Keywords
Immunisation, health policy, mass media, interpersonal communication
Introduction
The development and use of vaccines has been one of the greatest achievements in public health over the past two centuries [1]. Childhood immunisations are the most cost-effective medical intervention to prevent death and disease [2]. Not solely a good in itself, childhood immunisation represents the gateway provisioning of comprehensive health care to all children.
Most parents in high-income countries have little or no first-hand knowledge of the childhood diseases that vaccines prevent. The mass media have been called upon to play a major role in promoting health for all for decades [3,4]. In recent years, the mass media are increasingly popular as a strategy for delivering preventive health messages [5,6]. Some have taken up this challenge with 'evangelical enthusiasm', without any regard for the decades of research and experience in the use of mass communication for public health education [7,8]. The success of the mass media in the commercial sphere is often thought to be directly applicable to influencing health behaviour, although advertising usually aims at modifying pre-existing patterns, whereas public health programmes are often concerned with changing deeply rooted attitudes and behaviours [7].
In the past, communication strategists often developed by assuming a smooth causal relationship between messages beamed, consumer attitudes and knowledge, and ultimately improved health practices [9]. A recent review by Wakefield et al., [6] highlighted that high proportions of large populations are exposed to messages through the mass media, such as television, radio, and newspapers. Exposure to such messages is generally passive.
Narula [10] suggested that government communication channels should act more responsibly than private ones in regard of development support communication practices. Government-controlled mass communication channels like, radio, television, and official interpersonal channels like block infrastructure and programme specialists have more credibility than non-government channels like press and films or friends, or relatives.
Media advocacy has become an established health promotion strategy, partly due to the influence of Ottawa Charter for Health Promotion [11]. It has become common to seek a ‘partnership’ or ‘shared agenda’ [12] with the mass media in communicating health information to the public, particularly in the area of prevention, risk reduction, and drug information [13]. Proponents of ‘media advocacy’ for the exposure of health-related messages, accuracy and media responsibility in order to set the media agenda (framing for access), shape the media debate (framing for content), and advance healthy public policies [14].
More recently the media have also played a role in raising doubts about immunisation. Most famously through the hype around the now discredited research by Wakefield et al [15]. The latter research suggested that immunising children with three different virus strains at the same time could affect a child's immune system and lead to autism and bowel disorder [16]. As a result of this research and the media furore around it vaccination rates dropped in the UK, USA and Germany to name but a few countries [17].
Mass Media Health Promotion in Nepal
In Nepal, media exposure is higher for men than for women [18]. For example; over 60 percent of Nepali women are exposed to the radio and 40 percent watch television at least once a week. Women’s exposure to the print media is relatively low. Only one in ten women read a newspaper or magazine at least once a week (NDHS, 2006). Only eight percent of women were exposed to all three types of media, while 30 percent of them are not exposed at all to any of the three media [18].
The National Health Education, Information and Communication Center (NHEICC) was established in 1993. Under the Ministry of Health & Population the NHEICC acted as a focal point to coordinate the media and the health programme of the government. NHEICC is currently using government owned Radio Nepal and Nepal Television at national level to cover its informative health programme, radio and TV drama [19]. NHEICC has recognised importance of community radio (FM) for local information and education programmes for specific target populations.
In a developing country like Nepal with a low literacy rate and lacking a planned health promotion system, the saturated media market can be the most feasible vehicle to transmit the information from the service provider to the target population [20].
Use of newspaper for the dissemination of health information to a mass audience has not been properly addressed in Nepal as radio was prioritised due to its nationwide accessibility. When resources allowed NHEICC has also imparted information through TV channels.
Within health communication and education, inter-personal communication is regarded as stronger than mass media because of its non-linear model and possibility of understanding the message. For the inter-personal communication practices, most of the health policy and programme from the government has recognised its role to play for the deeply rooted traditional beliefs that is being obstacle to adopt modern health care facilities. To address the communication need of multi-ethnic and multi-lingual community of the country inter-personal communication is highly prioritized. For the flow of information on immunisation in the local level, FCHVs (Female Community Health Volunteers), mothers’ groups, peer groups (young mothers), high school pupils and school teachers are the focal point. These target groups are trained by the national health training programme on key health issues with assistance of IEC (Information, Education and Communication) in full on first use) materials.
Different national health plans and policies have suggested the interpersonal communication channel and as well as mass media to create awareness on this type of information. The effectiveness of specific communication strategy in health sector, a timely review and implementation practices is also a problem. We do not know the popularity and effectiveness of current health programme and media components delivered through different media. There is gap on how the interpersonal communication network is working to educate people on immunisation issues.
This study has focused on national immunisation strategy from a communication perspective regarding the effectiveness of an interpersonal communication channel and mass media networks set under the immunisation programme. Parents' knowledge, attitude and practice are associated with immunisation coverage among their children. However, the role of family who ensure that children are immunised has not yet been studied in Nepal.
The main aim of the present study was to examine the sources of information for parents on childhood immunisation in Kathmandu Valley; and these parents’ knowledge and practices on childhood immunisation.
Methods and Materials
Quantitative research method was used for this explorative study. Using stratified quota sampling methods, participants were selected from three areas (urban, semi-urban and urban-slum areas) of Kathmandu district [21]. A total of 120 parents with at least one child below the age of five were selected; half male and half female. The first author visited door-to-door to identify the possible respondents. Sample size is calculated using web based sample size calculator.
The structured questionnaire was designed using already validated questions from WHO and Demographic and Health Survey (DHS). DHS has a section on children’s health, which cover immunization related issues. Nepal Demographic Health Survey (NDHS) questionnaire related to immunization was already validated questionnaire which was used in 1996, 2001, 2006 and 2011 for Nepal Demography Health Survey. No statistical validation was performed for the research instrument as this was already validated questionnaire used for national level in the past.
Structured questionnaire has two sections, starting with socio-demographic information, and followed by questions on parents’ knowledge and practices towards childhood related immunisation. The vaccine schedule recommended under the EPI programme for every child under the age of one was asked to parents. Those parents who correctly answered the number of required dose was categorised as having a good level of knowledge. Similarly, those parents who answered the number of required dose incorrectly was categorised as having poor knowledge.
Questionnaire data were coded, checked and cleaned before entering into SPSS (version 18.0) for analysis.
A pilot study provides advice for the study as well as helps to identify possible problems and solution [22]. The pilot study was conducted by distributing the questionnaire to the parents in Kathmandu prior to the main study. The pilot study participants were requested to comment on structure, language clarity and organisation of the questions. Ten responses were received and based on these the order of questions was slightly changed and some multiple-choice questions were rephrased.
Ethical approval was awarded by the Central Department of Mass Communication and Journalism, Tribhuvan University, Nepal. The study was both confidential and anonymous as was clearly stated on the questionnaire.
Results
Socio-demographic information about respondent
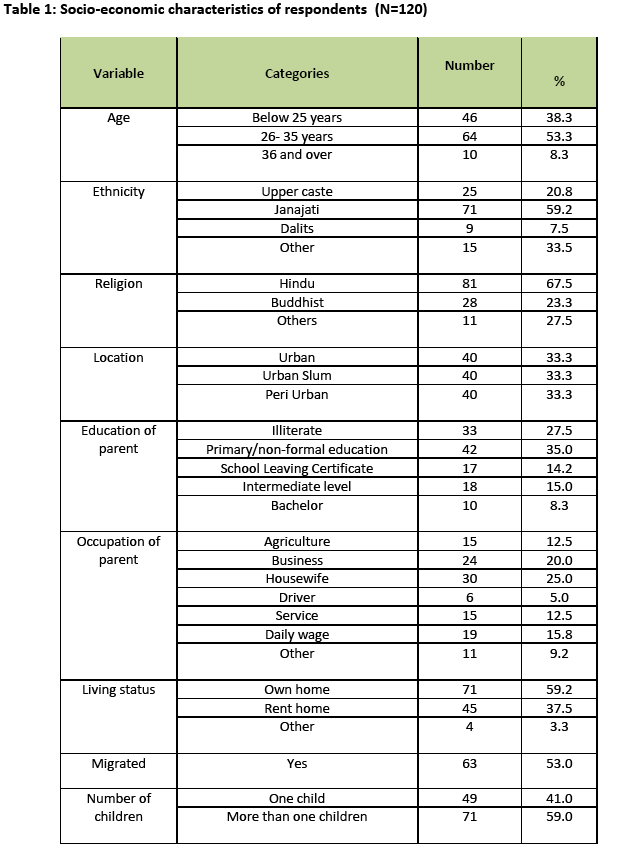
There was equal number of male (n=60) and female (n=60) participants, and slightly more parents were age 25 and younger than older than 26, less than 10% of parents were age 36 and over (Table 1). The majority of respondents were from the Janajati community, most were Hindu and a minority was Buddhists. One-third was illiterate, whilst most attended only primary education.
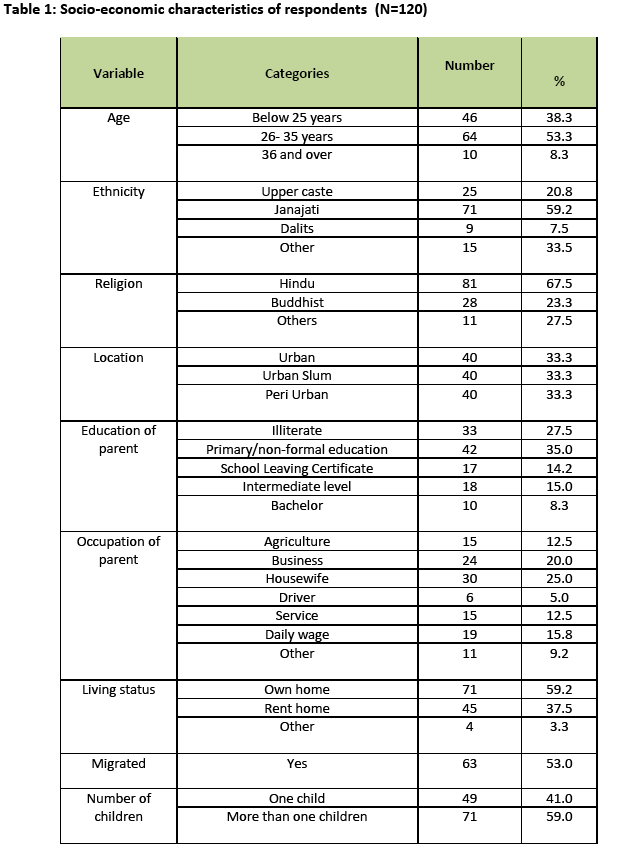
Housewives represented 25 % (n=30) of the total sample while 20% (n=24) were engaged in business, 12.5 % (n=15) were associated with agriculture. Most (71%) abode in their own house, whereas 53% (n=63) were migrants, and most respondents had more than one child.
Source of Information
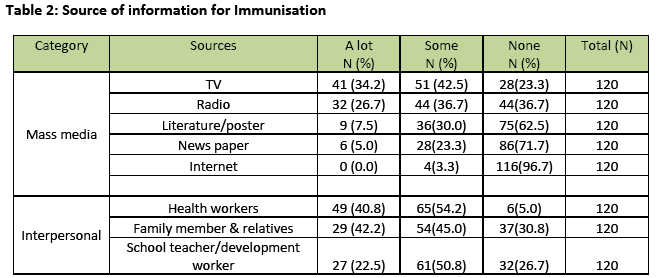
Our study suggests that health workers were the major source of information on immunisation. The respondents from urban area might have the effects on the national aggregate picture. This finding shows the importance of the communication in interpersonal level that it primarily means sharing and making the message or content common. The companionship influence has close connection with this finding. Health workers including doctor, nurse and FCHV have been recognised as a key channel of interpersonal health communication. Thus radio, TV, newspapers and the internet acted as a mass media source and health worker, family and the development worker facilitated the interpersonal communication.
Forty percent of the respondents tagged health workers as their main source of information, and more than half (54.2%) received some information form health workers on immunisation (Table 2). At the same time, few said that health workers were not a source of information on childhood-related immunisation. Less popular sources of information were TV, radio, literature and posters, newspapers and the internet. One-third (35.2%) of respondent received a lot of information from the TV.
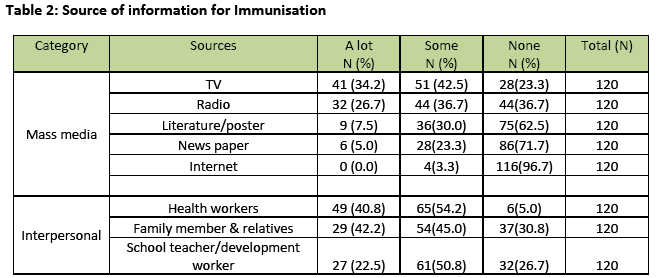
It has been found that one-quarter (24.2%) relied on family members and relatives for information on childhood-related immunisation. Another 22.5 percent had received such information from teachers and development workers as their major source of information.
The finding clearly shows that the highly prioritised IEC (information, education and communication) materials like handy literature and posters, has nominal effect on respondents as a source of information. The majority (62.6 %) had not received any information from these materials.
Newspapers were also marked as a non-effective means of communication on immunisation issues. Most respondents (71.7%) did not get any information from newspapers on immunisation. Generally parents of young children have little access to new media (internet) and only a negligible proportion (only 3%) use it to get the information on immunisation.
Knowledge about childhood Immunisation
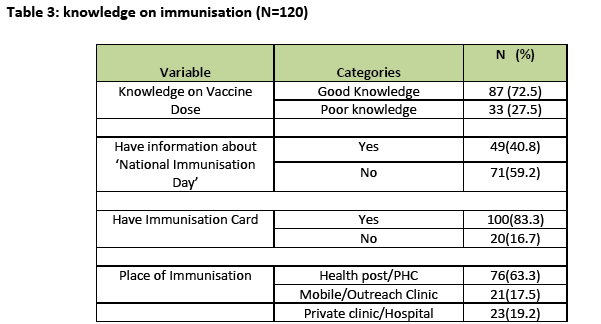
Table 3 shows that the parents’ knowledge on immunisation. The vaccine schedule recommended under the EPI programme for every child under the age of one was asked to parents. Most (72.5%) correctly answered the number of required dose, which was categorised as having a good level of knowledge. The advocacy based ‘National Immunisation Day’ is asked here to know about their exposure to this mass event, most (59.2%) had not heard about National Immunisation Day.
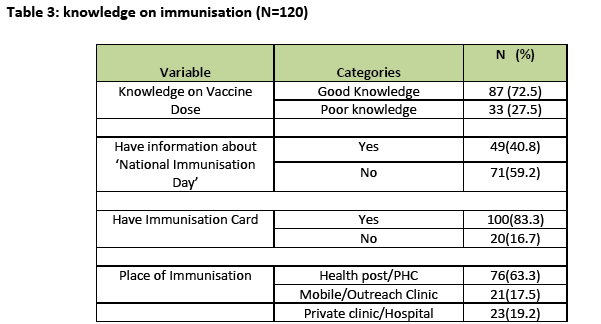
Parents of vaccinated children are suggested to keep the immunisation card at least till their children are five to observe the record whether the vaccine preventable diseases working to him/her or not. Most (83.3%) had kept the immunisation card of their last child which shows their consciousness regarding the instruction given by the health service providers.
The majority of vaccinations took place at health posts and community hospitals. Similarly, nearly one-fifth (19.2%) of parents went to private clinics and some (17.5%) attended mobile/outreach clinics. The majority (89.2 %) had opted for immunising their child to prevent their children from diseases. Similarly, 19.2% said that reasons behind immunizing their child were the highly publicized campaign and their neighbours’ dedication to vaccinate their own child. Some respondents mentioned that they immunize their child because the immunisation is easily available.
The least common motivating factor was the fear of isolation created due to ignoring the immunisation campaign.
Attitude and Practice in Immunisation
Our studies found that 91.7%t of children were fully immunized. Only, 5.8% of respondents said that they were not satisfied with the immunisation of their child. Since three-quarters (76.7%) of children had been immunized on the recommended schedule, it suggests that the parents are aware of the importance of the immunisation schedule.
Factors Affecting Immunisation Knowledge & Practice
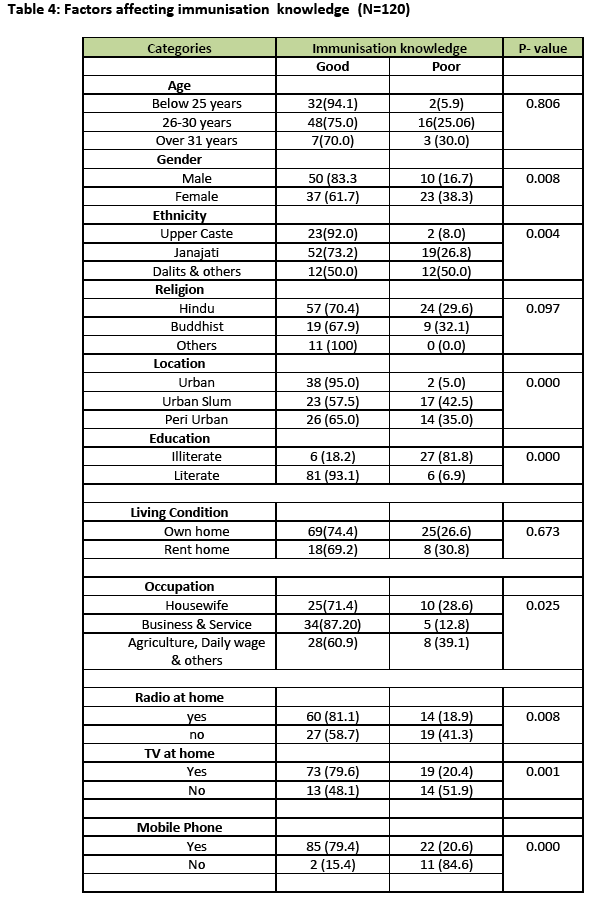
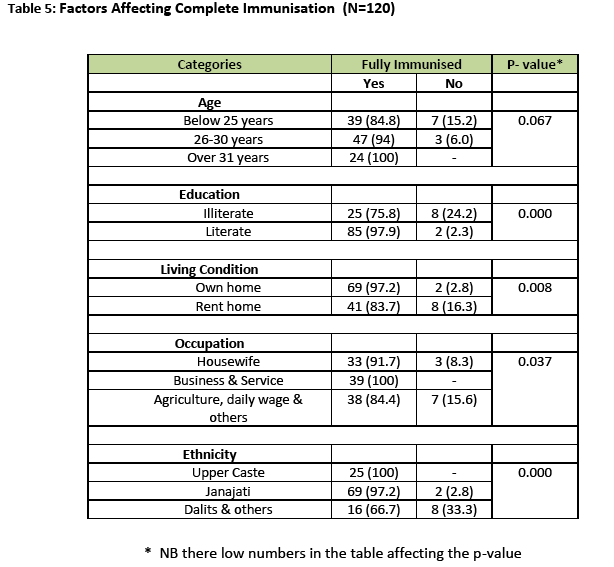
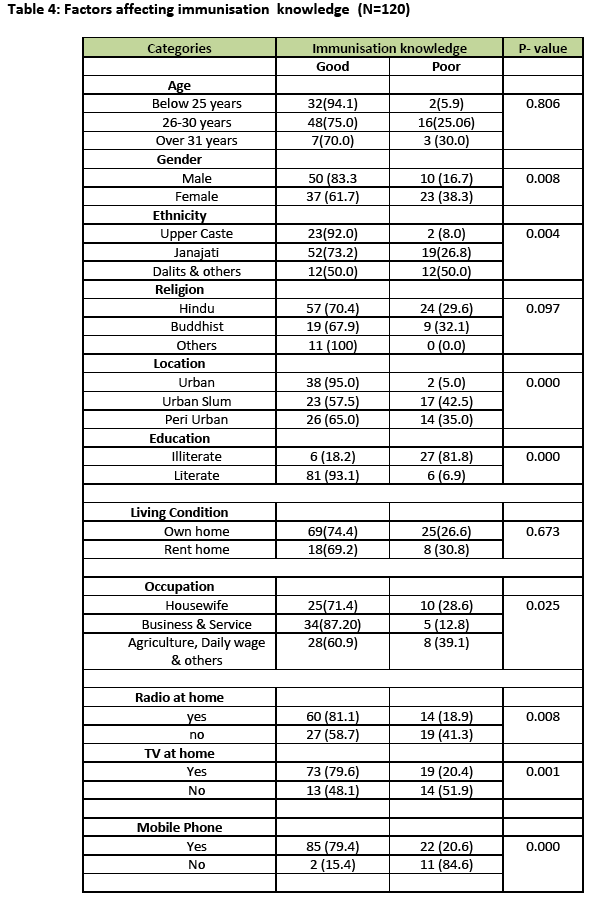
Gender, ethnicity, location, education level, occupation, having radio, TV and mobile phone at home were statistically significant factors (p<0.05) associated with knowledge level. Whilst age, religion and living in own home or rented home were not significant (Table 4).
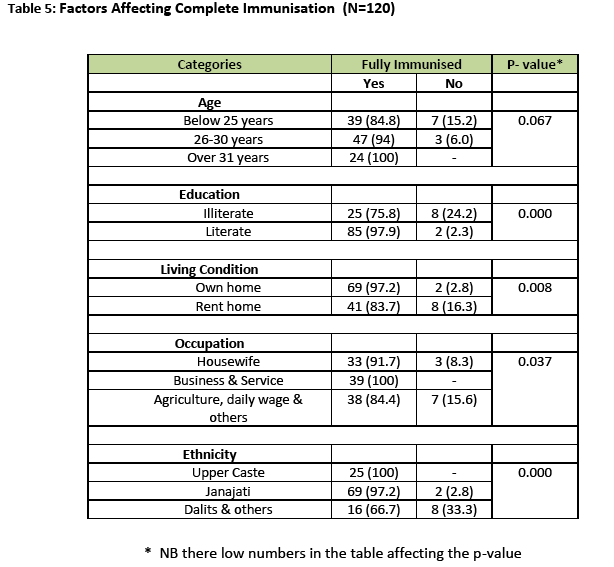
We also looked the practices of complete immunisation and the parents’ education and the different ethnicity group those parents belongs from. Illiteracy of parents was associated with non-completion of the immunisation schedule. Also children from the Dalit community were less likely to be fully immunisation those from upper caste and the Janajati community.
Moreover, younger parents were less likely to fully immunise their child than older parents. The people who lived in the rent home also are not immunising child completely.
Parents who are engaged in business and services were more likely to fully immunise their child compared to parents engaged in agriculture or on daily wages.
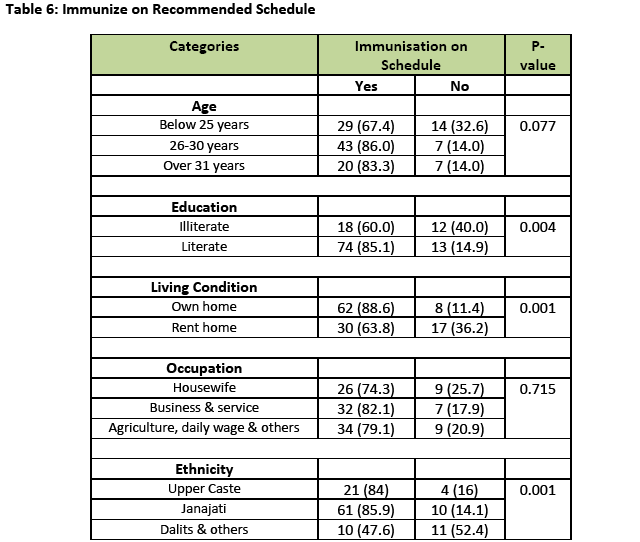
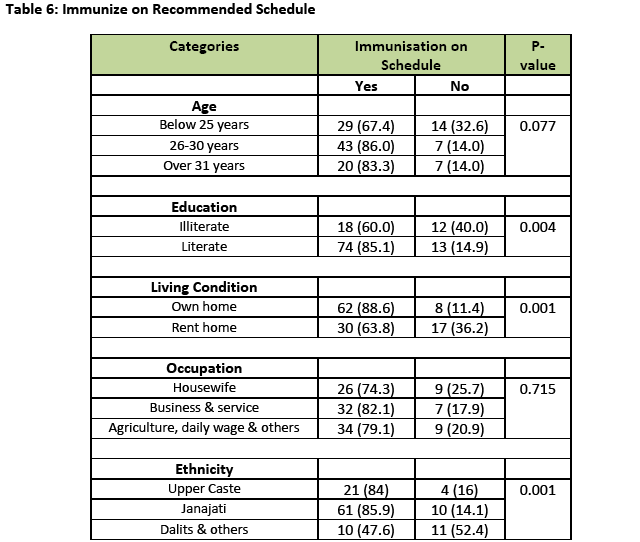
Table 6 shows the association between the socio-economic characteristics and immunisation on the recommended schedule; education, living condition and ethnicity were significantly associated. If the parents are literate, living at own home and from upper caste, the chances of immunising their child according to the recommended schedule was higher.
Discussion
Childhood immunisation rates were high in the study area. The Government of Nepal has been continuously promoted to use of mass media and interpersonal communication channels to enhance immunisation knowledge level in the population. There seems to be a considerable effects on target population as source of information and simultaneous in practice immunisation.
This study has shown that the majority of respondents’ source of information is local health workers, suggesting that people have relatively easy access health care facility in the study area, e.g. living in proximity to health services or frequently visiting health services. Surprisingly, though radio is portable, commonly owned and an easy medium to receive information, it has been placed in the third position in our study as a source of information. In contrast, the NDHS suggested that radio was the most effective source of information [23]. Similar to NDHS’ results, a study in Sunsari district revealed radio as the most effective source of information about the National Immunisation Day (NID) programme followed by health workers.
Health workers are the main source for immunisation in urban areas so, communication and education training to them need to be considered to improve their working with different strata of the population. A comprehensive communication strategy should be designed, regularly reviewed and updated. The strategic communication programme for different literacy level and ethnic group is must to reach the particular deprived group. As the radio jingles and TV spots were found as the most effective and understandable, this could help spread knowledge through broadcasts with regular intervals [24].
The study has found out that those who have immunized but not on recommended scheduled stand at 24%. Lack of correct understanding in the target population of the principle of the importance of the immunisation schedule challenges EPI communication planners. The existing policies are not concerned for strategic communication on this part.
Literacy goes hand-in-hand with health care practices. Here too the findings have clear association between immunisation practice and level of education of the parents. Same lacks as in the knowledge level. If the parents are illiterate the child has less chance to get fully immunized. Those, 24.2% of non-immunized child have the illiterate parents. As one of the Millennium Development Goals to achieve primary education access to all this will not only benefit the uptake of imminisation services but also all other aspect of health care and people’s lives in general [25].
Other finding of the study shows that the ethnic association with the practice of child immunisation rates also has diverse effects. Among non-immunized child, 33.3% their parents are from the Dalits community. The Nepalese government, as stated in its Three-Year Interim Plan (2007/2008 – 2009/2010) for special health programmes, already targets those most deprived including indigenous people (Adibasi Janajati), Dalits, people with disability and Madhesi people. Perhaps it is wise to also incorporate specific health communications for those deprived groups. So, the long-term communication support to EPI is the present need to face the prevailing challenge.
Even though the Nepalese seem to be well on the right track with regard to childhood immunisation, the dearth of systematic research on Nepalese parents’ knowledge and attitude about immunisation and their children’s health in relation to their immunisation behaviour not only suggests the importance of this particular study, but it also indicates how vital future research will be in furthering this story for generations to come.
2814
References
- Edwards KM. State mandates and Childhood Immunization. JAMA 2000; 284924); 3171-3173.
- World Bank, World Development Report 1993: Investing in Health; World Bank and Oxford Univ. Press, New York, 1993.
- Vittachi VT. The demand approach for the child survival and development revolution. Assignment Children 1984; 65/68: 13-20.
- Grant JP. State of the world's children 1987. New York: United Nations Children's Fund.
- Reman NS, Spencer EA, Sanson-Fisher RW. The role of mass media in changing health-related behaviour: a critical appraisal of two models; Health Promotion International 1990; 5 (1): 85-101.
- Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. The Lancet 2010; 376(9748): 1261?71.
- Griffiths W. The role of mass media in public health. American Journal of Public Health 1960; 50(4): 515-23.
- Hubley JH. AIDS in Africa: a challenge to health educators. Health Education Research 1988; 3(1): 41-47.
- Wallack LM. Mass media campaigns: the odds against finding behaviour change. Health Education Quarterly 1981; 8(3): 209-60.
- Narula U. Mass Communication; Theory and Practice, Har-An and Publications Pvt Ltd New Delhi, India 2003.
- WHO. The Ottawa Charter for Health Promotion; First International Conference on Health Promotion, Ottawa, 21 November 1986.
- Atkin C, Wallack L. (Eds.). Mass Communication and Public Health: Complexities and Conflicts. Newbury Park: Sage 1990.
- Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database of Systematic Reviews (Internet), 2002; (cited on 8 Nov 2012) 1. available from https://onlinelibrary.wiley.com/doi/10.1002/14651858.CD000389/pdf/standard.
- Wallack L, Dorfman L, Jernigan D, Themba, M. Media advocacy and public health: Power for prevention. Newbury Park: Sage 1993.
- Deer B. How the case against the MMR vaccine was fixed. British Medical Journal 2011; 342: 77-84.
- Wakefield AJ, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. The Lancet 1998; 351(9103): 637-41.
- Godlee F, Smith J, Marcovitch H. Wakefield's article linking MMR vaccine and autism was fraudulent. British Medical Journal 2011; 342: 64-66. 18. .
- New Era/Ministry of Health, Government of Nepal. Nepal Demographic Health Survey 2006. Kathmandu, Nepal.
- MoH. A Framework of Health Education, Information and Communication Program in Nepal, Kathmandu Nepal: Ministry of Health and Population; 2006.
- Waisbord S. Family Tree of Theories, Methodologies and Strategies in Development Communication: Convergences and Differences, New York: The Rockefeller Foundation; 2000.
- Bowling, A. Research methods in health: investigating health and health services. USA, Open University Press 2002.
- van Teijlingen E, Hundley V. The importance of pilot studies, Social Research Update 2001; Issue 35, (Edited by N. Gilbert), Guildford: University of Surrey.
- Jha N, Pokhrel S , Sehgal R. Awareness about a national immunisation day programme in the Sunsari district of Nepal. Bulletin of the World Health Organisation 1999; 77(7): 602-606.
- Devkota S, Simkhada P, van Teijlingen E, Rai LD. Media use for Health Promotion: Communicating Childhood Immunisation Messages to Parents. Health Promotion Journal of Nepal 2012;4(1)1-9.
- UN. The Millennium Development Goals Report 2012; United Nations, New York 2012.