Viplove Senadhi1*, Deepika Arora2, Dennis Emuron3, Manish Arora4 Andrew Ghaly5, Franklin Marsh6
1Johns Hopkins University/ Sinai Hospital Program in Internal Medicine, Baltimore, Maryland, USA
2Elmhurst Hospital/ Mount Sinai School of Medicine, New York City, New York, USA
3Mbarara University of Science and Technology, Mbarara, Uganda
4Mbarara University of Science and Technology, Mbarara, Uganda
5Saint Matthews University School of Medicine, Grand Caymen Islands, British West Indies
6Division of Gastroenterology, New York Hospital-Weill Cornell Medical Center, New York City, New York, USA
- *Corresponding Author:
- Viplove Senadhi
Johns Hopkins University/ Sinai Hospital Program in Internal Medicine
Baltimore, Maryland
USA
Introduction
Cancer is second only to Coronary Artery Disease in overall mortality in the United States. Amongst all the cancers, lung cancer is the most common and is associated with the highest cancer related mortality amongst both genders. Lung cancers present with metastasis about 50% of the time [1]. The most common sites of lung metastases include the adrenal glands, brain, bone, liver, lymph nodes, and the contralateral lung. However, gastrointestinal (GI) metastasis and manifestations are rare. Most of the reported cases of lung cancer metastasis to the gastrointestinal tract involve the small bowel (2-5) and occur through lymphatic spread. We present a rare case of a primary papillary (subtype) adenocarcinoma of the lung recurring as lower GI bleeding due to colonic metastasis.
Case Report
A 74 year old male with a past medical history of transfusion dependent anemia secondary to chronic kidney disease, a smoking history of 15 pack years, and an infiltrating papillary adenocarcinoma of the left upper lobe lung s/p resection was admitted for the management of severe symptomatic anemia. The patient presented with generalized body weakness and secondary acute on chronic renal insufficiency. The patient denied any abdominal pain, nausea, vomiting, melena, hemetemesis, anticoagulant/NSAID use and has never had any history of gastrointestinal bleeding in the past. Physical exam findings were positive for cachexia, conjuctival pallor and bilateral decreased air entry in the upper lobes. Rectal exam revealed hemoccult positive loose black stool while on iron therapy. The patient’s vital signs were within normal limits and were without any evidence of orthostasis. Laboratory findings revealed a hematocrit of 16 % with a MCV of 87 fl and a subsequent workup revealed possible acute blood loss. An elevated BUN of 95 mg/dl and creatinine of 4.7 mg/dl (patient’s baseline 3.3 mg/dl ) was attributed secondary to a pre-renal etiology from gastrointestinal bleeding. CT scan of the abdomen and pelvis revealed multiple pulmonary nodules, multiple hepatic lesions and a 3.2 cm X 2.5 cm intraluminal mass in the distal descending colon, which was concerning for a primary malignancy of the colon. Colonoscopy revealed a single large friable fungating mass in the hepatic flexure, which was consistent with the classic presentation of right sided colon cancer. Conservative management was undertaken until the patient was hemodynamically stable enough to be considered for a colonic resection. Surprisingly, the colonic biopsy revealed poorly differentiated papillary carcinoma and immuno-histochemical staining confirmed the tumor was primary, given the patient’s history of papillary adenocarcinoma lung, this finding was deemed compatible with a colonic metastasis from a primary lung cancer. Due to our patient’s comorbidities and in-hospital complications, surgery was postponed and unfortunately, the patient expired in the interval.
Discussion
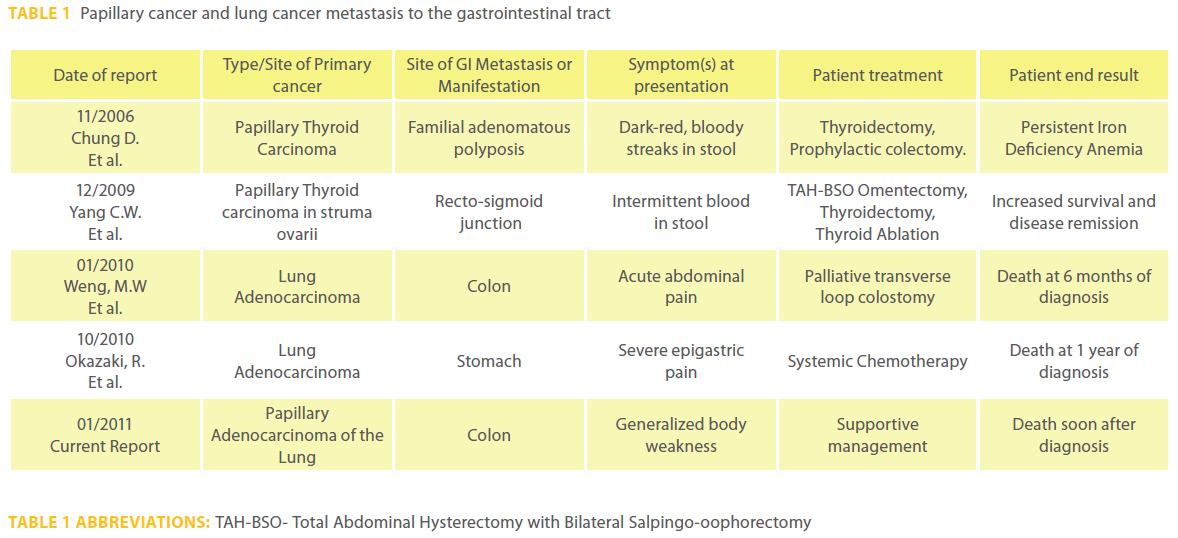
Papillary adenocarcinoma of the lung is one of the subtypes of non small cell lung cancer (NSCLC) and it arises from either mucin producing goblet cells, type 2 pneumocytes, or bronchial surface epithelial cells. Other common differentials in colonic papillary adenocarcinoma metastasis include primary malignancy from the thyroid, breast, and theoretically from biliary papillary cancer. However, lung cancer metastasis would be the most common overall cause of colonic papillary adenocarcinoma metastasis, given the overall prevalence of lung cancer. Table 1 summarizes the literature review with respect to papillary and lung cancer metastasis to the gastrointestinal tract.
Primary lung carcinoma metastasis to the GI tract is rare despite the prevalence at autopsy being about 4.7–14.0% (6, 7). The most common site of GI metastasis of lung cancer would be the small intestines, with metastasis to the stomach or colon occurring less frequently (2, 5, 8). Typically following diagnosis of a primary lung lesion, colonic metastasis usually occurs in the later stages of disease progression.
GI metastasis of lung cancer is a diagnosis that is usually asymptomatic and a diagnosis that is most likely obtained at autopsy (6, 7). Metastasis, initially is manifested in the submucosa and as the tumor expands, can cause symptoms. In a study by Yang et al, the clinical prevalence of symptomatic GI metastasis of lung cancer was about 1.77%(2). After the initial submucosal growth, and further growth of the tumor, the presenting symptoms that manifest are abdominal pain, nausea, vomiting, weight loss and anemia (9, 10, 11). These findings generally present after the diagnosis of the primary disease which was seen in our patient, but can occur synchronously or before the diagnosis of the primary disease (2, 10). Our patient manifested with severe anemia out of proportion to his anemia of chronic kidney disease and was most likely having subtle blood loss for a long period of time prior to his admission, which caused a pre-renal strain over the course of time.
GI metastasis from lung cancer can be highly variable in terms of symptoms, temporal relationship, and in terms of presentation. Occasionally, the lung primary and colonic lesion present synchronously (1). Lung cancer patients with GI metastasis have variable clinical presentations as described above, but can also present with upper GI bleeding, abdominal obstruction, abdominal perforation, fistula development, or peritonitis. Colonic polyposis following colonic metastasis has even been reported. Overall there is one universal factor with gastrointestinal metastasis from lung cancer, a high short-term mortality and a poor prognosis, as seen in our patient, who unfortunately passed away soon after. Lung cancer with GI metastasis has a poor prognosis regardless of choice of therapy, which is dependent on the extent of disease and the patient’s comorbidities. The role of surgical intervention is mostly palliative and improves the quality of life while decreasing the duration of hospital stay in cases of perforation, obstruction or bleeding. However, the overall goal of surgery is to achieve sufficient palliation (11). Unfortunately in our patient, surgery was not possible due to numerous comorbidities.
In summary, we describe a rare case of solitary colonic papillary adenocarcinoma metastasis presenting with lower GI bleed manifesting as symptomatic anemia in a patient with a previously resected lung papillary adenocarcinoma. We suggest that in patients with a history of lung cancer, a new onset of gastrointestinal bleeding be thoroughly evaluated for the implications of gastrointestinal metastasis on the overall prognosis and treatment of the patient.
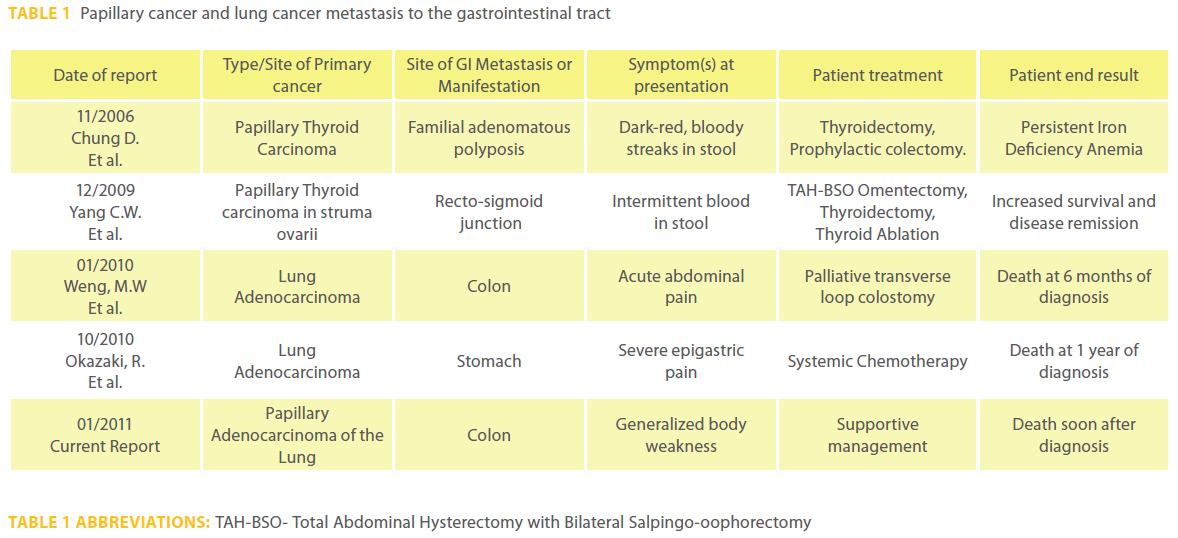
Table 1: Papillary cancer and lung cancer metastasis to the gastrointestinal tract
2550
References
- Weng MW, Wang HC, Chiou JC, et al. Colonic metastasis from a primary adenocarcinoma of the lung presenting with acute abdominal pain: a case report. Kaohsiung J Med Sci 2010; 26:40-4.
- Yang CJ, Hwang JJ, Kang WY, et al. Gastro-intestinal metastasis of primary lung carcinoma: clinical presentations and outcome. Lung Cancer 2006;54:319-23.
- Yilmaz S, Dursun M, Canoruç F, et al. Upper gastrointestinal bleeding caused by small-cell lung cancer: a case report. Dig Dis Sci 2006;51:788-90.
- Garwood RA, Sawyer MD, Ledesma EJ, et al. A case and review of bowel perforation secondary to metastatic lung cancer. Am Surg 2005;71:110-6.
- Carroll D, Rajesh PB. Colonic metastases from primary squamous cell carcinoma of the lung. Eur J Cardiothorac Surg 2001; 19:719-20.
- Antler AS, Ough Y, Pitchumoni CS, et al. Gastrointestinal metastases from malignant tumors of the lung. Cancer 1982;49:170-2.
- McNeill PM, Wagman LD, Neifeld JP. Small bowel metastases from primary carcinoma of the lung. Cancer 1987;59:1486-9.
- Yamamoto M, Matsuzaki K, Kusumoto H, et al. Gastric metastasis from lung carcinoma. Case report. Hepatogastroenterology 2002;49:363-5.
- Ahn SE, Lee HL, Lee OY, et al. [Colonic metastasis from primary lung adenocarcinoma]. Korean J Gastroenterol 2009;53:121-5.
- Berger A, Cellier C, Daniel C, et al. Small bowel metastases from primary carcinoma of the lung: clinical findings and outcome. Am J Gastroenterol 1999;94:1884-7.
- John AK, Kotru A, Pearson HJ. Colonic metastasis from bronchogenic carcinoma presenting as pancolitis. J Postgrad Med 2002;48:199-200.