Keywords
Obstructive sleep apnoea, Lateral cephalometric, Cranio-facial
Introduction
Obstructive Sleep Apnoea Hypopnoea Syndrome (OSAHS) is associated with an increased risk of cardiovascular disease and stroke, and there is a strong suspicion that untreated sleep disordered breathing precipitates greater mortality [1].
The disorder affects 4-7% of the general adult population [2]. Owing to its prevalence, it is currently considered a major public health concern, with severe physical and social consequences if not properly treated [2,3] (Figure 1).
Figure 1: Etiology of OSAHS.
These disorders affect mainly middle-aged patients that are professionally active and may generate high losses and absences from work [4]. Medical costs of OSAHS may be significantly reduced when effective diagnosis and treatment are performed early [5]. However, the increasing demand for apnoeic diagnosis has begun to place strain upon services based on overnight laboratory studies. This situation has been clearly reflected at the Edinburgh Sleep Clinic where new referrals for polysomnography testing were found to have increased tenfold between 1990 and 1996 [6].
Evidence suggests that the discrepancy between demand and available resources is steadily widening. The development of alternative diagnostic methods would therefore appear to be a worthy goal, and indeed this subject has received a great deal of attention within the recent literature.
Differences in cranio-cervico-facio morphology in the OSAHS subjects as compared to their ‘normal’ counterparts has been a consistent finding and more recent investigations have aimed to prove the existence of a relationship between cranio-cervicofacial morphology and severity of the OSAHS condition [7]. Evidence has been equivocal, and although a number have been suggested a correlation, none have yet converted this into a tool of clinical diagnostic significance.
Decreased cranial base length is a consistent finding of cephalometric studies of OSAHS subjects [8]. As a logical consequence, the lengths of the maxilla and of the bony pharynx are diminished. These measurements are confirmed by Battagel [9], who suggests a mean decrease in cranial base length of some 2.4 mm and identifies a consequential of the antero-posterior dimensions of the cranium with subsequent ‘Retrusion of the face’.
Bimaxillary retrusion or retrognathia of the mandible alone has been reported in up to 42% of subjects in a number of OSAHS investigations [10,11], and recent work has shown significant reductions in mandibular length gonion to menton (Go-Me) reduction of up to 5.9 mm, and even variations among mandibular plane inclinations are accounted for similar results were obtained [9]. Other studies have shown no indication of this trait and we must accept that while a decrease in mandibular body length has often been described, this does not appear to be a universal finding [12].
Decrease in mandibular body length has been reported [13]. A more recent study found reduced mandibular body length (Go- Me) by 5.9 mm in the OSAHS group P = 0.002 [9]. Recording this distance in the horizontal plane, to take into account variations in mandibular plane inclination, the same differences were found. Go-Me was 6.6 mm shorter and (Go-point B) 5.6 mm less in apnoeic individuals [9].
Bacon et al., Tsuchiya et al., and Lowe et al., [8,11,14] found that there is increase in the lower facial height with concomitant increase in the maxillo-mandibular planes angle.
The linear measurement Hyoid bone position is proposed to be of clinical value in terms of its application in diagnostic triage and subsequent management decisions [15].
Lateral cephalometric radiographs have been used by several investigators in an attempt to identify morphological parameters that might be characteristic of OSAHS.
The aim of this study is to determine if there are significant differences in cranio-facio-hyoid morphology between the OSAHS and the controls and to suggest possible skeletal morphology for the OSAHS patients.
Materials and Methods
The material for this study comprised the anomaly group, control group, cephalogram, lateral cephalometric films, computer and software, x-ray viewer, and the accessories. The sample of the anomaly and the control were not restricted in any way by malocclusion but it was decided that due to the nature of the variables chosen, subjects would all be dentate. This was to maintain standard cephalometric tracing in all subjects.
Subjects
All subjects were previously diagnosed with OSAHS by polysomnographic diagnostic sleep studies (Edinburgh Sleep Laboratory) before presenting to the orthodontic clinic. The group consisted of 65 white Caucasian male adults’ and their age ranged between 40-65 years. Subjects had not undergone any surgery for the treatment of OSAHS. The control subjects were asked if they had ever been known to snore. This was verified whenever possible by a sleeping partner. The group consisted of 30 white Caucation male adults’ between 20-30 years, matched for race and sex to the anomaly group; all subjects were in good medical health and did not suffer from any airway disease.
Materials and measurements
All the lateral cephalograms were taken using a Siemans Orthophos CD at the Royal Infirmary of Edinburgh Radiography Department which has a cephalostat with intensifying screen and motorizes adjustable grid. The KVP (peak kilo-voltage) was adjusted to optimise the contrast of both hard and soft tissues. The distance from the focus to the median plane was (60 inches) and from the median plane to the film was 12 inches [16]. The subject was standing upright with ‘natural’ head position that is the ‘natural’ posture of the head when standing with the visual axis being horizontal [17]. Such a standardized position has been investigated by Solow et al., [18] who provided a detailed description of the method. Initially the subject assumes the “orthoposition” defined as the ‘intention’ position from standing to walking [19]. The median plane parallel to the film with the maximal intercuspation of the teeth and lips in light contact, and in natural head position [20]. A possible lateral head tilt or rotation was prevented by means of a cross-light beam projected onto the face and finally, the bilateral ear rods were gently inserted onto the external part of the auditory meatus to stabilize the headposture during exposure. All lateral cephalograms were taken before any medical or surgical intervention.
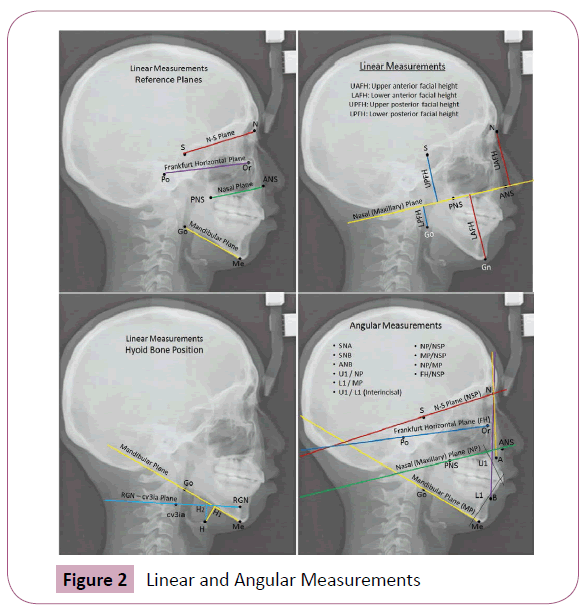
Radiographs were traced, oriented with the maxillary plane horizontal and skeletal points identified (Figure 2). Definitions of the landmarks are given in (Table 1). Points were digitized twice (one week interval) in a predetermined sequence to a tolerance of 0.2 mm and the mean value taken.
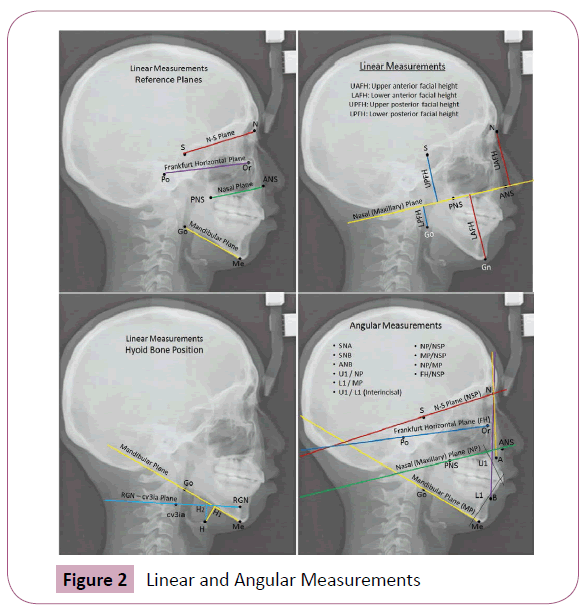
Figure 2: Linear and Angular Measurements
The reference points and lines used in this research are given in Table 1. The definitions are taken from [21-23]. Some unfamiliar landmarks, planes and measurements which are not described in these papers are described and explained in details.
The
Landmarks |
Definition |
| N |
Nasion:The most anterior point of the fronto-nasal suture. |
| S |
Sella:The midpoint of the sella tursica. |
| Or |
Orbitale:The deepest point on the infra-orbital margin. |
| Po |
Porion: The uppermost, outermost point on the bony external auditory meatus |
| ANS |
Anterior Nasal Spine:The tip of the anterior nasal spine. |
| PNS |
Posterior Nasal Spine:The tip of the posterior nasal spine. |
| Gn |
The most antero-inferior point of the mandibular symphesis. |
| Me |
Menton: The lower most point on the mandibular symphesis in the midline |
| Go |
Gonion: The intersection of the line connecting the most distal aspect of the condyle to the distal border of the ramus and the mandibular plane. |
| RGN |
The most infero-posterior point on the mandibular symphesis. |
| cv3ia |
The infero-anterior point of the body of the third cervical vertebra. |
| H |
The upper edge of the frontal area of hyoid body. |
| H1 |
Perpendicular from H to the mandibular plane (Go-Me) |
| H2 |
Perpendicular from H to the line RGN-cv3ia |
| U1 |
Long axis of the upper incisors |
| L1 |
Long axis of the lower incisors |
| Linear Measurements |
Definition |
| NSP |
Nasion Sella Pine: The line throughpoints N and S. |
| FHP |
Frankfurt Horizontal Plane: The line through point Or and Po. |
| NP |
Maxillary Plane: The line connecting ANS with PNS. |
| MP |
Mandibular Plane: The line connecting Me to Go. |
| UAFH |
Upper Anterior Facial Height: perpendicular from N to the Max P. |
| LAFH |
Lower Anterior Facial Height: perpendicular from Me to the Max P. |
| UPFH |
Upper Posterior Facial Height: perpendicular from S to the Max P. |
| LPFH |
Lower Posterior Facial Height: perpendicular from Go to the Max P. |
| OJ |
Overjet: The horizontal distance between the palatal surface of the most proclined upper incisor to the labial surface of the lower incisors. |
| OB |
Overbite: The vertical overlap of the lower anteriors by the upper anteriors. |
| H - H1 |
The linear distance along a perpendicular from hyoid (H) to the Mandibular plane. |
| H - H2 |
The linear distance between hyoid (H) and a perpendicular to the cv3ia-RGN plane. |
| (H - H1) + (H - H2) |
Vertical Hyoid Position. |
| Angular Measurements |
Definition |
| NP / NSP |
The angle between the nasal plane and Nasion-Sella plane. |
| MP / NSP |
The angle between the mandibular plane the Nasion-Sella plane. |
| NP / MP |
The (Nasal) maxillary mandibular plane angle. |
| FHP / NSP |
The angle between Frankfurt horizontal and Nasion-Sella plane. |
| SNA |
Sella-Nasion-A point. |
| SNB |
Sella-Nasion-B point. |
| ANB |
Point A - Nasion - Point B. |
| U1 / NP |
Long axis of the upper incisors to the (Nasal) Maxillary plane. |
| L1 / MP |
Long axis of the lower incisors to the Mandibular plane. |
| U1/L1 |
The angle formed with long axis of upper and lower incisors. |
Table 1: The Landmarks, Linear and Angular Measurements.
Statistical analysis
Statistical software: SPSS for windows version 14.0 (Norusis MJ), [Prentice-Hall Inc., A Simon & Schuster Company, Upper Saddle Drive, New Jersey, USA]. Descriptive statistics was used to describe the different variables. T-test and coefficient of correlation were used to test the different and association between two variables respectively. For the entire tests 0.05 was used as level of significant.
Results
Demographic outcomes
Sixty five patients and 30 healthy controls were participated in this study. The median age of the OSAHS was 47.5 with range (40-65), while the median age among the healthy group was 23.7 and range (20-30) years.
Body Mass Index (BMI)
The median BMI for the OSAHS group was 27.5 (range, 24.9- 44.6), and for the controls the median was 23. (range, 21.8-27.7), which is highly significance (p=0.001). This shows that OSAHS is significantly related to obesity (increase in the BMI).
Linear measurements
Among the twelve variables studied the result was presented in Table 2, that shows the average of the anatomical lines (Gn- NP, Go-NP) were higher among OSAHA 68.39 (SD 7.4) and 36.2 (SD 5.98) compared with controls 62.6 (SD 5.27) and 32.89 (SD 5.09) with p-value 0.002 and 0.01 respectively, which indicates increased lower anterior and posterior facial heights more downward facial growth pattern. In addition the average of the ANS-PNS was lower in the OSAHS 54.26 (SD 4.99) compared with controls 57.57 (SD 3.36) with p-value 0.0013, which indicates shortened maxilla among the cases. It was also found that the vertical hyoid position [(H-H1) + (H-H2)] was higher in the OSAHS 34.79 (SD 11.48) compared with controls 27.25 (SD 10.06), which indicates inferiorly positioned hyoid bone among the OSAHS group. There were statistically linear associations between most of linear measurements except for the measurement of overbite and overjet, as shown in Table 3.
| Linear Measurements |
| Variables |
Group |
Mean |
Std.
Deviation |
N |
Pvalue |
| N – NP |
control |
53.73 |
2.67 |
30 |
0.7964 |
| sample |
53.95 |
4.121943 |
65 |
| Gn – NP |
control |
62.60 |
5.27 |
30 |
0.0002 |
| sample |
68.39 |
7.40 |
65 |
| S – NP |
control |
42.87 |
3.55 |
30 |
0.3741 |
| sample |
43.60 |
3.79 |
65 |
| Go – NP |
control |
32.88 |
5.09 |
30 |
0.010 |
| sample |
36.20 |
6.00 |
65 |
| N – S |
control |
73.43 |
3.32 |
30 |
0.9141 |
| sample |
73.35 |
4.06 |
65 |
| ANS – PNS |
control |
57.58 |
3.36 |
30 |
0.0013 |
| sample |
54.26 |
5.00 |
65 |
| Go – Me |
control |
74.38 |
5.70 |
30 |
0.400 |
| sample |
73.21 |
6.55 |
65 |
| OB |
control |
3.47 |
2.11 |
30 |
0.4224 |
| sample |
3.93 |
2.81 |
65 |
| OJ |
control |
3.42 |
2.65 |
30 |
0.8612 |
| sample |
3.32 |
2.60 |
65 |
| H – H1 |
control |
18.58 |
4.72 |
30 |
0.002 |
| sample |
22.88 |
6.51 |
65 |
| H – H2 |
control |
8.67 |
6.00 |
30 |
0.011 |
| sample |
12.21 |
6.23 |
65 |
| (H-H1)+ (H-H2) |
control |
27.25 |
10.06 |
30 |
0.003 |
| sample |
34.79 |
11.49 |
65 |
| AngularMeasurements |
| NP/NSP |
control |
8.78 |
2.42 |
30 |
0.6005 |
| sample |
8.41 |
3.60 |
65 |
| MP/NSP |
control |
36.35 |
6.43 |
30 |
0.9138 |
| sample |
36.20 |
6.19 |
65 |
| NP/MP |
control |
26.72 |
6.77 |
30 |
0.2546 |
| sample |
28.34 |
6.24 |
65 |
| FHP/NSP |
control |
8.10 |
3.92 |
30 |
0.8322 |
| sample |
8.25 |
3.17 |
65 |
| SNA |
control |
76.25 |
18.99 |
30 |
0.0231 |
| sample |
82.31 |
6.46 |
65 |
| Sqrt SNB |
control |
8.77 |
0.21 |
30 |
0.3365 |
| sample |
8.83 |
0.33 |
65 |
| ANB |
control |
4.03 |
3.70 |
30 |
0.8775 |
| sample |
4.16 |
3.78 |
65 |
| Interincisal |
control |
132.15 |
12.06 |
30 |
0.1228 |
| sample |
136.77 |
14.01 |
65 |
| U1 / NP |
control |
107.80 |
9.17 |
30 |
0.4677 |
| sample |
106.46 |
7.90 |
65 |
| L1 / MP |
control |
92.50 |
9.10 |
30 |
0.0613 |
| sample |
88.71 |
9.06 |
65 |
Due to the lack of Normality, variable SNB has been transformed by the square root function (ie, it has been replaced in the analysis by the square root of SNB).
Table 2: Comparison between OSAHS and the Controls.
| |
N-NP |
Gn-NP |
S-NP |
Go-NP |
N-S |
ANS-PNS |
Go-Me |
OB |
| Gn-NP |
0.296* |
|
|
|
|
|
|
|
| S-NP |
0.188 |
0.404** |
|
|
|
|
|
|
| Go-NP |
0.385** |
0.330** |
0.169 |
|
|
|
|
|
| N-S |
0.433** |
0.474** |
0.309* |
0.507** |
|
|
|
|
| ANS-PNS |
0.438** |
0.233 |
0.283* |
0.269* |
0.534** |
|
|
|
| Go-Me |
0.383** |
0.270* |
0.276* |
0.273* |
0.595** |
0.502** |
|
|
| OB |
-0.046 |
-0.193 |
-0.126 |
-0.178 |
-0.040 |
-0.186 |
-0.101 |
|
| OJ |
0.121 |
0.045 |
0.169 |
-0.031 |
0.004 |
0.215 |
-0.043 |
0.360** |
| H-H1 |
0.189** |
0.245* |
0.181 |
0.084 |
0.112 |
0.104 |
-0.153 |
0.129 |
| H-H2 |
0.282 |
0.290** |
0.230* |
0.314* |
0.239* |
0.286** |
-0.060 |
0.091 |
| (H-H1)+(H-H2) |
0.262* |
0.285** |
0.215* |
0.211** |
0.185 |
0.166 |
-0.114 |
0.129 |
** P<0.001, * P<0.05 The linear measurements were higly correlated except that of the overbite and the overjet. The study found that the overjet is highly correlated with overbite.
Table 3: Pearson Correlation Coefficient of the Linear Measurements.
Angular measurement
As shown in Table 4, only the average of SNA was statistically significant higher among OSAHS 82.31 (SD 6.46) when compared with control 76.25 (18.99) with a p-value 0.0231. In addition, there were some positive and negative statistical linear associations.
| |
NP/NSP |
MP/NSP |
NP/MP |
FHP/NSL |
SNA |
SNB |
ANB |
U1/L1 |
U1/NP |
| MP/NSP |
0.350** |
|
|
|
|
|
|
|
|
| NP/MP |
-0.105 |
0.773** |
|
|
|
|
|
|
|
| FHP/NSP |
0.293 |
0.288** |
0.046 |
|
|
|
|
|
|
| SNA |
-0.205 |
-0.169 |
-0.028 |
-0.117 |
|
|
|
|
|
| SNB |
-0.398** |
-0.348** |
-0.132 |
-0.229 |
0.501** |
|
|
|
|
| ANB |
0.198 |
0.335** |
0.270** |
0.105 |
0.115 |
-0.264** |
|
|
|
| U1/L1 |
0.004 |
-0.087 |
-0.021 |
0.019 |
-0.055 |
0.037 |
-0.236 |
|
|
| U1/NP |
0.044 |
-0.244 |
-0.298** |
-0.135 |
0.069 |
0.096 |
-0.081 |
-0.684** |
|
| L1 / MP |
-0.036 |
-0.240** |
-0.269** |
-0.038 |
0.059 |
0.003 |
0.173 |
-0.725** |
0.441** |
Table 4: Pearson Correlation Coefficient of the Angular Measurements.
Discussion
Cephalometric radiography has a long tradition as a diagnostic and follow-up technique in the study of cranio-cervico-facial morphology [24] and in the surgical management of craniofacial deformities [25]. Availability of normative data and the possibility of superimposition of long-term serial records have given this method a unique position [26,27]. Recently, several reports regarding the deviated cephalometric data of OSAHS patients have been published with some controversies [28,29]. Consequently, a comprehensive study of the subject to solve some of these controversies is needed.
The characteristic appearance of the typical patient severely affected by obstructive sleep apnoea hypopnoea syndrome led Osler [30] to characterize this condition as ‘Pickwickian’ according to the novel by Charles Dickens (1836) in which such a condition was described. Subsequently the term ‘Pickwick syndrome’ has sometimes been used for OSAHS. Although no formal description of the head posture in this condition has been made, an extended head posture is generally recognized by clinicians as being a characteristic feature of the appearance of patients with obstructive sleep apnoea [31].
In the field of Orthodontics, the natural head posture is of interest from two aspects: Firstly, in the diagnostic assessment of facial aesthetics in orthodontic and orthognathic surgery treatment plan. Secondly, in the assessment of the role of head posture in postnatal facial morphogenesis
In assessment of facial aesthetics, emphasis is laid on the posture of the head in relation to a gravity-determined true vertical.
Several cephalometric analyses have been developed for the purpose of performing such aesthetic assessments of the maxillary and mandibular protrusion in relation to a gravity determined true vertical [32-34]. It may be noted, however, that widely differing means of the cranio-cervical angulation have been reported by different authors. A survey of means for NSL/ VER in five different studies showed a range from 89.6° to 102.4° [19]. This can be taken to indicate that the cranio-vertical angle is particularly very sensitive to differences in methodology for recording of head posture.
Assessment of facial protrusion in relation to a gravity-determined vertical thus would seem to require further standardization of the positioning procedures used in such studies.
The role of head posture in facial development has been demonstrated in a series of studies which provide for the existence of a sequence of events comprising: obstruction of the upper airways; increase in the cranio-cervical angulation; vertical direction of the facial development.
It is important to notice, however, that the posture involved in this sequence of events is the position of the head in relation to the cervical column. Changes in this angle are mediated by changes in the cranio-vertical and in the cervico-horizontal angles. An increase in cranio-cervical angulation thus can be mediated by an extension of the head in relation to the true vertical, by a forward inclination of the cervical column or by a combination of both.
An increase in the cranio-cervical angle can be triggered by various types of obstruction of the upper airway. One reason for this physiological mechanism could be that such a change in posture will increase the diameter of the airway and thus reduce the airway resistance. Another reason could be that, an increase in the cranio-cervical angle will lift the head away from the hyomandibular complex and thus, facilitate the transition from nasal breathing to mouth breathing which occurs in many subjects with a larger upper airway resistance caused by nasal or nasopharyngeal obstruction [35].
Studies of head posture in subjects with adenoidal obstruction have demonstrated an average increase in cranio-cervical angulation of about 2° [22,36]. This increase is mediated by an increase in the cranio-vertical relationship, whereas the average cervical inclination is not affected. After adenoidectomy this extended head posture in the obstructed children has shown to normalize. Thus, in individual children a reduction of the craniocervical angle of up to 9º has been found [22].
It has long been known that various kind of craniofacial anomalies are closely related to upper airway obstruction which may lead to the OSAHS condition. Craniosynostosis syndrome such as Crouzon or Apert [37], Pierre Robin syndrome [38] and Treacher Collins syndrome [39] were among these.
This present study provides further evidence for the suggestion that obstruction of the upper airway may trigger an increase in the cranio-cervical angulation. Six cranio-cervical angles were statistically different in the OSAHS group when compared to the control with special significance to the angles formed with the OPT. The large difference in cranio-cervical angulation was mediated by a forward inclination of the cervical column. A physiological requirement for a major increase in cranio-cervical angulation due to airway obstruction therefore can only be met by a forward inclination of the cervical column.
A similar mechanism, in head tilting mediates minor changes in head posture whereas larger changes are mediated by changes in cervical inclination, was observed in a study of how subjects produced the change in head posture from the self-balance position to the mirror position [40].
The angle of the cervical curvature (OPT/CVT) has shown to be reduced in the OSAHS group (mean 7°, SD 3.05), when compared to the control (mean 10.9°, SD 4.91). This further shows forward positioning of the head. Similar study found the OPT/CVT to be lesser in the OSAHS group mean 4.5° and SD 2.91 [41]. Similar research found OPT/CVT to be also reduced in the obese OSAHS group (mean 1.1°, SD 2.6), than the control (mean 1.5°, SD 3.1) [42], A comprehensive cephalometric analysis of cranio-cervico-faciohyoid skeletal morphology in 100 male patients with obstructive sleep apnoea (OSA) and 36 male controls was performed, with aberrations in the OSA group features are; shorter dimension of cranial base with slight counter-clockwise rotation and depression of clivus; shorter maxillary length with normal height; maxillomandibular retrognathia related to nasion perpendicular plane (N⊥FH) despite normal angles of prognathism; 47% of the OSA group had mandibular retrognathia; increased anterior lower facial height and mandibular plane angle; reduced size of bony pharynx; inferiorly positioned hyoid bone at C4-C6 level; deviated head posture with larger cranio-cervical angle, and came with the conclusion that cephalometric analysis is highly recommended in OSA patients as one of the most important tools in diagnosis and treatment planning [43].
Conclusion
In linear measurements the OSAHS patients showed increased in upper and lower posterior facial height, decreased length of the maxilla and inferiorly positioned hyoid bone. Angular measurements showed increased SNA angle, which indicate a low angle CL II cases (that explained increased proclination of maxillary teeth and retroclination of the mandibular teeth which has effect on the position of the ‘A’ and ‘B’ points), this shows further forward positioning of the head and clockwise rotation of the craniofacial complex.
We recommend further studies in the use of lateral cephalometric radiograph analysis of the hard (cranio-cervico-facial morphology and hyoid bone position) and soft tissues (pharyngeal width, tongue and soft palate length) using different cephalometric analysis to further aid in the diagnosis and treatment of OSAHS.
7781
References
- Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365: 1046-1053.
- RacioneroCasero MA, García Río F, PinoGarcía JM, Prados Sánchez C, DíazLobato S, et al. (1999) [The sleep apnea syndrome as a health problem. An estimation of its prevalence and morbimortality].An Med Interna 16: 97-102.
- Barthel SW, Strome M (1999) Snoring, obstructive sleep apnea, and surgery. Med Clin North Am 83: 85-96.
- Pieters T, Rodenstein DO (2001) Therapeutic options in obstructive sleep apnoea: have we made enough progress? Sleep Med Rev 5: 3-6.
- Kapur V, Blough DK, Sandblom RE, Hert R, de Maine JB, et al. (1999) The medical cost of undiagnosed sleep apnea. Sleep 22: 749-755.
- Whittle AT, Finch SP, Mortimore IL, MacKay TW, Douglas NJ (1997) Use of home sleep studies for diagnosis of the sleep apnoea/hypopnoea syndrome. Thorax 52: 1068-1073.
- Mageet AO, Khamis AH and McDonald JP. The Relationship between Obstructive Sleep Apnoea hypopnoea Syndrome and the Cranio-Cervical Morphology in Adults: Angular Measurements. International Journal of Scientific Research 4: 672-676.
- Bacon WH, Krieger J, Turlot JC, Stierle JL (1988) Craniofacial characteristics in patients with obstructive sleep apneas syndrome. Cleft Palate J 25: 374-378.
- Battagel JM (1996) Obstructive sleep apnoea: fact not fiction. Br J Orthod 23: 315-324.
- Jamieson A, Guilleminault C, Partinen M, Quera-Salva MA (1986) Obstructive sleep apneic patients have craniomandibular abnormalities. Sleep 9: 469-477.
- Tsuchiya M, Lowe AA, Pae EK, Fleetham JA (1992) Obstructive sleep apnea subtypes by cluster analysis. Am J Orthod Dentofacial Orthop 101: 533-542.
- deBerry-Borowiecki B, Kukwa A, Blanks RH (1988) Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope 98: 226-234.
- Rivlin J, Hoffstein V, Kalbfleisch J, McNicholas W, Zamel N, et al. (1984) Upper airway morphology in patients with idiopathic obstructive sleep apnea. Am Rev Respir Dis 129: 355-360.
- Lowe AA, Santamaria JD, Fleetham JA, Price C (1986) Facial morphology and obstructive sleep apnea. Am J Orthod Dentofacial Orthop 90: 484-491.
- Young JW, McDonald JP (2004) An investigation into the relationship between the severity of obstructive sleep apnoea/hypopnoea syndrome and the vertical position of the hyoid bone. Surgeon 2: 145-151.
- Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics.Book, Elsevier 2013.
- Broca P (1862) Sur les projections de la tete, etsur le nouveau procede de cephalometrique. Bull SocAnthropolparis 3: 514-544.
- Solow B, Tallgren A (1971) Natural head position in standing subjects. ActaOdontolScand 29: 591-607.
- MOLHAVE A (1958) [Sitting & standing posture in man]. UgeskrLaeger 120: 1516-1518.
- Moorees CFA, Kean AR (1958) Natural head position, a basic consideration in the interpretation of cephalometric radiographs. American Journal of Physical Anthropology 16: 213-234.
- Solow B (1996) The pattern of craniofacial association. ActaOdontolScand 24: 21-44.
- Solow B, Greve E (1979) Craniocervical angulation and nasal respiratory resistance. In: Mcnamara J A (ed.) Nasorespiratory function and cranial growth, Monograph No. 9. Craniofacial growth series.Center for Human Growth and Development, University of Michigan. Ann Arbor 26-54.
- Lyberg T, Krogstad O, Djuspesland G (1989) Cephalometric analysis in patients with obstructive sleep apnoea syndrome: I. Skeletal morphology. Journal of Laryngology and Otology 103: 287-292.
- Broadbent BH (1931) A new X-ray technique and its application to orthodontia, Angle Orthodontist 1: 45-66.
- Burstone CJ, James RB, Legan H, Murphy GA, Norton LA (1978) Cephalometrics for orthognathic surgery. J Oral Surg 36: 269-277.
- Behrents R (1985) Growth in the Aging Craniofacial Skeleton. Craniofacial Growth Series, Ann Arbor, Michigan.
- Behrents, R (1985) An Atlas of Growth in the Aging Craniofacial Skeleton. Craniofacial Growth Series, Ann Arbor, Michigan.
- Maltais F, Carrier G, Cormier Y, Sériès F (1991) Cephalometric measurements in snorers, non-snorers, and patients with sleep apnoea. Thorax 46: 419-423.
- Davies RJ, Stradling JR (1990) The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. EurRespir J 3: 509-514.
- Osler W (1901) The principle practice of medicine, 4th edn. Pentland, Edinburgh.
- Cote EF (1988) Obstructive sleep apnea--an orthodontic concern. Angle Orthod 58: 293-307.
- Moorrees CF, uanVenrooij ME, Lebret LM, Glatky CG, Kent RL, et al. (1976) New norms for the mesh diagram analysis. Am J Orthod 69: 57-71.
- Cooke MS, Wei SH (1988) The reproducibility of natural head posture: a methodological study. Am J Orthod Dentofacial Orthop 93: 280-288.
- Lundström F, Lundström A (1989) Clinical evaluation of maxillary and mandibular prognathism. Eur J Orthod 11: 408-413.
- Ricketts RM (1968) Respiratory obstruction syndrome, from the forum on the tonsil and adenoid problem in orthodontics. Am J Orthod 54: 485-514.
- Woodside DG, Linder-Aronson S (1979) The channelization of upper and lower anterior face heights compared to population standard in males between ages 6 to 20 years. Eur J Orthod 1: 25-40.
- Schafer ME (1982) Upper airway obstruction and sleep disorders in children with craniofacial anomalies. ClinPlastSurg 9: 555-567.
- Lapidot A, Ben-Hur N (1975) fastening the base of the tongue forward to the hyoid for relief of respiratory distress in the Pierre Robin syndrome. Plastic and Reconstructive Surgery 56: 89-91.
- Johnston C, Taussig LM, Koopmann C, Smith P, Bjelland J (1981) Obstructive sleep apnea in Treacher-Collins syndrome. Cleft Palate J 18: 39-44.
- Solow B, Tallgren A (1971) Postural changes in craniocervical relationships. Tandlaegebladet 75: 1247-1257.
- Solow B, Ovesen J, Nielsen PW, Wildschiødtz G, Tallgren A (1993) Head posture in obstructive sleep apnoea. Eur J Orthod 15: 107-114.
- Sakakibara H, Tong M, Matsushita K, Hirata M, Konishi Y, et al. (1999) Cephalometric abnormalities in non-obese and obese patients with obstructive sleep apnoea. EurRespir J 13: 403-410.
- Tangugsorn V, Skatvedt O, Krogstad O, Lyberg T (1995) Obstructive sleep apnoea: a cephalometric study. Part I. Cervico-craniofacial skeletal morphology. Eur J Orthod 17: 45-56.