Keywords
Mama; Breast neoplasm; Mastectomy
Introduction
Breast cancer occurs due to abnormal and exacerbated development of the breast cell, which suddenly multiplies until form a malignant tumor cell. Nowadays, breast cancer is considered the most common cancer among women, causing functional and psychological consequences, and is the leading cause of death by malignant neoplasm [1].
In 2018, 59.700 new cases of breast cancer were estimated in Brazil [2]. For the years 2020-2022, there is already an estimate of 66.000 new cases/year in the country [3]. There is still no direct relationship between breast cancer and its causative agents. Its etiopathology is still unknown, however, it is believed that there is an interaction between pre-existing genetic factors, which influences the increased risk of morbidity, and environmental factors, such as: exposure to ionizing radiation, hormone therapies, age, alcohol consumption, dietary factors, reproductive history, menopause after age 55, use of contraceptives containing estrogen and/or progesterone, and genetic alteration of the BRCA1 and BRCA2 genes, which create conditions that favor the onset and development of cancer [2,4].
The signs and symptoms of breast cancer can vary. Can presents a single hardened nodule, irritation of a part of the breast, sensation of an enlarged nodule in the axillary region, bloody or serous discharge from the nipple, breast pain and secondary infections [5]. From the positive diagnosis of the disease, which includes mammography, biopsy, and ultrasonography, the specific treatment plans for each patient are outlined. In addition, the degree of involvement is included with the excision of the nodule with radiation and partial mastectomy. This consists of removing a small part of the normal tissue around the nodule and the axillary lymph nodes, or total, with the total removal of the breast, which is the most commonly, used surgical method [6,7].
The surgery for the removal of the breast has a great impact on the lives of these women, due to the impairment of the physical functioning and mainly because of the psychosocial distress. It is understood that breast cancer causes an emotional shock in a much more relevant way than any other cancer. These women present a functional and aesthetic limitation, which causes an immediate physical and psychological repercussion, constituting a traumatic event for the majority of mastectomized women [8].
After the mastectomy, it is recognized that the disfigurement and breast asymmetry caused by the surgery affects the psychological state of women with breast cancer, mainly making them depressed [9]. After this procedure, these patients can undergo total breast reconstruction, through implantation and with the help of micro pigmentation. In this way, there is the possibility of recovering the self-esteem of patients who have undergone mastectomy and improve the quality of life [10].
Among these methods used in the health area, there is the areola micro pigmentation, which is used to improve the aesthetic appearance of the breast, with high rates of satisfaction due to the improvement on the body image [11]. However, although it is a safe and simple procedure, it can trigger allergic reactions and scars, so one should seek a qualified micropigmenter who can perform the areola micro pigmentation, highlighting the important role of this professional in the treatment of these women [10].
Micro pigmentation or permanent makeup is a technique that uses a dermograph device performs to the deposition of intradermal pigments according to the tissue coloration, allowing the areola to return to the previous original color tone, in addition to scar camouflage and a good symmetry [12]. This procedure is an important factor for the recovery of women undergoing the surgical process of mastectomy by promoting improvement in the visual aspect of the areola and nipple, highly related to the patient's overall satisfaction and acceptance of the own body, with better perception of self-image, well-being, and quality of life [13].
Thus, considering the need for enhance the self-esteem of these women, this study proposed to verify the influence of paramedic areola micro pigmentation on the quality of life of mastectomized women.
Materials and Methods
This is a clinical, longitudinal, prospective study with a qualitative and quantitative approach. The study was carried out in Belém city with female patients from the Caroline de Siqueira Mendes Micro pigmentation and Aesthetics Center. This study was submitted and approved by the Research Ethics Committee of the Pará State University under advice No. 3.670.891.
The sample consisted of 15 volunteers who signed the Informed Consent Form (ICF). The patients were aged between 30 and 70 years, who underwent mastectomy within 12 months, followed by breast reconstruction within 24 months. These patients sought paramedical areolar micro pigmentation treatment after breast reconstruction and consequently the medical clearance from their oncologist for such a procedure.
Patients who underwent mastectomy without removal of the areola were excluded from this study. In addition, those who had associated tissue pathologies, allergies to the pigment, difficulty in understanding the procedure, or some cognitive deficit by the Mini Mental State Examination, scored less than 23. Also excluded were patients who were still undergoing radiotherapy or chemotherapy and with less than six months of breast reconstruction.
For breast evaluation, images were taken before and after the micro pigmentation procedure, in the seated position. The camera used was an iPhone 7 Plus which was positioned one meter away from the breasts, with a flat background and uniform color. Afterwards, the Breast Cancer Scale - FACT-B-Version 4 was applied, and then the specific questionnaire for breast cancer, called FACT - B (Functional Assessment of Cancer Therapy - Breast). This consists of 36 questions, 27 of which refer to general quality of life (FACT-G) and nine to problems specific to breast cancer patients. The questionnaire is composed of six domains: Physical Well-being (PWB), Social/family Well-being (SFWB), Emotional Well-being (EWB), Functional Well-being (FWB), and Additional Concerns (AC) (breast cancer and arm). The answers are presented on a five-point Likert scale, where the higher the score, the higher the patient's quality of life.
The calculation of the score for this instrument was performed separately for each domain. The score was calculated by summing the questions in each domain. To keep score meaning, some questions were reversed, that is: PWB1 to PWB7, EWB1 to EWB3 to EWB6, AC1 to AC3, AC5 to AC8, and AC10: PWB1 to PWB7, EWB1, EWB3 to EWB6, AC1 to AC3, AC5 to AC8, and AC10... After calculating the formula for each domain, the results were summed to obtain the final score, which ranges from 0 to 284. In case any question is not answered, the assumed value for it will be the average of the answers from that domain. For this reason, first the average of the questions answered is taken and then this result is multiplied by the number of questions in the domain [14].
Another instrument used was the EORTC QLQ - BRECON23 questionnaire on quality of life after breast reconstruction. It consists of 23 questions, which are subdivided into six categories: I) about symptoms and problems (12 questions); II) for patients who had nipple conservation (02 questions); III) for patients who underwent total breast reconstruction (3 questions); IV) for patients who underwent tissue removal procedures for breast reconstruction (4 questions); V) for patients with nipple loss or who did not undergo nipple reconstruction (01 question) and VI) for patients who underwent surgery conservation or recovery exercises (01 question). The questionnaire was given to the participants who marked options from 01 (not at all) to 04 (quite a lot), according to the command of the questions and according to the events post breast reconstruction.
As described in the EORTC QLQ - BRECON manual, to calculate the Score, the points can be transformed from 0 to 100, where zero represents the worst health condition and 100 the best health condition. It should be added that the symptoms scale is excluded, in which the higher the score, the worse the quality of life. Therefore, an evident score on the functional scale indicates that the patient has a healthy functional level. And if the score is high on the symptom scale, the patient has a high degree of symptoms and side effects [14].
For the paramedical micropigmentation procedure, the volunteers were positioned in sedestation for asepsis with 70% alcohol or alcoholic chlorhexidine on the entire extent of the breast. Afterwards, a perimetry of the breast was performed with a GR® pachymeter, which enabled the symmetry of the area to be pigmented. After a symmetrical analysis of the breasts, a dermographic pencil drawing was made to simulate the areolas that were micropigmented.
The patients were positioned on a stretcher in dorsal decubitus, with inclination varying from 30º or neutral, according to the patient's comfort. Then the patients were covered with disposable lab coats, which contained the hole in the direction of the breast to be micropigmented. The professional responsible for the micropigmentation was properly equipped with a disposable hood, glove, disposable cap and mask, sterile gloves, and a lab coat.
It was applied on the areola of the patients, anesthetic formulated by VICTA®, containing Lidocaine 40% and occlusion of the region with film paper for 15 to 20 minutes for the effect of the anesthetic. Afterwards, the field was prepared with a dermograph, using a 3-point and a single-point needle, as well as the MAG® brand pigments. Subsequently, a mixture of colors was performed, according to the tone of the adjacent areola and/ or the patient's desire. With this, the composition of different shades of the breast was avoided.
The central region of the nipple was pigmented with a lighter color to create an illusion of projection and thus using the pendulum technique, which consists of positioning the device at 45°. With short movements, the filling of the breast started from the external edge, towards the center, thus providing a degrade and areolar formation. At the end each patient received guidance on the care to be taken for the best result of micropigmentation. These patients were advised to return within 15 days for a re-evaluation of the area. And, if necessary, retouching of the micropigmented area would be performed, since the pigment is not always uniform.
All data obtained from the participants were processed (grouped and sorted) in a Microsoft Excel software spreadsheet version 2016. To compare the mean scores obtained in the EORTC-BR23 and FACT-B instruments, they were analyzed using descriptive statistics by means of measures of position and variability (mean, standard deviation and minimum and maximum values). ANOVA variance analysis with Tukey's test was used for sample characterization and for the questionnaires, considering p<0.05.
Results
Table 1 expresses the mean values referring to the characterization data of the sample regarding the discovery of the disease, the Mastectomy, Reconstruction and Paramedic areolar micropigmentation. It was observed that the mean intervention period from the discovery of the disease to the paramedical areolar micropigmentation procedure was ±4 and the standard deviation was 3.10 years (p<0.05).
| Variable |
Mean (µ) |
±DP |
Minimum |
Maximum |
| Age |
51.87 |
12.13 |
34 |
70 |
| D - M (months) |
12.9 |
35 |
0 |
124 |
| M - R (months) |
9.6 |
9.91 |
0 |
26 |
| R - Mic (months) |
18.31 |
10.45 |
5 |
39 |
| D - Mic (years) |
3.64 |
3.104 |
0 |
11 |
Source: Data resulting from the research (2020).
D=Discovery of disease; M=Mastectomy; R=Reconstruction; Mic=Micropigmentation.
Table 1 Age and mean time between disease discovery, mastectomy, reconstruction and paramedical areolar micropigmentation.
The results of the EORTC-BR23 questionnaire showed that, for the evaluation scale of the quality of life of women after breast reconstruction, in the item III (μ=100.00) and IV (μ=60.3), the volunteers presented the highest scores. Considering that the higher score, the better the satisfaction with the quality of life after the reconstruction procedure, resulting in a higher degree of satisfaction in these domains (Table 2). It can be seen that for the scores, item I- side effects of treatment (μ=16.67) and item II - symptoms at the site of removal (μ=33.3), the women showed a low level of symptomatology or problems. While in scores VI - satisfaction with nipples (μ=31.0) and IV - sexual function (μ=37.2), there was a significant drop in scores, indicating a low degree of satisfaction of women in these aspects.
| Domain |
Items |
N |
N* |
Mean (µ) |
±DP |
Minimun |
Maximum |
| Symptomatology or Problem Scales |
Item 1 |
15 |
0 |
16.66 |
17.8 |
0.0 |
50.0 |
| Item 2 |
1 |
14 |
33.33 |
* |
33.3 |
33.3 |
| Item 3 |
15 |
0 |
100.0 |
0.0 |
100.0 |
100.0 |
| Functional and Satisfaction Scales |
Item 4 |
15 |
0 |
37.22 |
7.6 |
25.0 |
50.0 |
| Item 5 |
15 |
0 |
60.31 |
15.1 |
33.3 |
90.5 |
| Item 6 |
14 |
1 |
30.95 |
31.3 |
0.0 |
100.0 |
| Item 7 |
14 |
1 |
56.34 |
3.0 |
55.6 |
66.7 |
| Item 8 |
2 |
13 |
33.33 |
47.1 |
0.0 |
66.7 |
| P-Value(1) |
|
|
|
0.000* |
|
|
|
Source: Research protocol (2020).
Table 2 Scores obtained in the domains of the EORTC-BR23 questionnaire by mastectomized women and women with breast reconstruction after the areolar paramedic micropigmentation procedure.
Table 3 shows the mean values of scores obtained in the domains of the FACT-B questionnaire, for mastectomized women and women with breast reconstruction after the paramedic areolar micropigmentation procedure. It can be seen that the Additional Concerns (AP) domain was better evaluated, obtaining a mean value of 215.16 ± 35.37. The satisfaction of women was lower in the domains, social/family well-being (SFWB) with mean score equal to 23.64, and functional well-being (FWB) with mean score equal to 18.13 (p<0.05).
| Variable |
N |
N* |
Mean |
Standard Deviation |
Minimum |
Maximum |
| 1 - Physical well-being (PWB) |
15 |
0 |
144,83 |
22,41 |
116,00 |
172,00 |
| 2 - Social/family well-being (SFWB) |
15 |
0 |
23,64 |
5,92 |
4,67 |
28,00 |
| 3 - Emotional well-being (EWB) |
15 |
0 |
74,16 |
15,25 |
43,20 |
99,60 |
| 4 - Functional well-being (FWB) |
15 |
0 |
18,13 |
6,85 |
7,00 |
28,00 |
| 5 - Additional concerns (AC) |
15 |
0 |
215,16 |
35,37 |
153,00 |
284,00 |
| P-Value(1) |
|
|
0.000* |
|
|
|
Source: Research protocol (2020).
Table 3 Descriptive statistics of the scores obtained in the domains of the FACT-B questionnaire, by mastectomized women and women with breast reconstruction after the areolar paramedic micropigmentation procedure.
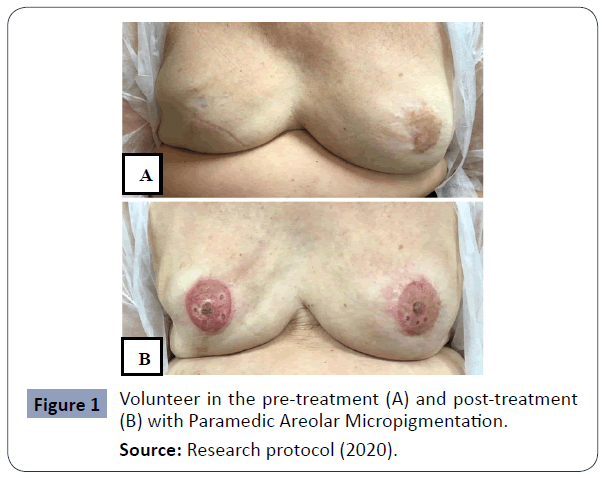
In analyzing the qualitative data, Figure 1 expresses pre- and post-treatment paramedic micropigmentation images of one of the volunteers. It is observed in position A the pre-treatment, the absence of areolas and bilaterally well-defined nipples. The position B corresponds to the post treatment with micropigmentation in the areolae regions and nipple reconstruction. What demonstrates symmetry between the breasts, coloring considering the phototype of the patient's skin with choice of the correct pigment, which provided a natural appearance of the breasts.
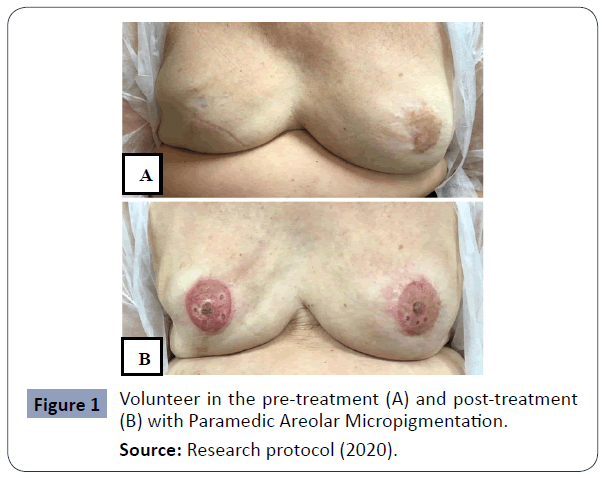
Source: Research protocol (2020).
Figure 1 Volunteer in the pre-treatment (A) and post-treatment (B) with Paramedic Areolar Micropigmentation.
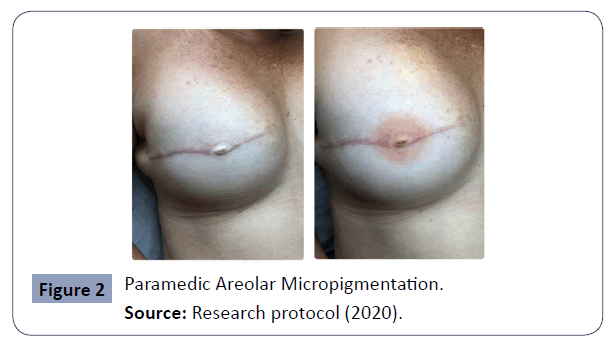
Figure 2 expresses pre and post-treatment paramedic micropigmentation images of another volunteer. Position A corresponds to the pre-treatment. It is observed the absence of the areola of the right breast, however, with preservation of the nipple. In position B is observed the post-treatment with the areolar reconstruction of the right breast. In this case it was preserved, considering the colorations according to the skin phototype and the gradation of the tones used, which provided a natural aspect of the breasts.
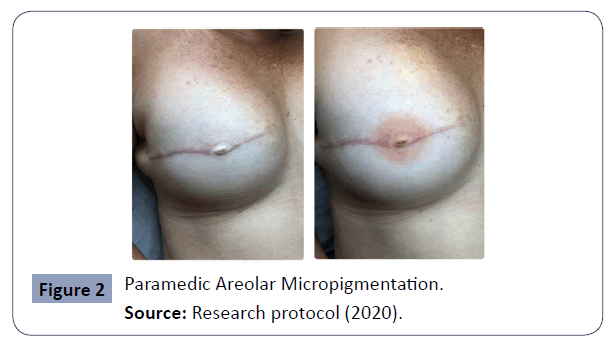
Source: Research protocol (2020).
Figure 2 Paramedic Areolar Micropigmentation.
Discussion
Despite breast cancer not having only one specific cause, age remains the main risk factor for the onset of the disease. This incidence increases rapidly until age 50 and after that age, the increase becomes slower [15]. In this study, the age range of mastectomized women who underwent breast reconstruction and consequently paramedical areolar micropigmentation was 51.87 ± 12.13 years. This corroborates with the study of Odom et al. [16], which presented a mean of 50.2 years. Furthermore, it was observed in the present study that the women went through a long period from the discovery of the disease to the submission of micropigmentation. However, it is worth mentioning the lack of studies related to this period of time in the databases, which did not allow discussing this result.
With regard to the quality of life after breast reconstruction, according to the EORTC-BR23 questionnaire, the results of this study showed that the women presented better satisfaction with their quality of life, supposing that the results obtained through the questionnaire showed an increase in their self-esteem and a better visualization of their self-image and sexual function. Despite this, breast cancer still occupies a prominent place among malignant neoplasms worldwide, compromising self-esteem and interfering with their self-image due to the loss of the organ [17].
In some mastectomy procedures the natural nipples are preserved in an attempt to maintain a natural appearance. However, the study presented here showed that although the women showed low rates of symptomatology at the site of the breast removal, as well as few side effects of the treatment, they were dissatisfied with their natural nipple due to imperfections resulting from the surgery. According to Hirschle et al. [17] imperfections negatively interfere with women's sexuality and compromises their sexual performance. In addition, the studies by Mastroianni et al. [18] showed that most women decide to preserve their nipple, however, unfortunately some may lose them due to oncological reasons or necrosis.
Regardless of the time of discovery and surgery that the patients underwent, significant differences were found regarding the degree of satisfaction of these women who underwent the paramedical areolar micropigmentation procedure. These results are consistent with the scopes clarified in the study by Hirschle et al [17] who evaluated how the micropigmentation procedure for areola reconstruction had gone. Differences were found between the quality of life of those who had undergone the procedure and those who had not. In this way it is concluded that these women who chose to perform the procedure, were much more satisfied, having increased self-esteem and better perception of their body image.
As for the scores obtained through the application of the EOTIC-BR23 questionnaire for the evaluation of the quality of life, the present study has a significant difference in the degree of satisfaction between the domains, as well as in the symptomatologies or problems. With this, a good degree of satisfaction with the quality of life in breast reconstruction is shown. However, despite having shown low side effects and symptomatology at the site of withdrawal, these women showed a drop in satisfaction regarding satisfaction with the nipple after reconstruction and sexual function. In the study of Silva, Ferreira, Costa, & Pernambuco [19] presented as a mean score in the Symptomatology or Problems Scale, the result of 24.47 ± 14.87, as for the Functional Scales and satisfaction, the score was 27.23 ± 16.11.
With regard to the FACT-B questionnaire in the present study, regarding the physical well-being aspect, considering the scores obtained, they were well evaluated regarding quality of life, however, the social and family well-being domain obtained a low score. This differs from the study published by Cordeiro, Nogueira, & Gradim [20], where they showed results with lower scores regarding physical well-being, social/family well-being, emotional well-being, functional well-being, and additional concerns subdivided into breast cancer and with the arm, that is, the women who participated in the research tended not to present a good quality of life.
It is important to analyze that the study obtained positive results regarding the evaluation of the quality of life of women who underwent paramedical areolar micropigmentation. However, with regard to sexual function after reconstruction, this quality of life ends up being impaired. Due to this, after the micropigmentation, the women present a great satisfaction. Corroborating the study of Faria et al. [21] which points out that the greatest fear of women affected by this disease is still the fantasy of no longer being sexually attractive and, after consecutive micropigmentation surgery, comes the feeling of satisfaction.
After obtaining the results regarding the paramedic areolar micropigmentation, it can be observed that the application of this technique in mastectomized women and with breast reconstruction has been growing more and more. Both with the method of application, and with the valorization of the technique by health professionals. This technique, besides being recommended for women submitted to breast reconstruction, is also indicated for the improvement of the scar and intensification of the areolar coloration, which has a variability of tones that allows one to approach the natural coloration of the nipple.
The qualitative results of this study corroborate and prove the aforementioned reports, since the self-esteem of women in this study increased, which modified their quality of life after paramedical micropigmentation for having a positive self-image regarding the conformity of their breast and natural appearance designed the areolas and nipples with the proposed technique, besides presenting a reinsertion in the social context.
The search for areolar micropigmentation has as a common goal, the increase in self-esteem and the improvement of body image, for being a technique that has promising results and with scientific basis for its application, in addition, the application of the pigment in the region does not interfere in the clinical history of the patient regarding breast cancer, however, it must be performed after medical recommendation. The pigments used are applied in the sub-epidermal layer of the skin and, although its application is similar to tattooing, the pigment reaches only the superficial layer of the epithelial tissue.
Conclusion
It is believed that the study could contribute to a better understanding about the quality of life of mastectomized women who underwent paramedic areolar micropigmentation. Unfortunately, the lack of sample-based data on paramedic micropigmentation made it impossible to make a comparison with other studies. In a way, the research carried out fills the existing gap in the literature on the subject. It is concluded that the absence of this organ for women is unacceptable, due to this,micropigmentation after breast reconstruction becomes satisfactory, making them feel included in society, returning their self-esteem and improving their self-image after the impact of the disease.
36602
References
- de Oliveira ARD, Moraes DG, da Consolação JP, Mélo FML (2017) Physical therapy resources used in the postoperative period of mastectomized women. Physiotherapy Brazil 18: 514-520.
- Ministry of Health (2018) Breast cancer: symptoms, treatments, causes and prevention. Brazil.
- Kolak A, Kamińska M, Sygit K, Budny A, Surdyka D, et al. (2017). Primary and secondary prevention of breast cancer. Ann Agric Environ Med 24: 549-553.
- Batista DRR, de Mattos M, da Silva SF (2015) Livingwith Cancer: From Diagnosis to Treatment. Revista de Enfermagem da UFSM 5: 499-510.
- Ryan R, Tawfik O, Jensen RA, Anant S (2017) Current approaches to diagnosis and treatment of ductal carcinoma in situ and future directions. Prog Mol Biol Transl Sci 151: 33-80.
- Silva MB, Júnior JMP, Miranda FAN (2016) Life trajectory of mastectomized women based on the collective subject discourse. Revista Online de Pesquisa Cuidados Fundamentais 8.
- dos Santos MS, Freitas DDFL, Andrade JSO, da Silva FML (2019) Implications of mastectomy for women's self-esteem. Revista Eletrônica Acervo Saúde 29: e1124-e1124.
- Zhang C, Hu G, Biskup E, Qiu X, Zhang H, et al. (2018) Depression Induced by Total Mastectomy, Breast Conserving Surgery and Breast Reconstruction: A Systematic Review and Meta-analysis. World Journal of Surgery 42: 2076–2085.
- Casassola GM, Gonçalves GR, Stallbaum JH, Pivetta HMF, Braz MM (2020) Physiotherapeutic interventions used in the functional rehabilitation of the upper limb of women after mastectomy. Fisioterapia Brasil 21: 93-103.
- Obasi J (2019)Micropigmentation of the nipple–areola complex after breast cancer reconstruction surgery. Oxford medical case reports 8: 367-368.
- Simonacci F, Bertozzi N, Pesce M, Santi PL, Raposio E (2018) Areola Reconstruction: Principles and Techniques. Open Medicine J 5: 84-92.
- Paoliello H, Paoliello R (2018) Aesthetic Repair of Nipple and Areolar Abnormalities. Breast Surgery pp: 575–586.
- Michels FAS, Latorre MRD, Maciel MDS (2013) Validity, reliability and understanding of the EORTC-C30 and EORTC-BR23, quality of life questionnaires specific for breast cancer. Rev Bras Epidemiol 16: 352-363.
- Ministry of Health (2019)Estimate 2020: incidence of cancer in Brazil. National Cancer Institute.
- Odom EB, Sharma K, Grant DW, Buck DW, Myckatyn TM (2017) A Retrospective Cohort Study on Payor Type and the Effect on Revisions in Breast Reconstruction. Plast Reconstr Surg 140:527e-537e.
- Hirschle TMR, Maciel SC, Amorim GKD (2018)Social Representations about the Body and Sexual Satisfaction of Mastectomized Women and their Partners. Trends in Psychology 26: 457-468.
- Mastroianni M, Lin AM, Smith BL, Austen WG, Colwell AS (2016) Nipple loss following nipple-sparing mastectomy. Plast Reconstr Surg 138: 24e-30e.
- Silva FC, Ferreira LJ, Costa CM, Pernambuco AP (2018)Evaluation of quality of life in women with breast cancer submitted to surgical intervention. Physiotherapy Brazil 19: 524-531.
- Cordeiro LDAM, Nogueira DA, Gradim CVC (2018)Women with breast cancer in adjuvant chemotherapy: assessment of quality of life. Revista Enfermagem UERJ 26: 17948.
- Faria NC, Fangel LMV, Almeida AMD, Prado MAS, Carlo MMRDPD (2016) Psychosocial adjustment after mastectomy- a look at the quality of life. Psic Saúde Doenças 17: 201-213.