). Cervical spine X-ray (Figure 2) showed pathology at C4, C5 and C6 levels. Meticulous history and examination [restricted movements of neck, pain radiating to right shoulder and right upper limb, tingling numbness in right upper limb, deep tendon jerks were absent in right upper limb, power 2/5 at right shoulder joint, elbow flexors 4/5, wrist 5/5] suggested spinal involvement and trauma previously. Lumbar spine X-ray (Figure 3) was advised which showed reduction in joint space. Patient was further investigated in the form of cervical spine MRI (Figure 4) with screening whole spine. MRI was suggestive of syringomyelia from C2 to D6 level, dessication of disc at all levels with anterior osteophytes at mid cervical level, mild lateral and posterior disc bulge at C4,5,6 disc, tortuous distal left vertebral artery causing indentation of cervicomedullary junction (Figure 5). The other joints were examined but were normal without any neurodeficit. The patient was treated conservatively by assuring not to do strenuous activities in order to protect from further trauma to the joint for 6 weeks. Patient now has got full range of movements of the arm (Figure 6).
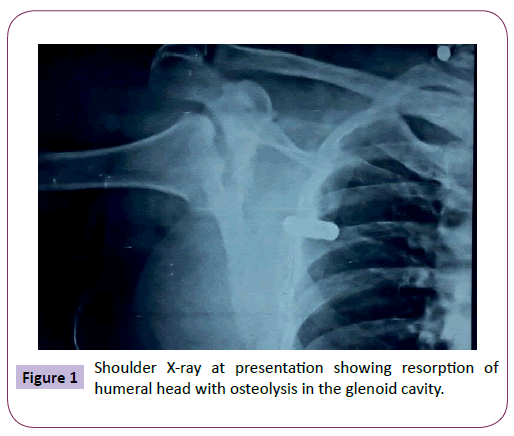
Figure 1: Shoulder X-ray at presentation showing resorption of Figure 1 humeral head with osteolysis in the glenoid cavity.
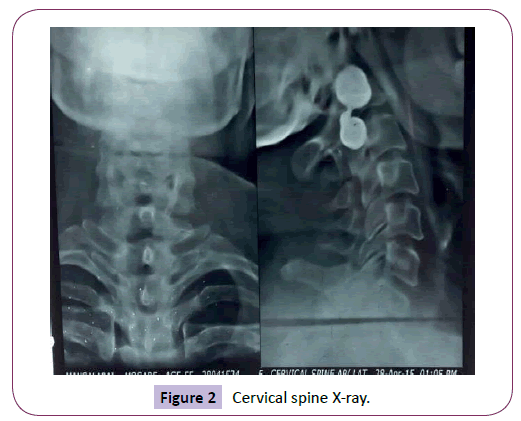
Figure 2: Cervical spine X-ray.
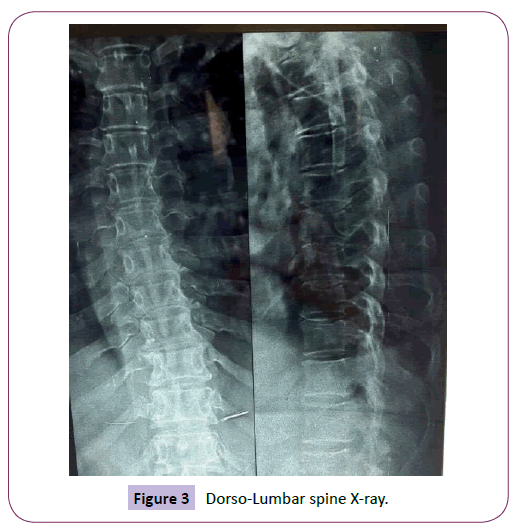
Figure 3: Dorso-Lumbar spine X-ray.
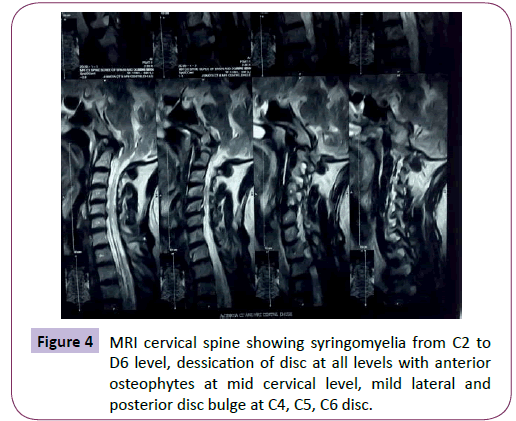
Figure 4: MRI cervical spine showing syringomyelia from C2 to D6 level, dessication of disc at all levels with anterior osteophytes at mid cervical level, mild lateral and posterior disc bulge at C4, C5, C6 disc.
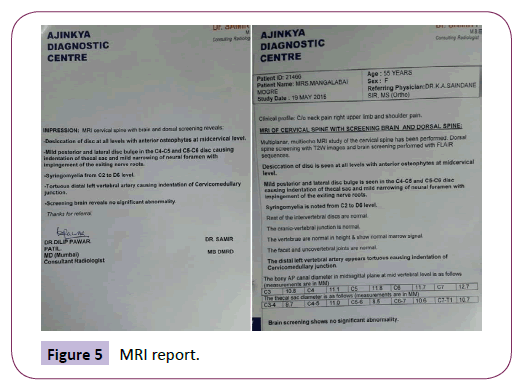
Figure 5: MRI report.
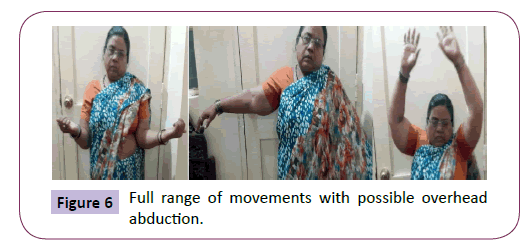
Figure 6: Full range of movements with possible overhead abduction.
Discussion
Neuropathic arthropathy, also known as Charcot joint, is a destructive situation resulting from decreasing or loss of proprioception, pain, and temperature sensation [3]. Various etiologies include: syringomyelia (25%), diabetes mellitus (0.16– 2.5%) and tabes dorsalis (5–10%) [4]. Shoulders and elbows are commonly involved in syringomyelia, hips and knees in tabes dorsalis, and ankles and feet in diabetes mellitus [5].
Syringomyelia leads to interruption of lateral spinothalamic tract, dorsal column fibers, anterior horn cells and sympathetic pathways sequentially leading to loss of joint sensation [6]. Symptoms related to shoulder frequently precede or overshadow neurological deficits. Onset of symptoms may be acute with neck and shoulder pain. The atrophic form of neuropathic arthropathy usually affects non-weight bearing joints such as shoulder, elbow and wrist with severe destruction rapidly, sometimes in less than 6 weeks [7].
Syringomyelia is a disorder involving a fluid-containing cavity (syrinx) within the spinal cord. These cavities commonly occur in the lower cervical and upper thoracic segments, and the distension may propagate proximally. Causes of syringomyelia include congenital, traumatic, infectious, degenerative, vascular, or tumor-related [8-11]. MRI is the most effective imaging modality for visualization of a syrinx.
The pathophysiology of syringomyelia involves the disruption of the adjacent gray and white matter. The initial fibers damaged are the pain and temperature sensory fibers as they cross the midline. Their loss in the upper extremity, with intact position sense and motor function, is often the first clinical sign. It is the loss of these sensory fibers that is thought to result in the etiology of neuropathic arthropathy of the shoulder. As the syrinx grows or propagates, the dorsal column fibers or anterior horn cells may be affected. Areflexia, muscle weakness, and atrophy results, commonly involving the hand intrinsics.
Conclusion
Neuropathic arthropathy of the shoulder is rare, and if not evaluated carefully can be misdiagnosed. Considering only the involving joint tumor is the most common diagnosis if proper neurological and physical examination is not done.
Clinical Message
Neuropathic arthropathy of the shoulder is rare, and correct diagnosis is possible by careful physical and neurological examination and pathologic evaluation when needed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in- Chief of this journal.
Competing Interests
The authors declare that they have no competing interests.
Conflict of Interest
None
Financial support
No financial support was received for this study.
Authors Contribution
KS analyzed and treated the patient and contributed in writing the manuscript. VK collected the data and wrote the manuscript along with NG. All the authors read and approved the final manuscript.
7355
References
- "Neurosurgical considerations in posttraumatic syringomyelia-Home Study Program" (2003). AORN Journal.
- Brewis M, Poskanzer DC, Rolland C (1966) "Neurological disease in an English city". ActaNeurologicaScandSuppl 24: 1-89.
- Johnson JT (1967) “Neuropathic fractures and joint injuries. Pathogenesis and rationale of prevention and treatment,” Journal of Bone and Joint Surgery A 49: 1-30.
- Jones J, Wolf S (1998) Neuropathic shoulder arthropathy (Charcot joint) associated with syringomyelia. Neurology 50: 825-827.
- Shapiro G, Bostrom M (2001) Heterotopic ossification and Charcot neuroarthropathy. In: Chapman MW, editor. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams and Wilkins 3245 62.
- Mancall ES (1984) In: Rowland LP, editor. Merritt's textbook of neurology. Philadelphia: Lea and Febiger 552-556.
- Brower AC, Allman RM (1981) Pathogenesis of the neurotrophic joint: Neurotraumatic vs. neurovascular. Radiology 139: 349-354.
- Brodbelt AR, Stoodley MA (2003) Post-traumatic syringomyelia: a review. J ClinNeurosci 10: 401-408.
- Klekamp J (2002) The pathophysiology of syringomyelia – historical overview and current concept. ActaNeurochir (Wien) 144: 649-664.
- Biyani A, el Masry WS (1994) Post-traumatic syringomyelia: a review of the literature. Paraplegia 32: 723-731.