John Ouma1*, Dereje Mamo1 and Marcus Gritzman2
1 Department of Neurosurgery, University of the Witwatersrand, Johannesburg, South Africa
2 Gritzman & Thatcher, Anatomical Pathologists, Johannesburg, South Africa
- *Corresponding Author:
- Ouma JR
Department of Neurosurgery
University of the Witwatersrand
Johannesburg, South Africa.
Tel: 0117172239
E-mail: John.Ouma@wits.ac.za
Received Date: March 20, 2018; Accepted Date: May 10, 2018; Published Date: May 15, 2018
Citation: Ouma J, Mamo D, Gritzman M (2018) Occurrence of cerebellar haemangioblastoma in a 13-year-old girl with Neurofibromatosis type 2; Report of a case and discussion of the literature. Arch Cancer Res. Vol.6 No.2:7 DOI: 10.21767/2254-6081.100173
Neurofibromatosis is a condition that can occur in a number of forms, the commonest of which are types 1 and 2. As a group, they fall under the phacomatoses family of conditions, otherwise known as neurocutaneous syndromes, owing to the fact that they concurrently have disorders of the nervous system and the integument, which organs share a common ectodermal origin. Other examples include Schwannomatosis and Von Hippel Lindau syndromes. We describe a case of a young girl who presented with features of NF2 and was discovered to have a cerebellar hemangioblastoma at the same time. We are not aware of this association being described in the literature.
Keywords
Neurofibromatosis; Cerebellar hemangioblastoma; Phacomatoses; Neurocutanoeus Syndromes
Introduction
Neurofibromatosis type 2 is a disorder characterized by the growth of noncancerous tumors in the nervous system. The most common tumors associated with neurofibromatosis type 2 are called vestibular schwannomas or acoustic neuromas. These growths develop along the nerve that carries information from the inner ear to the brain (the auditory nerve). Tumors that occur on other nerves are also commonly found with this condition. We describe a case of a young girl who presented with features of NF2 and was discovered to have a cerebellar haemangioblastoma at the same time. We are not aware of this association being described in the literature.
Clinical Presentation
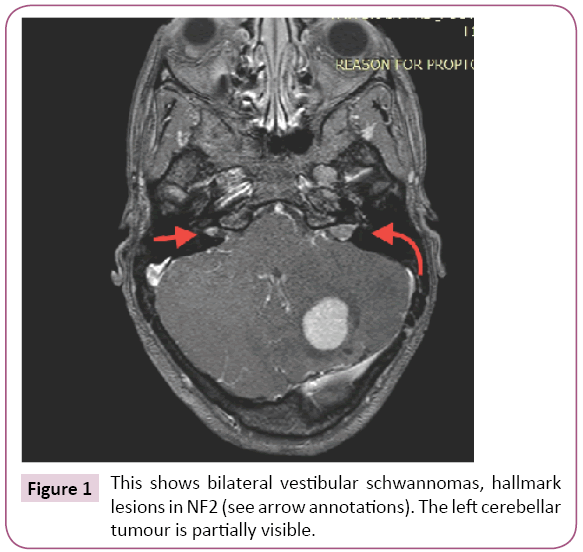
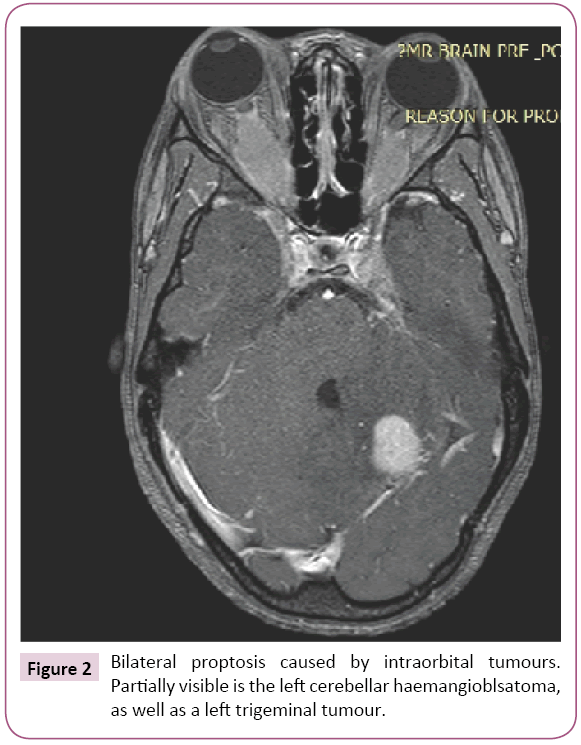
This young girl was referred to her family physician for bilateral painless proptosis that had developed spontaneously over a period of several months. She was subsequently referred to the neurosurgical service following a brain scan. By the time she was seen by us, she had developed a raised pressure type of headache as her main symptom. Clinically, she was in good condition, had no cutaneous lesions, and other than the obvious bilateral proptosis, had no other noteworthy findings on the general or neurological examinations. Her brain magnetic resonance imaging (MRI) scan showed a total of nine separate enhancing lesions in the brain, orbits, and on both sides of the tentorium cerebelli (Figure 1). In particular, she had bilateral acoustic schwannomata, fulfilling the criteria for the diagnosis of Neurofibromatosis 2 by both the Manchester and Baser criteria. Owing to the size of the cerebellar lesion and the symptoms that is was causing, we decided to remove it. It turned out to be a spongy, extremely vascular lesion with a vascular stalk from the inferior surface of the tentorium. It was successfully excised in toto, and histological examination showed it to be a hemangioblastoma (Figure 2). This was entirely in keeping with its vascular nature and gross appearance. The rest of the lesions appeared to be schwannomas rather than hemangioblastomas radiologically, but no attempt was made to biopsy them. Further clinical and radiological examination excluded any features in keeping with Von Hippel Lindau disease. Genetic testing for the phacomatoses was not available in our institution at the time. Of note, there was no positive history suggestive of any neurocutaneous syndrome amongst her firstdegree relatives.
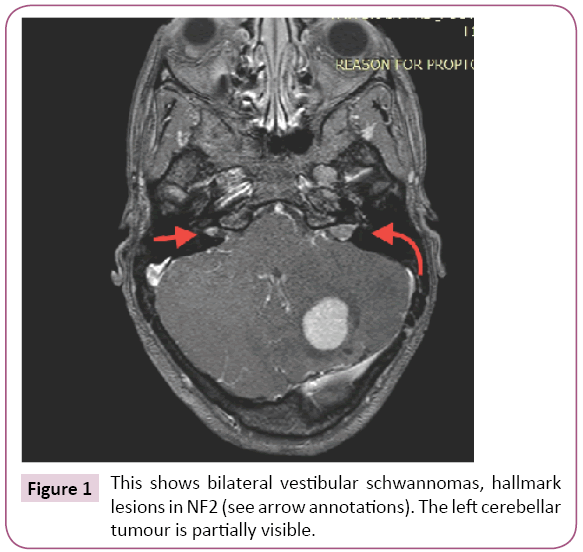
Figure 1: This shows bilateral vestibular schwannomas, hallmark lesions in NF2 (see arrow annotations). The left cerebellar tumour is partially visible.
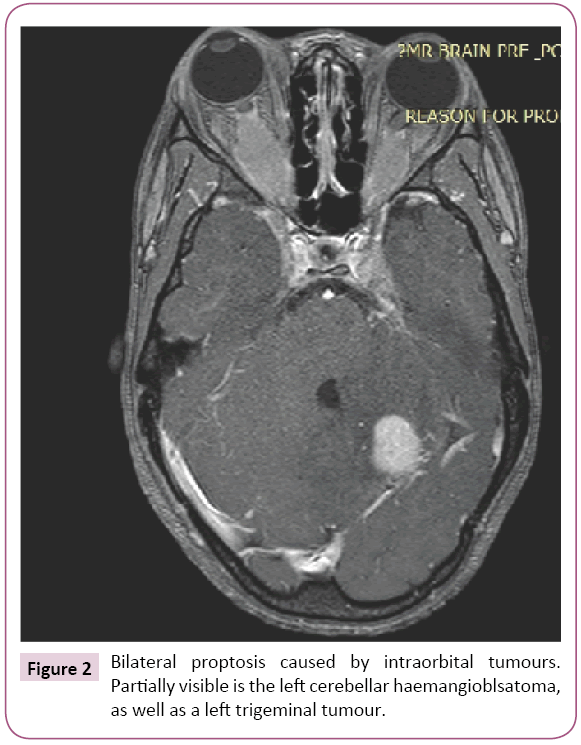
Figure 2: Bilateral proptosis caused by intraorbital tumours. Partially visible is the left cerebellar haemangioblsatoma, as well as a left trigeminal tumour.
Discussion
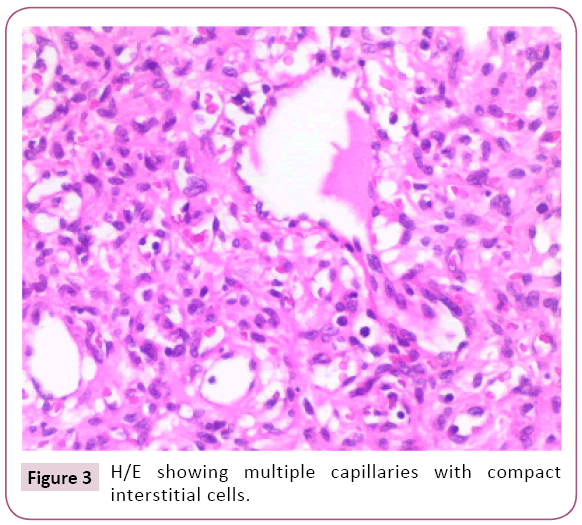
The diagnosis of neurofibromatosis type 2 is made upon fulfilling certain criteria, as expressed in the Manchester or the newer baser criteria. These include the presence of bilateral vestibular schwannomas (VS), as was the case in this patient [1-4]. Her initial manifestation was with bilateral proptosis, possibly due to intraorbital involvement of the III cranial nerves with schwannomata as they are prone to do [2], or else due to meningiomas. NF2 is associated with multiple tumours, primarily intracranial schwannomas and meningiomas, as well as spinal ependymomas [2,4]. For this reason, it is also referred to as the MISME (multiple inherited Schwanommas, meningiomas and ependymomas) syndrome (Figure 3). Hemangioblastomas may occur sporadically or as part of the Von Hippel Lindau syndrome, in which case they are associated with multiple other tumours and disorders of a wide range of organs. Von Hippel Lindau syndrome is associated with cerebellar and spinal hemangioblastomas, retinal-naevi, pancreatic and renal cysts as well as pancreatic cancer. We are not aware of any reports in the literature of the occurrence of hemangioblastomas in the setting of a case of NF2. The genetic basis for these conditions has been well described [1-4]. This patient presents with a hemangioblastoma in addition to the classic picture of NF2 with bilateral vestibular schwannomas and multiple other tumours around the brain.
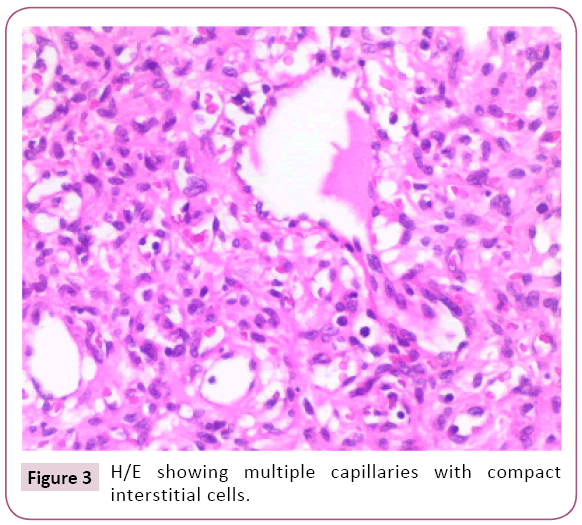
Figure 3: H/E showing multiple capillaries with compact interstitial cells.
Conclusion
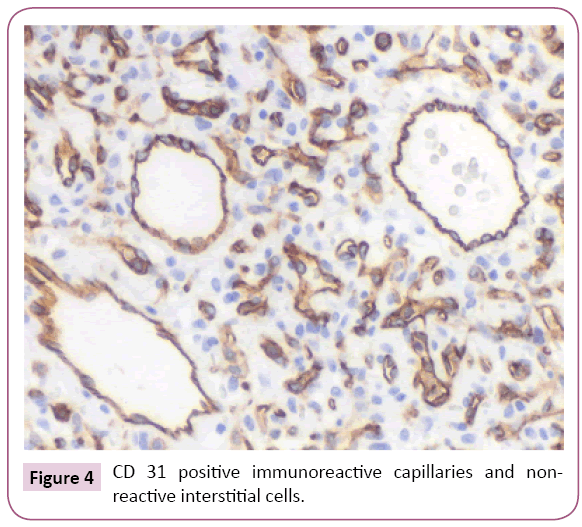
This paper is written to draw attention to this association, which may have direct implications as the vascularity and surgical difficulties presented by the hemangioblastoma in this patient may surprise an unsuspecting surgeon. We suggest that the occurrence of this previously undescribed association may be due to sheer chance, although there may be an unrecognized association that may become apparent as more reports like this one come to light. One hopes that this paper will encourage surgeons with similar experiences to report their cases. The prognosis of this case is, we think, rather guarded. She faces the possibility of multiple further procedures to preserve her vision and hearing as well, in addition to controlling intracranial pressure. The role of radiation in a case of this sort will need to be defined (Figure 4).
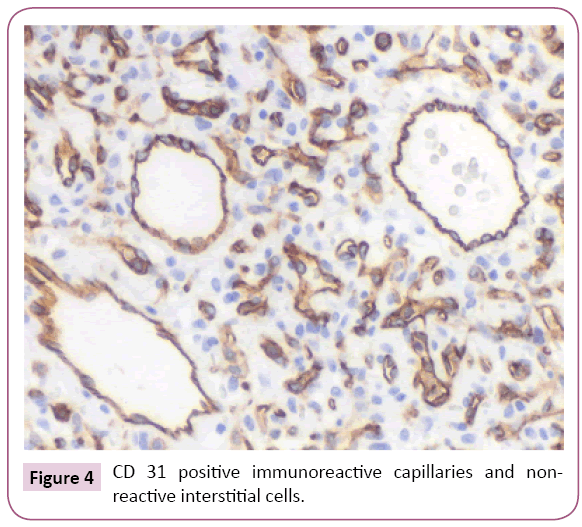
Figure 4: CD 31 positive immunoreactive capillaries and nonreactive interstitial cells.
22633
References
- Rodrigues LO, Batista PB, Goloni-BertolloEM, De Souza-Costa D, Eliam L, et al. (2014) Neurofibromatoses: Part 1 - Diagnosis and differential diagnosis. ArqNeuropsiquiatr 72: 241-250.
- Borofsky S, Levy LM (2013) Neurofibromatosis: Types 1 and 2. AJNR Am J Neuroradiol 34: 2250-2251.
- Goutagny S, Bah AB, Henin D, Parfait B, Grayeli AB, et al. (2012) Long-term follow-up of 287 meningiomas in neurofibromatosis type 2 patients: Clinical, radiological, and molecular features. Neuro Oncol 14: 1090-1096.
- Fisher MJ, Belzberg AJ, De Blank P, De Raedt T, Elefteriou F, et al. (2018) Children's Tumor Foundation Conference on Neurofibromatosis type 1, Neurofibromatosis type 2, and Schwannomatosis. Am J Med Genet A 176:1258-1269.