Ichsan AM1,2*, Stevanie N1, Habibah SM1,2 and Budu P1,2
1Faculty of Medicine, Department of Ophthalmology, Hasanuddin University, Makassar, Indonesia
2Celebes Eye Center ORBITA, Makassar, Indonesia
*Corresponding Author:
Ichsan AM
Faculty of Medicine, Department of
Ophthalmology, Hasanuddin University
Makassar, Indonesia
Tel:+6281342280880
E-mail: am_ichsan@yahoo.com
Received date: June 11, 2018; Accepted date: July 07, 2018; Published date: July 12, 2018
Citation: Ichsan AM, Stevanie N, Habibah SM, Budu P(2018) Oral Furosemide Therapy in Patients with Exudative Retinal Detachment Due to Hypertensive Retinopathy-IV. Ann Clin Lab Res. Vol.6 No.3:240. doi:10.21767/2386-5180.100240
Keywords
Hypertension retinopathy; Exudative retinal detachment; Furosemide
Introduction
Hypertension is a significant risk factor for heart disease, kidney disease, ischemic and hemorrhagic stroke, that may cause sudden death. In the field of eye diseases, severe hypertension accompanied by the presence of retinal hemorrhages, exudates and papil edema may cause blindness and very poor prognosis if it delayed for treatment [1].
Preeclampsia is characterized by new onset hypertension and proteinuria in pregnancy. Placental ischemia lead to activation of the maternal vascular endothelium elevates vascular sensitivity to angiotensin II, and decrease formation of vasodilators such as nitric oxide. These endothelial abnormalities cause generalized vasoconstriction throughout the body including kidney [2]. Patients with chronic kidney disease, impaired renal sodium handling leads hypertension because of extracellular fluid volume increases despite a decreased of total peripheral resistance [3].
The typical sign of hypertensive retinopathy is retinal vascular changes in hypertensive person. Initially there is vasoconstrictive stage. This stage is seen as a generalized narrowing of the retinal arterioles, intimal thickening, hyperplasia of the media wall, and hyaline degeneration in the subsequent, sclerotic. The next stage is an exudative stage. It is signed by disruption of the blood retinal barrier, necrosis of the smooth muscles and endothelial cells, exudation of blood and lipids, and retinal ischemia. These changes are seen as microaneurysms, hemorrhages, hard exudates and cotton-wool spots. Swelling of the optic disk usually indicates severe hypertension [4].
Furosemide inhibits chloride transport systems in a wide variety of epithelia. Furosemide-inhibitable chloride (Cl) absorption may be a driving force for fluid absorption across the retinal pigment epithelium (RPE). This is consistent with a model for ion transport in the isolated RPE, in which active furosemideinhibitable transport of chloride from retina to choroid accounts for a significant fraction of the short-circuit current [5]. The RPE pump absorbs and drains fluid from the retinal to the choroidal surface [6]. The flow of subretinal fluids may assist the sensory retina in attachment to the RPE, and unconventional routes for aqueous humor drainage in eyes with retinal detachments [6].
In this article, we report cases of 2 young patients with exudative retinal detachment due to hypertensive retinopathy grade- IV who led to the diagnosis and management of hypertensive retinopathy with oral furosemide.
Case Presentation
Case 1
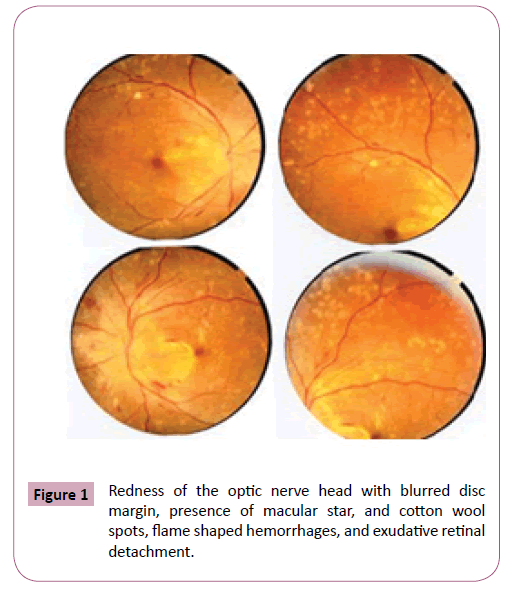
A 21-year-old male patient complained a sudden blurred of vision in both eyes. Patient has a history of hypertension and kidney failure since two months ago and routine dialysis for twice a week. Initial ophthalmology assessment revealed visual acuity on the right eye was 20/100 and the left eye was 20/200. Anterior segment examination showed subconjunctival bleeding in the right eye. Posterior segment examination revealed hard exudates, macular star and inferior retinal detachment in both eyes with remarkably visible a shifting fluid. Patient received citicholine 1000 mg, furosemide, amlodipine 10 mg, bisoprolol, and valsartan once daily, domperidon 3 times daily, methylprednisolon eye drops combined with sodium diclofenac eye drops 5 times daily in both eyes (Figure 1).
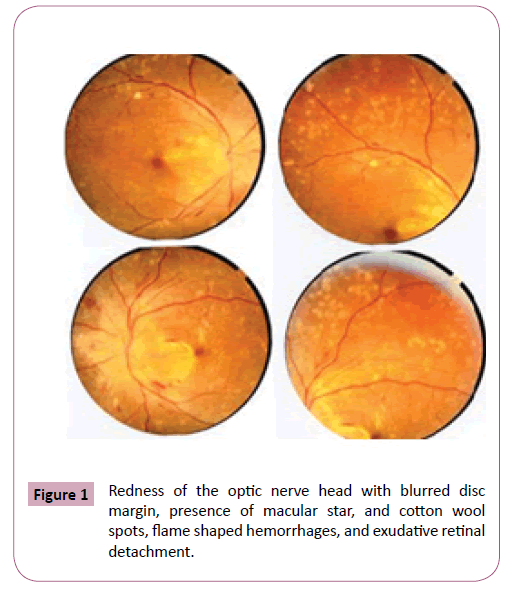
Figure 1: Redness of the optic nerve head with blurred disc margin, presence of macular star, and cotton wool spots, flame shaped hemorrhages, and exudative retinal detachment.
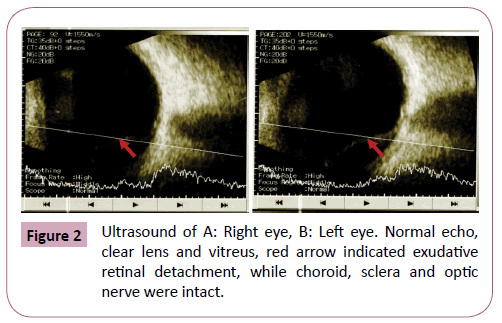
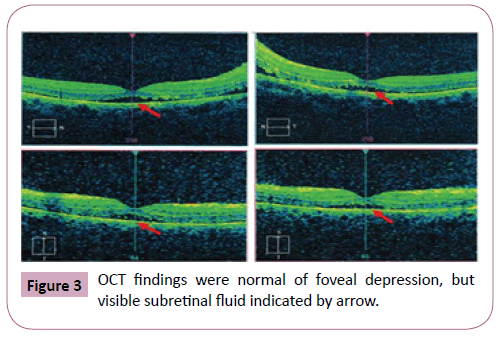
Seventeen days after oral therapy with furosemide, visual acuity increased to 20/80 in both eyes. Anterior segment showed diminished of sub-conjunctival bleeding in the right eye. Posterior segment examination revealed cotton wool spots and shallow detachment at the inferior retina in both eyes (Figures 2 and 3).
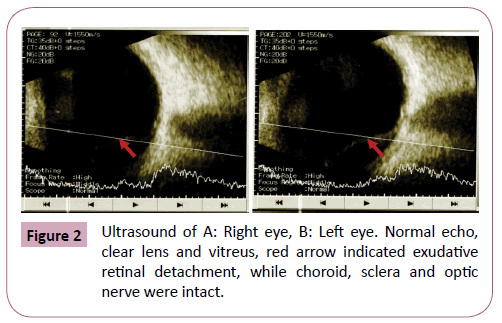
Figure 2: Ultrasound of A: Right eye, B: Left eye. Normal echo, clear lens and vitreus, red arrow indicated exudative retinal detachment, while choroid, sclera and optic nerve were intact.
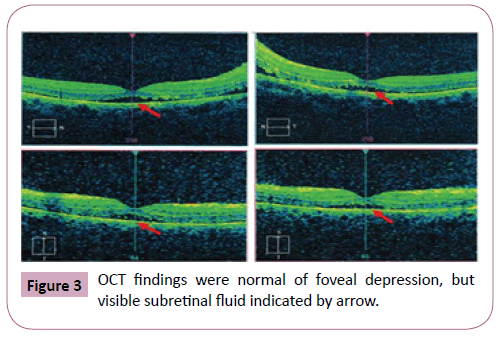
Figure 3: OCT findings were normal of foveal depression, but visible subretinal fluid indicated by arrow.
Case 2
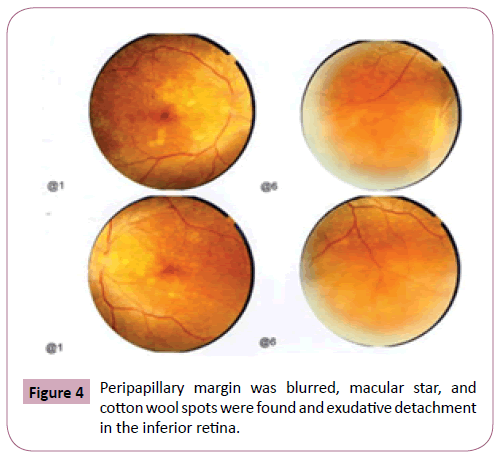
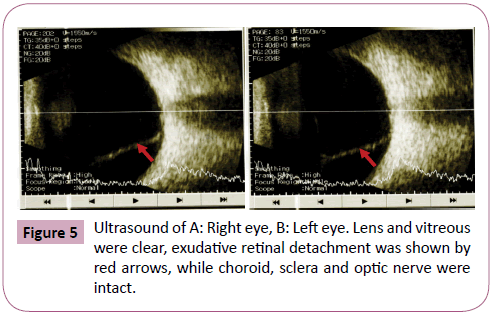
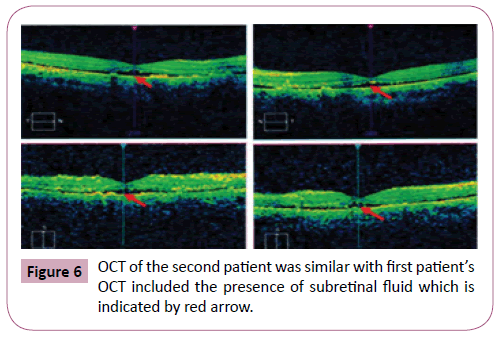
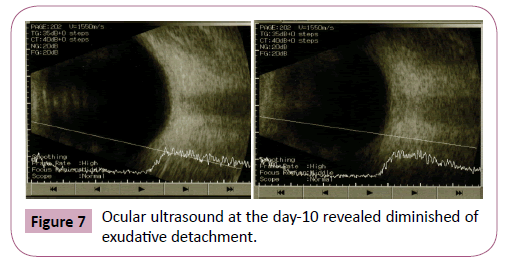
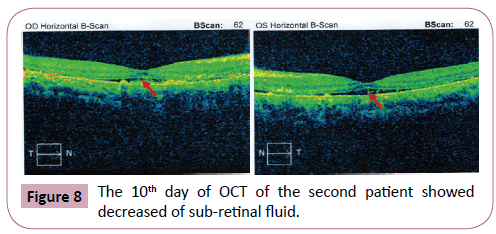
A 26-year-old woman complained a sudden blurred of vision in both eyes, one day after delivered her second child. Antenatal care recorded hypertension history including anti-hypertensive agent therapy. After delivered, her blood pressure increased to 180/100 mmHg and patient was immediately transferred to district hospital. Ophthalmology examination showed visual acuity in both eyes was 2/60. Anterior segment was within normal limit, while some abnormalities in posterior segment were found such as hyperemia of the optic nerve head (ONH), cotton-wool spots, and inferior retinal detachment that changed according to changing position. Patient received oral citicholine 1000 mg, and furosemide 40 mg, amlodipine 10 mg, and Isosorbide dinitrate 5 mg once daily, hepatoprotector twice daily, methylprodnisolone eye drops and sodium diclofenac eye drops 3 times daily in both eyes (Figures 4-6). Ten days after treated by oral furosemide, visual acuity improved to 20/400 in both eyes. Anterior segment remain normal and decreased of exudate sub-retinal in inferior quadrant (Figures 7 and 8).
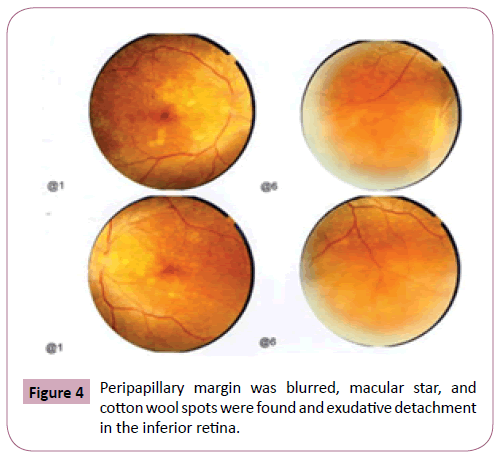
Figure 4: Peripapillary margin was blurred, macular star, and cotton wool spots were found and exudative detachment in the inferior retina.
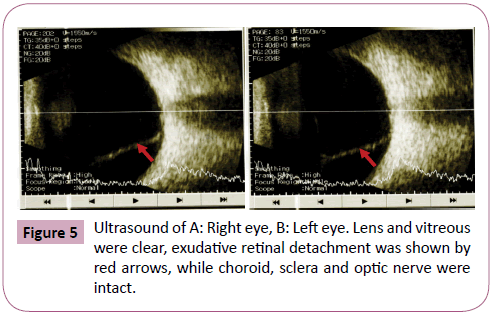
Figure 5: Ultrasound of A: Right eye, B: Left eye. Lens and vitreous were clear, exudative retinal detachment was shown by red arrows, while choroid, sclera and optic nerve were intact.
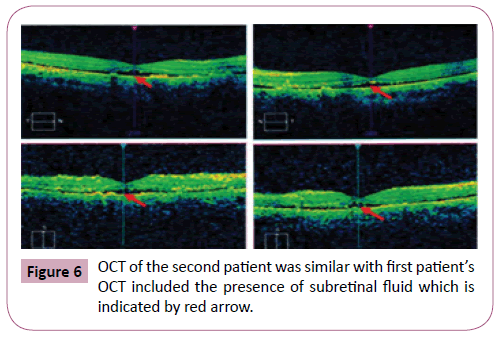
Figure 6: OCT of the second patient was similar with first patients OCT included the presence of subretinal fluid which is indicated by red arrow.
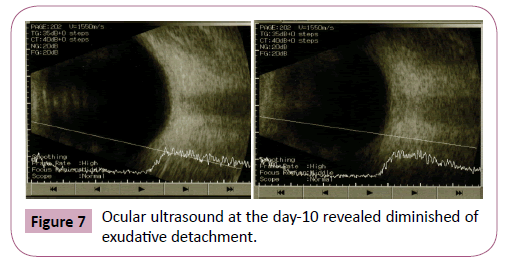
Figure 7: Ocular ultrasound at the day-10 revealed diminished of exudative detachment.
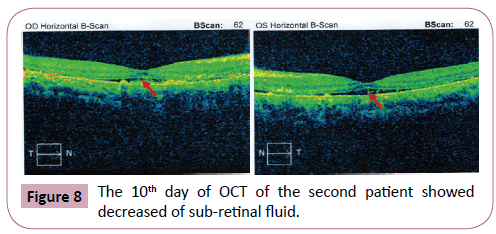
Figure 8: The 10th day of OCT of the second patient showed decreased of sub-retinal fluid.
Discussion
High level of blood pressure affects precapillary arterioles and capillaries, the anatomical loci of autoregulation and nonperfusion [7] which is may cause blood–retina barrier breakdown or obliteration of capillaries [8]. This condition resulted intraretinal hemorrhages, cotton-wool spots, retinal edema, or swelling of the optic disc [8]. The effects of arterial hypertension can be directly visualized in the fundus [9]. These changes may involve the retinal arterioles, the choroid, and the optic nerve [9]. Hypertensive retinopathy graded into a vasoconstrictive phase, an exudative phase, a sclerotic phase, and complications of the sclerotic phase. In the vasoconstrictive phase, the rise of systemic blood pressure excites pliable and nonsclerotic retinal vessels to increase their vascular tone by autoregulation [10]. In the exudative phase, blood is extravasated to form flame-shaped and splinter hemorrhages. Retinal capillary closure with areas of nonperfusion may be observed by fluorescein angiography. Cotton-wool spots are seen scattered in the posterior pole. Breakdown of the blood-retinal barrier can be quantitated by vitreous fluorophotometry [10]. Metabolic transport activity of the RPE is the mechanism for dehydrating the subretinal space. It may be related to retinal adhesiveness [11,12]. Furosemideinhibitable chloride (Cl) absorption may be a driving force for fluid absorption through the RPE [5,13,14]. Furosemide is effective at the apical side of the RPE that might cause delayed reabsorption of subretinal fluid following retinal detachment surgery [14]. It reduced the apical-to-basal Cl-flux and supressed the net Cl-flux. The transepithelial electrical current was reduced. Furosemide had no effect when Cl was removed from the bathing medium. It shows that furosemide acts on a transport site needs extracellular Cl [15]. It was reported the usage of furosemide in patients with diabetic who had significant macular edema and visual loss, the condition evolved favorably under treatment with gradual remission of macular edema and recovery of visual function after oral therapy with furosemide 40 mg daily for 3 weeks [16]. Patients with diabetic macular edema should be treated with oral furosemide 40 mg twice daily for 2 weeks to reduce the amount of fluid overload and resolving the macular edema [17].
Conclusion
In summary, furosemide treatment is effective for patients with hypertensive retinopathy grade-IV with exudative retinal detachment, based on literature review and our cases. In cases of hypertension crisis, blood pressure should be aggressively controlled and gradually normalized the systemic condition and to achieve an improvement of visual acuity.
23017
References
- Gabb GM, Mangoni AA, Anderson C, Arnolda L, Cowley D, et al. (2016) Guidelines for the diagnosis and management of hypertension in adults. National Heart Foundation of Australia. 1-84.
- Palei AC, Spradley FT, Warrington JP, George EM, Granger JP, et al. (2013) Pathophysiology of hypertension in preeclampsia: A lesson in integrative physiology. Acta Physiol (Oxf) 208(3): 224-233.
- Abraham G, Arun KN, Gopalakrishnan N, Renuka S, Pahari DK, et al. (2017) Management of hypertension in chronic kidney disease: Consensus statement by an expert panel of Indian nephrologist. J of the physic. of Ind (suppl) pp. 6-22.
- Wong TY, Mitchell P (2004) Hypertensive retinopathy. N Engl J Med 351: 2310-2317.
- Frambach DA, Valentin JL, Weiter JJ (1989) Furosemide-sensitive CI transport in bovine retinal pigment epithelium. Invest Ophthalmol and Vis Sci (30): 2271-2274.
- Kita M, Michael F (1992) Effects on retinal adhesive force in vivo of metabolically active agents in the subretinal Space. Invest Ophthalmol and Vis Sci (33): 1883-1887.
- Cantor LB, Rapuano CJ, Cioffi GA (2016) Retinal vascular diseases in : American Academy of Ophthalmology, Section 12. Retina and vitreous. pp.145-146.
- Lang GK (2000) Degenerative retinal disorders In: Ophthalmology A Short Text Book. 3rd Ed Thieme. New York, USA. pp. 328-337.
- Quillen D, Blodi B (2002) Clinical retina in American Medical Association. United States. 136-137.
- Erden S, Bicakci E (2012) Hypertensive retinopathy: Incidence, risk factors and comorbidities. Clin Exp Hypertens 34(6): 397-401.
- Henderson AD, Biousse V, Newman NJ, Lamirel C, Wright DW, et al. (2012) Grade III or Grade IV Hypertensive Retinopathy with Severely Elevated Blood Pressure. West J Emerg Med. 13(6): 529-534.
- Tso MOM, Jampol LM (1982) Pathophysiology of hypertensive retinopathy. J Ophthalmol (89): 1132-1145.
- Frambach DA, Misfeldt DS (1983) Furosemide-sensitive Cl transport in embryonic chicken retinal pigment epithelium. Am J Physiol pp.244-246.
- DiMattio J, Degnan KJ, Zadunaisky JA (1983) A model for transepithelialion transport across the isolated retinal pigment epithelium of the frog. Exp Eye Res (37): 409-420.
- Tsuboi S, Pederson JE (1986) Experimental retinal detachment: Furosemide-Inhibitable fluid absorption across retinal pigment epithelium in vivo. Arch Ophthalmol (104): 602-603.
- Koo NK, Kim YC (2012) Resolution of macular edema after systemic treatment with furosemide. Korean J Ophthalmol 26(4): 312-315.
- Ciardella AP (2004) Partial resolution of diabetic macular edema after systemic treatment with furosemide. Br J Ophthalmol (88): 1224-1229.