Keywords
allergy, allergic reaction, antiseptics, disinfectants, preventive measures.
Introduction
The exposure of the nursing staff to variable allergens in the workplace constitutes an important occupational risk. The substances commonly listed as the most important allergens affecting mainly nurses, are natural latex glove proteins, several antiseptics, instruments and surface disinfectants (especially glutalraldehyde), drugs (like penicillins, cephalosporins, antineoplastic agents), as well as fragrances contained most often in liquid soaps and hand disinfectants [1,2].
Occupational asthma of different severity, or a variety of skin disorders are the most common manifestations of an allergic reaction in the workplace [3,4].
Health care workers accounted for 16% of 1879 work-related asthma cases, as reported between 1993 and 1999 to the National Institute for Occupational Safety and Health (NIOSH). Data showed that among these health care workers the majority worked in hospitals and nurses consisted the largest proportion (more than 40%) of all cases [4]. Health care workers may develop allergic asthma from breathing in powdered proteins of latex gloves or from mixing powdered medications [3]. Allergic skin reactions are presented in two forms: either as allergic contact dermatitis (delayed cutaneous hypersensitivity reaction type IV), in which a rash, edema, eczema or papules appear some hours after contact with the allergen or as urticaria (type I hypersensitivity reaction or anaphylactic reaction - IgE), usually within minutes of exposure to the allergen. Type I hypersensitivity reactions are potentially more dangerous given that their clinical presentation except of localized or generalized urticaria may also include, edema of the larynx, bronchospasm or anaphylactic shock [5].
The aim of this multicenter, descriptive study was to evaluate the frequency and the type of allergic reactions in the nursing staff at work.
Subjects and Method
An anonymous questionnaire regarding a history of an occupational allergic reaction in the past was distributed to the nursing staff of three general hospitals of Athens (Konstantopoulion, Evaggelismos and Gennimatas: 180, 500 and 120 questionnaires respectively). The statistical package SPSS for Windows version (10.0.1) was used for the statistical analysis
Results
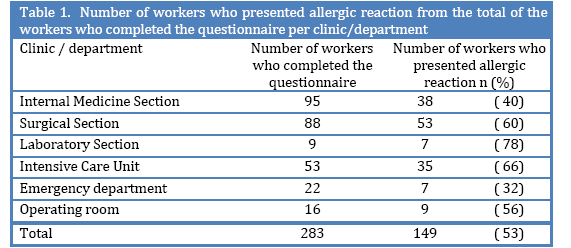
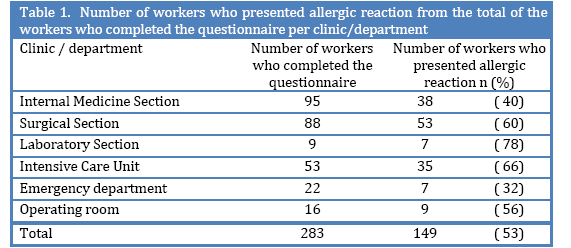
From the total of 800 questionnaires distributed , 283 were returned completed to the investigators: 105 (58%) from Konstantopoulion, 115 (23%) from Euaggelismos and 63 (52%) from Gennimatas . The overall response rate of was 35%. The workers who completed the questionnaire were 28 males (9,9%), 255 females (90,1%) with a mean age of 38±16 years , The majority of the nursing stuff was working in the internal or surgical clinics and in the intensive care units . (Table 1). A history of an allergic reaction in the workplace was reported in 149 individuals (53%), and 62 of them (41,6%) presented the most recent episode in the previous year. In 75% of the subjects 2 or more episodes were reported. Rash (74.5%) ,dyspnea (29.5%), facial angioedema (16.1%) ,laryngeal edema (6,7%), were the manifestations reported .No episode of allergic shock was quoted.
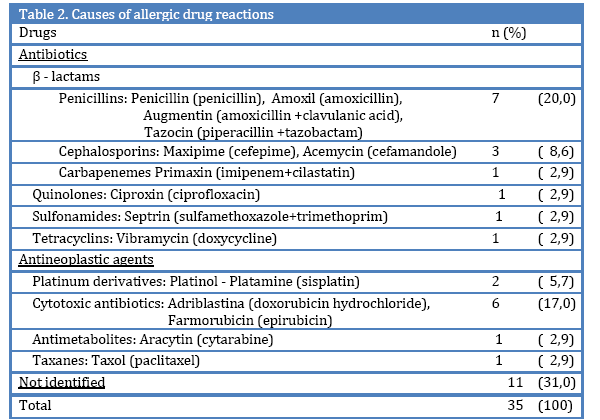
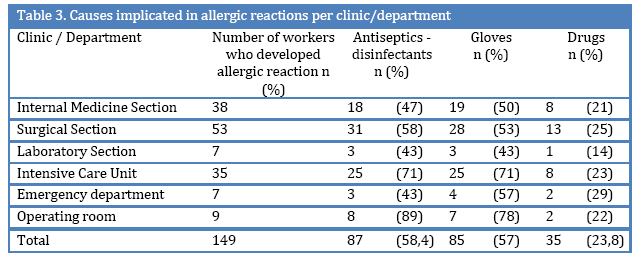
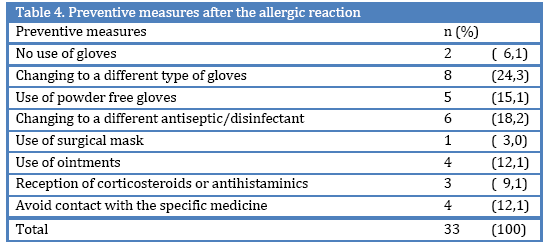
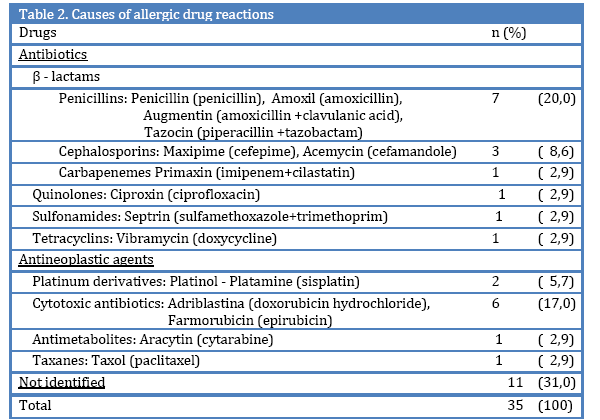
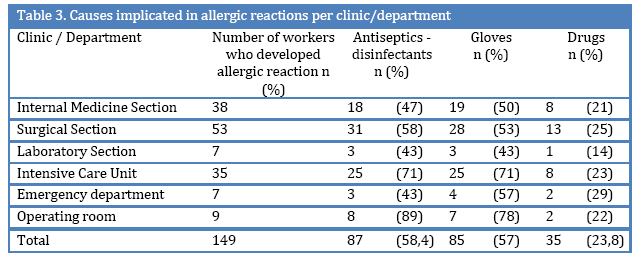
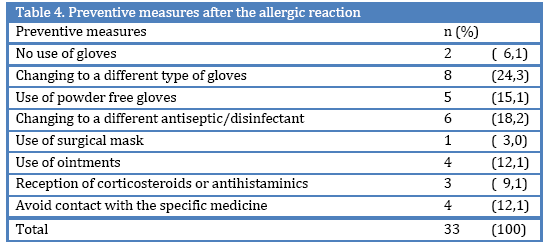
In 58,4% of the cases of allergic reactions antiseptics-disinfectants (like povidone iodine, chlorhexidine, sodium hypochloride, glutaraldehyde) have been implicated, in 57% gloves, in 23,5% some medication (table 2) while in 22,8% of the cases the causative agent could not be identified (table 3). From the total of the workers who presented with an allergic reaction, 77 (51,7%) needed medical treatment, 12 (8,1%) hospitalization, 17 (11,4%) received sick- leave, while only 9 individuals (6%) changed clinic/department of work.In 42 % of the allergic cases the head nurse was not informed. Only 33 individuals (22,1%) took preventive measures after the allergic episode (table 4), while 41,6% of the workers reported that taking preventive measures is practically difficult.
Finally, 45% of the individuals with a history of occupational allergic reactions had also a history of allergic reactions outside the workplace. There was no statistical significant relation found between the development of allergic reaction in the workplace and the history of allergic reactions outside the workplace (logistic regression coefficient β=0,154 with 95% confidence intervals:0,50-2,71 and p=0,72).
Discussion
The response rate of the nursing staff regarding the completion of the questionnaire is considered small (35%), taking into account the extent and the dangerousness of the problem.
The percentage of the nursing staff who reported a history of allergic reaction in the workplace was significant (53%). This percent would possibly be even higher if there was a greater correspondence from nurses who work in areas where there is a high use of latex gloves and/or antiseptics-disinfectants like operating rooms, intensive care units and emergency departments.
The current study was retrospective and the estimation of the type and frequency of allergic reactions was made based upon data self-reported by he workers who completed the questionnaire, without objective confirmation (confirmation of the involvement of the immune system with clinical and laboratory diagnostic tests), fact which may have led to imprecise estimation of the frequency of allergic reactions (systematic error). This problem is also met in relative studies that are reported in the international literature [6,7].
In the majority of the allergic reactions the antiseptics-disinfectants and gloves have been implicated. This finding agrees with the findings of relative studies [8,9].
The prevalence of latex allergies has significantly increased over the past two decades primarily due to the increased use of gloves for barrier protection after the “universal precaution” recommendations, and is estimated to be between 10% and 17% [7,10,11].
Latex allergy can present as variable clinical reactions like allergic contact dermatitis (triggered by the chemical additives used during the treatment of natural rubber), allergic contact urticaria, rhinoconjuctivitis, asthma, anaphylaxis and seldom anaphylactic shock, caused by the proteins contained in the natural rubber. Exposure to latex proteins can occur through contact with the skin or the mucous membranes or inhalation of the particles of glove powder which absorb the proteins and become airborne and widely disseminated in the work place as the gloves are donned and removed by the staff [7,12-14].
Nurses can minimize their risk of sensitization by using latex gloves only when necessary (contact with infectious substances). When the use of gloves is imposed it is better to use powder-free gloves. In the rest of the cases nonlatex gloves can be used. Gloves made of protein-free synthetic materials and particularly vinyl gloves have been proved to have poor barrier performance, and although they may be protein-free, they are not allergen-free [7].
Frequent cleaning of the surfaces as well as good ventilation of the working areas in order to remove the particles of dust containing latex proteins is very important. In case of allergic reaction complete avoidance of exposure to latex, although very difficult, is the most effective approach [4,7,15]. Given that latex proteins become airborne complete avoidance of exposure to them by the allergic individual is not possible (even if the same individual doesn’t use gloves) when gloves are used from the other personnel in the same area.
A much smaller percentage (23,5%) of allergic reactions was attributed to medications, mainly β- lactams (penicillins, cephalosporins, carbapenemes) and antineoplastic agents. This finding agrees with the findings of relative studies [1].
A significant percentage of the workers who presented allergic reaction needed medical treatment, while few were hospitalized and even fewer had to change clinical/department of work. In the literature cases of nurses who even had to leave their job because of the severe health problems caused by allergic reactions in the workplace, are reported [16].
Health care workers with a history of atopy (type I allergic reaction), are at an even grater risk for sensitization and allergic reactions following exposure to several occupational allergens [7,17,13,19]. In our study 45% of the workers with a history of allergic reactions in the workplace had also a history of allergic reactions outside the workplace, without, finding a statistically significant difference in our sample.
Future prospective studies are certainly useful in order to determine the type of allergens to which nurses are daily exposed in the course of their work and to measure the levels of exposure. More research is required into prevalence of allergic reactions at work and prevention strategies. It is also important to educate health care workers in order to make them aware of their risk and ways to protect themselves.
3679
References
- Schnuch A, Uter W, Geier J, Frosh PJ, Rustemeyer T. Contact allergies in healthcare workers. Results from the IVDK. Acta Derm Venereol 1998;78:358-363.
- Buckley DA, Rycroft RJG, White IR, McFadden JP. Fragrance as an occupational allergen. Occup Med 2002;52:13-16.
- Bernstein DI. Allergic reactions to workplace allergens. JAMA 1997;278(22):1907-1913
- Filios MS, Pechter E. Health care workers and asthma. Am J Nurs 2006;106(4):96.
- Garabrant DH, Schweitzer S. Epidemiology of latex sensitization and allergies n health care workers. J Allergy Clin Immunol 2002;110(2):S82-95.
- McFadden ER. Natural rubber latex sensitivity seminar: conference summary. J Allergy Clin Immunol 2002;110(2):S137-140.
- McDonald JC, Keynes HL, Meredith SK. Reported incidence of occupational asthma in the United Kingdom. Occup Environ Med 2000;57:823-829
- Vyas A, Pivkering CA, Oldham LA, Francis HC, Fletcher AM, Merrett T, et al. Occup Environ Med 2000;57:752-759
- Roy Dr. Latex glove allergy – dilemma for health care workers. An overview. AAOHN J. 2000;48(6):267-277
- Zaglaniczny K. Latex allergy: are you at risk? AANA J 2001;69(5):413-424.
- Sussman GL, Beezhold DH. Allergy to latex rubber. Ann Intern Med 1995;122:43-46
- Fish JE. Occupational asthma and rhinoconjunctivitis induced by natural rubber latex exposure. J Allergy Clin Immunol 2002;110(2):S 75-81
- DHHS (NIOSH) Preventing allergic reactions to natural rubber latex in he workplace. 1997 Publication No. 97-135
- Booth B. Latex allergy: a growing problem in healthcare. Prof Nurse 1996;11(5):316-319.
- Bauer X, Ammon J, Chen Z, Beckman U, Czuppon AB. Health risk in hospitals through airborne allergens for patients presensitized to latex. Lancet 1993;342:1148-1149
- Hunt LW, Fransway AF, Reed CE Miller LK, Jones RT, Swanson MC, et al. An epidemic of occupational allergy to latex involving health care workers. J Occup Environ Med 1995;37:1204-1209
- Amr S, Bollinger ME. Latex allergy and occupational asthma in health care workers: Adverse outcomes. Environmental Health Perspectives 2004;112:378-381
- Petsonk EL. Work-related asthma and implications for the general public. Environ Health Perpect 2002;110:S569-72