Michael Promise Ogolodom1*, Lekpa Kingdom David2, Okechukwu Felix Erondu3, Mark Chukwudi Okeji4 and Awajimijan Nathaniel Mbaba5
1Rivers State Hospitals Management Board, Port Harcourt, Nigeria
2Department of Anatomy, University of Port Harcourt Rivers State, Nigeria
3Imaging Department of Image Diagnostics Ltd Port Harcourt, Rivers State, Nigeria
4Radiographers Registration Board of Nigeria Abuja, Nigeria
5Department of Radiology, Rivers State University Teaching Hospital, Port Harcourt, Nigeria
*Corresponding Author:
Michael Promise Ogolodom
Rivers State Hospitals Management Board, Port Harcourt, Nigeria
Tel: +234 (0) 80396979393
E-mail: mpos2007@yahoo.com
Received Date: November 27, 2018; Accepted Date: January 02, 2019; Published Date: January 09, 2019
Citation: Ogolodom MP, David LK, Erondu OF, Okeji MC, Mbaba AN (2019) Patterns of Traumatic Head Injury among Patients that Underwent Craniofacial Computed Tomography Scan in Port Harcourt Metropolis, Rivers State, Nigeria. Health Sci J Vol.13.No.1:615. DOI: 10.21767/1791-809X.1000615
Copyright: © 2019 Ogolodom MP, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Keywords
Traumatic head injury; Computed tomography; Port Harcourt
Introduction
Head injury is normally associated with trauma to the head (scalp, skull and brain). It is the commonest cause of mortality and morbidity in the global population, more frequently among those below 44 years of age [1-4]. In developed countries such as United State alone, head injury due to trauma account for over 40 billion dollars in cost of management yearly [1,5]. According to Tuong et al. [1], the causes of head trauma were normally related to the patient’s age. The National Center for Injury Prevention and Control had reported that approximately 2% of the entire population of the USA lives with disabilities associated with traumatic head injury (THI) and accounted for greater percentage of emergency department visits yearly [6,7].
In sub-Saharan African, there is higher rate of head injury conditions of the order of 150 to 170/100,000 which are associated with road traffic accident (RTAs) when compared to the world population rate of 106/100,000 [3,8]. The effects of head injury abnormalities due to trauma has become a major public health challenge, as it is the major leading cause of death in major cities including Port Harcourt Metropolis, Rivers State Nigeria. Port Harcourt is the administrative capital of Rivers State in the South-South geopolitical Zone of Nigeria with a population of over one Million people according to the 2006 National Population Census. The high population density of the city has tremendously contributed to the high prevalence of traumatic head injuries especially among young adults. Traumatic head injury had contributed about 31% of the total death associated with trauma in Nigeria [3,9]. According to Sutton [10], traumatic head injuries in the United Kingdom accounted for over 150,000 hospital admissions annually and 9 deaths per 1,00,000 people a year. Most victims of traumatic head injury normally ended up with some neurological disabilities due to the extensive effects of the trauma to mostly the neck region, thereby resulting to traumatic thrombosis, traumatic dissection, arteriovenous fistula, traumatic aneurysm and ruptured veins [10]. The effects of traumatic head injury can manifest in manifolds including late effects seen in cerebral atrophy, porencephalic cyst, cerebral infections, cerebrospinal fluid leak and hydrocephalus [1,10].
In diagnostic radiography, there are several imaging modalities usually adopted for the investigation of traumatic head injuries, but the choice of one modality over another depends on the following; the availability, speed of image acquisition, nature of the information to be obtained, age of the subject, as well as cost of the procedure [11-14]. Conventional X-ray of the head is still the crude and cheapest technique of evaluating head injury but due to superimposition of structures, its choice for traumatic head injury evaluation is limited [14-21]. In the case of babies with suspected perinatal trauma, head injuries can be evaluated with ultrasonography, although with some diagnostic limitations [10]. Magnetic resonance imaging (MRI) can also be used for the assessment of traumatic head injury especially if soft tissues are of major interest. Several researchers had recommended computed tomography (CT) as the gold standard in cases of traumatic head injury imaging despite its cost when compared with conventional x-ray and ultrasonography [1,3,10,14]. They reported the advantages of CT to be; shorter acquisition time when compared to MRI, availability, higher sensitivity in the detection of tiny skull fractures and in cases of intracranial bleeds. In addition CT suite allows the introduction of life-support gadgets such as oxygen cylinder and monitoring equipment. Adequate documentation of the patterns of traumatic head injury cases in major cities of Nigeria including Port Harcourt, would guide both the State and the Federal Governments on desired level preparedness to be attained in order to prevent and reduce mortalities associated with traumatic head injuries, hence this study. This study aimed at evaluating the patterns of traumatic head injuries (THI) in Port Harcourt Metropolis, common causes of the trauma in our locality, the age and sex distribution of the patients.
Materials and Methods
This is study adopted the retrospective survey design. Three private radio-diagnostic centers with CT scanners in Port Harcourt metropolis, Rivers State, Nigeria were enlisted into the study. Ethical approval was obtained from the Ethical Committees of the radio-diagnostic centers and the retrieved data were treated utmost confidentiality and used only for the purposes of this study. A total of 743 radiological images and reports of patients who underwent craniofacial CT scans in the three radio-diagnostics within the period of study (January 2010 to November 2017) were retrieved from their archives and studied. All the selected images were based on preselected inclusion criteria set for this study, such as presence of full identification parameters (age, sex, clinical indications, detailed diagnostic findings showing soft tissue and bony involvements. Images without the aforementioned criteria were excluded. All CT scan were performed on multi slice helical General Electric (GE) CT scanners with standard protocols and parameters (slice thickness 3-5 mm, slice Interval 3-5 mm, 80-120 kvp, 20-25 cm field of view, 200-300 mAs, 512 × 512 matrix size, window with 80 and window level 40 for brain tissues and window width 2500 and level of 500 for osseous structures, reconstruction algorithms (bone and Standard), Scan types; helical and axial scans) [1,3,13,22,23]. The choice of thin slice thickness was to enable the reformatting of the acquired axial images into sagittal and coronal planes to aid diagnosis.
Well-structured data capture sheets were used for data collection in the three centers. The obtained data were subjected to descriptive statistics and presented in tables and charts according to the objectives of this study. Data analyses were done using statistical package for social sciences (SPPS) version 20 (Chicago; Ilinosis, USA).
Results
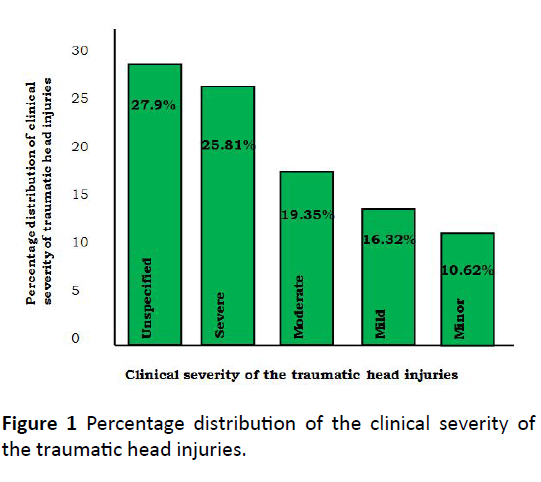
Of the 743 craniofacial CT images and reports evaluated, 482 (64.87%) had traumatic head injuries while 261 (35.13%) were non-traumatic head injuries and normal findings (Table 1). Out of the number of patients with traumatic head injuries, 302 were males (62.64%) and 180 were females (37.34%) giving a ratio of male to female as 1.7:1 (Table 1). Table 2 shows the age group distribution of sources of the trauma, with motor vehicle (road traffic accident) being the greatest contributor 43.3% followed by assault 31.53%. Out of 482 identified causes, age group 16-30 years was 34.03% (n=164). Among age group 16-30 years, motor vehicle (RTAs) account for 17.29% (n=83) (Table 2). Table 3 shows the nature of the injuries with the highest frequency being penetrating trauma mechanism (26.14%) and the least being closed trauma mechanisms 7.4%. Figure 1 shows the degree of the traumatic head injuries with “unspecified” being the most common 27.9% and closely followed by “Severe” 25.81% and “minor” 10.62% as the least. Both fractures and intra-axial lesions were the most common form of head injuries 23.24% (Table 4). Out of 23.24% intra-axial lesions, intracerebral hematomas were highest 12.30% followed by cortical contusions 5.81% (Table 4). In Table 4, subdural hemorrhage was highest 7.88% of the total 15.77% extra-axial lesions and the least was epidural 3.32%. Table 4 also shows the sex distribution of the forms of traumatic head injuries in this study, males had 10.20% extra-axial lessons while females had 5.57%. Intra-axial lesions 13.28% among males and females 9.99% out of the total of 23.24% cases of intra-axial lesions identified in this study.
Table 1 Sex frequency and percentage distribution of the incidence of the traumatic head injuries.
| Sex |
Frequency and percentage |
Total |
| THI (%) |
NTH 1+NF |
| Male |
302 (40.65) |
63 (21.93) |
465 (62.58) |
| Female |
180 (24.23) |
98 (13.19) |
278 (37.42) |
| Total |
482 (64.88) |
261 (35.12) |
743 (100) |
THI: Traumatic Head Injuries; NTHI+NF: Non-Traumatic Head Injuries+Normal Findings
Table 2 Age distribution of the causes of the traumatic head injuries.
| Age group (Yrs) |
Causes (Sources of Trauma) |
Total n (%) |
| MV |
AF |
A |
MS |
| 0-15 |
6 |
11 |
30 |
8 |
55 (11.41) |
| 16-30 |
83 |
3 |
63 |
15 |
164 (34.03) |
| 31-45 |
62 |
4 |
25 |
13 |
104 (21.58) |
| 46-60 |
40 |
10 |
15 |
2 |
67 (13.90) |
| 61 - 75 |
10 |
18 |
13 |
1 |
42 (8.71) |
| 76-90 |
8 |
32 |
6 |
4 |
50 (10.37) |
| Total |
209 |
78 |
152 |
43 |
482 (100) |
MV: Motor Vehicle (RTA); AF: Accidental Fall; A: Assult; Abuse; MS: Multiple Sources of traumatic head injuries.
Table 3 Frequency and percentage distribution based on the trauma mechanisms.
| Trauma mechanisms |
Frequency (n) |
Percentage (%) |
| Penetrating |
126 |
26.14 |
| Open |
92 |
19.09 |
| Blunt |
56 |
11.62 |
| Closed |
39 |
8.09 |
| Unspecified |
169 |
35.06 |
| Total |
482 |
100 |
Table 4 Sex frequency and percentage distributions of forms traumatic head injuries evaluated.
| Forms of traumatic head injuries |
Sex N (%) |
| Male |
Female |
Total |
| Extra-axial lesions |
49 |
27 |
76 (15.77) |
| Subarachnoid hemorrhage |
13 |
9 |
22 (4.56) |
| Subdural hemorrhage |
26 |
12 |
38 (7.88) |
| Epidural hemorrhage |
10 |
6 |
16 (3.32) |
| Intra-axial lesions |
64 |
48 |
112 (20.36) |
| Intracerebral hematomas |
31 |
27 |
58 (12.03) |
| Cortical contusions |
18 |
10 |
28 (5.81) |
| Axonal shearing injuries |
3 |
2 |
5 (1.04) |
| Gray matter injury |
7 |
5 |
12 (2.49) |
| Vascular injury |
5 |
4 |
9 (1.87) |
| Acute and sub-acute lesions |
32 |
23 |
55 (11.41) |
| Cerebral edema |
21 |
12 |
33 (6.85) |
| Ischemia |
8 |
6 |
14 (2.90) |
| Brain herniation |
3 |
5 |
8 (1.66) |
| Chronic lesions |
14 |
17 |
31 (6.43) |
| Cerebrospinal fluid(CSF) leak |
8 |
10 |
18 (3.73) |
| Hydrocephalus |
4 |
5 |
9 (1.87) |
| Encephalomalacia |
2 |
2 |
8 (0.83) |
| Fractures |
80 |
32 |
112 (23.24) |
| Simple |
34 |
11 |
45 (9.34) |
| Multiple |
46 |
21 |
67 (13.90) |
| Multiples injuries |
63 |
33 |
96 (19.91) |
| Total |
302 (62.66) |
180 (37.34) |
482 (100) |
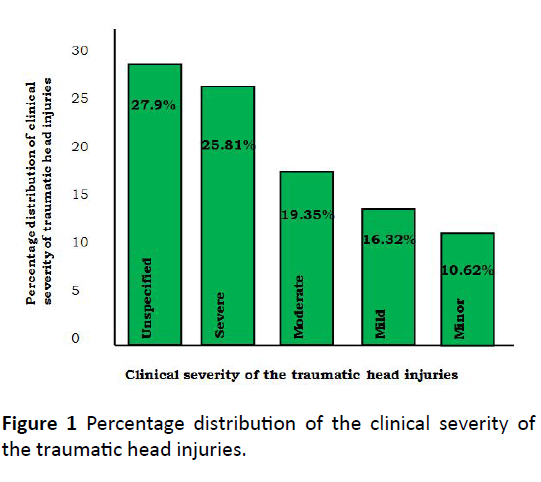
Figure 1: Percentage distribution of the clinical severity of the traumatic head injuries.
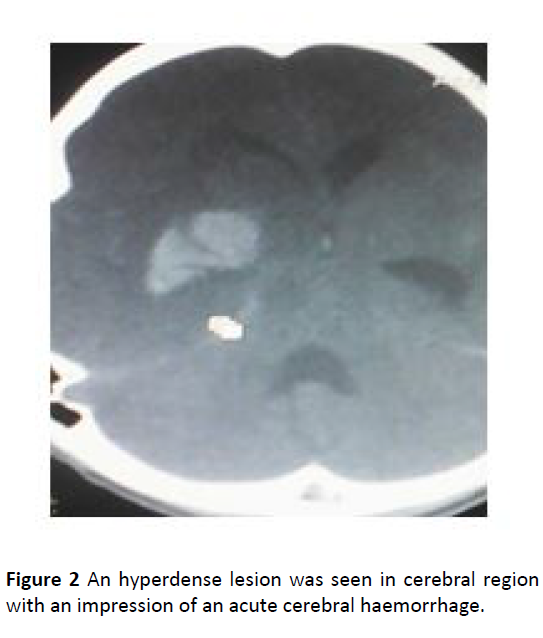
Fractures were found more in male population 16.70% (n=80) when compared to the female counterpart which is 6.54% (n=32) (Table 4 and Figures 2-5).
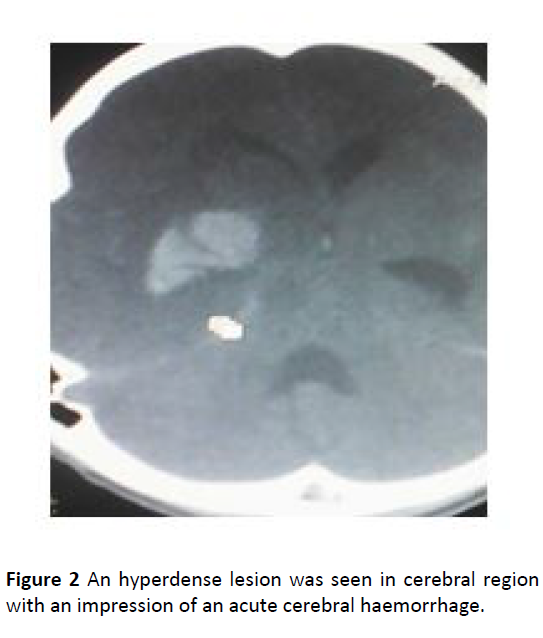
Figure 2: An hyperdense lesion was seen in cerebral region with an impression of an acute cerebral haemorrhage.
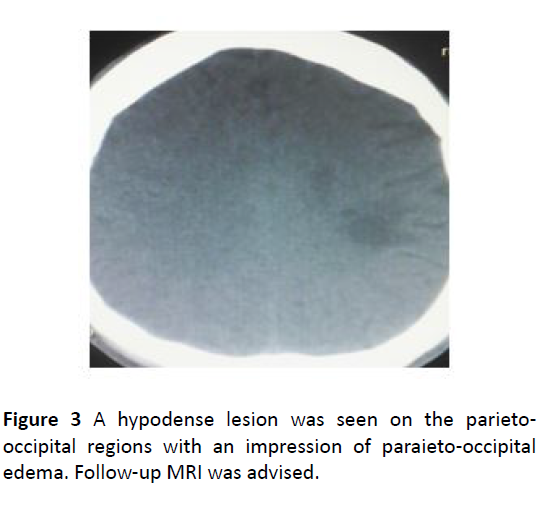
Figure 3: A hypodense lesion was seen on the parietooccipital regions with an impression of paraieto-occipital edema. Follow-up MRI was advised.

Figure 4: An ill-defined hypodense lesion with an average HU density of 20.5 HU is involving the paracentral lobule of the left frontal lobe. The lesion measures approximately 5.4 cm (AP) x 1.2 cm (Trans) x 3.0 cm (Long) in dimension and extends posteriorly into the parietal lobe. It shows no enhancement on post contrast scan with an impression of an acute left ischemic cerebral infarct in the territory of the peripheral branches of the left anterior cerebral artery.

Figure 5: Bone window images show depression with fracture of the right aspect of the frontal bone. There is associated hyperdensity of the brain parenchyma surrounding the aforementioned depressed skull bone with an impression of depressed skull fracture of the right aspect of the frontal bone with associated surrounding brain parenchymal changes.
Discussion
Majority (64.87%) of the head injury patients presenting for CT scan of the craniofacial region had traumatic head injuries. Our study showed fewer percentage of traumatic head injuries in Port Harcourt metropolis when compared with the study of Itanyi et al. [24] who reported 85.6% among pediatric patients with traumatic head injury in Abuja, Nigeria and Adekanmi et al. [25], who documented 77.6% among patients that underwent CT to evaluate the patterns of traumatic head injury at a tertiary hospital in Ibadan, South Western, However our study is in agreement with Ogunseyinde et al. [26] who reported 60.62% in Ibadan, South Western Nigeria and Onwuchekwa and Alazigha [3] who did their study in two tertiary hospitals in Niger Delta and reported 64.19%. The variation in values of our study and others may be due to differences in sample sizes used and geographical variations in relation to population density and traffic accidents.
The increase in the incident of traumatic head injuries has been attributed to the followings causes; bad road network with potholes, presence of commercial motorcyclists commonly known as “Okada” in some cities, military beset on civilians, cultism and militant activities especially in the Niger Delta region of Nigeria, including Port Harcourt Metropolis [3,26,27-32]. Although “Okada” commercial transportation had been implicated in major cities, our findings to that of Onwuchekwa and Alazigha [3] who reported military beset on civilians, cultism and militancy activities as major causes which are common in the Niger Delta region of Nigeria, including Port Harcourt Metropolis. This is because “Okada” transportation has been banned in Port Harcourt Metropolis by the Rivers State Government since 2009.
Our study found motor vehicles accident (RTAs) as the highest contributor to traumatic head injury in Port Harcourt metropolis. Our finding is similar to that of other researchers in developing countries including Nigeria [3,25,26,29,31,33,34]. According to Adekanmi et al. [25], out of 2142 cases of cranial CT scans enlisted in their study, 1318 cases were due to RTAs. The causes of RTA due to motor vehicles had been attributed to poor and bad road systems, inadequate motor vehicle maintenance, importation of substandard and used vehicles and tiers for both private and commercial transportation purposes. The utilization of alcohol and drugs, such as tramadol and marijuana, low levels of education, lack of eye test awareness among drivers in Nigerian have also contributed immensely to RTAs in our roads with resultant effect in traumatic head injuries in our localities [3,35-38].
Assault was the second commonest cause of trauma head injury identified in our study with over 30% of the cases. This is contrary to earlier studies by Adekanmi et al. [25] and Onwuchekwa and Alazigha [3]. Adekanmi et al. [25] reported assault as the least sources of trauma with only 6.3% in Ibadan, South-Western Nigeria while Onwuchekwa and Alazigha [3], documented 10% for assaults. The differences in values from our study could be attributed to geographical variations occasioned by cultural differences, difference in sample sizes employed as well as the nature of the study designs adopted.
The major trauma mechanism noted in our study was unspecified mechanisms which accounted for over 30% of the mechanisms evaluated. This is peculiar to our study, as majority of the other studies reviewed, do not captured data on the different trauma mechanisms.
With regard to clinical severity of traumatic head injuries, unspecified patterns of documentation was highly noted followed by severe and the least was minor patterns. According to Teasdale et al. [39], Tuong et al. [1], documentation clinical severity of traumatic head injury is usually graded using the Glasgow Coma Scale of minor: GCS≥15, Mild: GCS ≥ 13, Moderate: 9 ≥ GCS ≤ 12, Severe: 3 ≤ GCS ≤ 8. Based on these classifications and the appropriate documentations of minor, mild, moderate and severe patterns in our study, severe clinical presentation of traumatic head injuries was highest and the least was minor. This is consistent with the finding of similar study conducted in Abuja by Itanyi et al. [24] among children. This situation could be ascribed to the high cost of CT investigations in our locality which leaves CT as the last resort of investigation when others become equivocal.
High unspecified patterns of clinical severity documented in our study could be attributed to the different wavelength of knowledge of the Glasgow Coma Scale grading systems for severity of head injuries by some of the clinicians in private clinics. The most prevalent form of traumatic head injury identified in this study was fractures followed by primary injuries with subdural hemorrhage as the highest and the “secondary injuries” as least with acute and sub-acute injuries as highest when compared to the chronic form. Subdural and intra-cerebral hemorrhages were the most prevalent forms of extra-axial and intra-axial hemorrhages in our study. This is in agreement with Adekanmi et al. [25] who reported subdural hemorrhage as the highest (65.3%) of the extra-axial lesions while intra-axial hemorrhage was the highest form of intraaxial lesions (50.9%). Ashaleye et al. [28], Adeyekun et al. [27] and Onwuchekwa and Alazigha [3], equally reported subdural hemorrhage as the highest form of extra-axial lesions with 80%, 26.9% and 57.53% respectively. Ogunseyinde et al. [26] also reported similar findings where subdural and intra cerebral hemorrhages (28.7% and 26.3%) were the highest forms of extra-axial and intra-axial hematomas. However, our result is contrary that of Itanyi et al. [24] who documented contusion as the highest intracranial pathology. The differences in our findings could be attributed to the nature of subjects studied Itanyi et al. the sample size evaluated, geographical variations and the differences in the knowledge wavelength of the reporting radiologists [39-42].
Greater number of the traumatic head injuries evaluated in this study was within age groups 16-30 and 31-45 years of age. This shows that young adults were more prone to traumatic head injuries in our locality. This is in agreement with the result of Adekanmi et al. [25], Onwuchekwa and Alazigha [3], Ogunseyinde et al. [26] and Ashayele et al. [28]. It is however contrary to the findings of Itanyi et al. probably due to the studied population which were mainly children between the ages of 0-15 years. Adekanmi et al. [25] described this to the fact that young adults normally engage in travelling activities. Male populations were seen to be highly involved in the traumatic head injuries in our study when compared to their female counterpart. This finding is similar to the result of Adekanmi et al. [25] with 75.3% males and 24.7% females and ratio of 3:1. Coronado et al. [42] reported 2 times more frequent head injuries in male when compared to their female counterpart. Onwuchekwa and Alazigha [3] equally reported high number of traumatic head injuries among male. This could be attributed to more consumption of hard drugs among males, involvement in cultism and militancy activities and disobeying road traffic rules and regulations.
Conclusion
The incidence of traumatic head injuring in our study is high among those that underwent Craniofacial CT scans in Private Diagnostic Centers in Port Harcourt Metropolis. Fracture cases were highly noted with intra-axial lesions commonly documented when compared to the extra-axial lesions. Although “severe pattern” of traumatic head injuries was highly observed, majority of the cases were not classified using the Glasgow Coma Scales. Young adults were commonly affected with traumatic head injuries and male preponderance noted.
23951
References
- Tuong HL, Alisa DG (2006) Imaging of head trauma: seminar in rentgenology. JACR 51: 177-188.
- MacDorman MF, Minino AM, Strobino DM, Guyer B (2002) Annual Summary of Vital Statistics– 2001. Pediatrics 110: 1037-1052.
- Onwuchekwa CR, Alazigha NS (2017) Computed tomography patterns of traumatic head injury in Niger Delta, Nigeria: A mutticenter evaluation. Int J Crit llin Inj Sci 7: 150-155.
- Obajim MO, Jumah KB, Brakohuapa WO, Idrissu W (2002) Computed Tomography features of head injury in Ghanian children. Niger J Surg Res 4: 848.
- Lewin J, Summers D (1992) Anorexia due to brain injury. Brain Inj 6: 199-201.
- National Center for Injury Prevention and Control (2001) Injury Fact Book 2001-2002. Atlanta, GA: Centers for Disease Control and Prevention.
- Nirula R, Kaufman R, Tencer A (2003) Traumatic brain injury and automatic design: making motor vehicles safer. J Trauma 55: 844-848.
- Odero W, Garner J, Zwi A (1997) Road Traffic Injuries in developing countries: A comprehensive review of epidemiological studies. Trop Med Int Health 2: 445-450.
- Solagbem BA (2002) Spinal cord injuries in Ilorin Nigeria. West Afr JMed 21: 2030-2232.
- Sulton D (1995) Head injury and Trauma: In: David Sulton. Concise textbook of clinical imaging, pp: 745-820.
- Verma J, Tyagi S, Srivastava M, Agarwal A (2016) Computed tomography of paranasal sinuses for early diagnosis of nasal and sinus pathology. J Otorhinolaryngol Head Neck Surg 2: 70-71.
- Herman GT (2009) Fundamental of computerised tomography: image reconstruction from projection (2nd edn.). Springer pp: 234-249.
- Satish KB (2002) CT and MRI protocols: A practical approach (2nd edn.). PeeRee Publishers and Distributors (P)ltd. New Delhi, India. pp: 16-18.
- Ogolodom MP, Ugwu AC, Ohagwu CC, Eze C J, Obetta TC, et al. (2018) Patterns and prevalence of paranasal sinues diseases among patients referred for paranasal sinuses computed tomography in Port Harcourt, Rivers State, Nigeria. In J Med Health Res 4: 71-75.
- Bolger WE, Butazia CA, Parsons DS (1991) Paranasal Sinus bony anatomic variants and mucosal abnormalities: CT imaging analysis for endoscopy surgery. Larynoscope 101: 56-64.
- Bell RS, Loop JW (1971) The utility and futility of radiographic skull examination for trauma N Engl J Med 284: 236-259.
- Hackney DB (1991) Skull radiography in the evaluation of acute head trauma: a survey of current practice. Radiology 181: 711-714.
- Masters SJ (1980) Evaluation of head trauma: efficacy of skull films. AJR Am J Roentgenol 13: 539.
- Cure JK, Schabel S (1995) Sinuses: In: David Sulton editor. Concise textbook of clinical imaging. pp: 857-871.
- Stewart AW, Charles S, Graham H, Adrian DM, Chrissie WA (2005) Clark’s positioning in radiography (12th edn.), Hodder Headline Group, 338 Ebiston Road London NWI 3BH pp: 275-280.
- Brenner DJ, Hall EJ (2007) Computed Tomography: An increasing source of radiation exposure. North Engl JMed 357: 2277-2284.
- Halina S (1999) The Head: SinusesIn: Suzanne Henwood. Clinical CT Techniques and Practice, Cambridge University press, London. pp: 26-28.
- Sharm BN, Panta OB, Lohan B, Khanal U (2015) Computed tomography in the evaluation of pathological lesions of paranasal sinuses. J Nepal Health Res Couciling 13: 117.
- Itanyi UD, Yunusa KHO (2017) Computed tomography findings in pediatric traumatic head Injury in Abuja, Nigeria. Afr JMed Health Sci 16: 52-57.
- Adekanmi AJ, Adenniji-Sfoluwe AT, Obajimi MO (2015) Computed Tomography patterns of traumatic head injury at a tertiary hospital Ibadan, South-Western Nigeria: A 10 years review. Afr J of Trauma 4: 45-50.
- Ogunseyinde AO, Obajimi MO, Ogundare SM (1999) Radiological evaluation of head trauma by computer tomography in Ibadan, Nigeria. West Afri J Med 18: 33-38.
- Adeyekum AA, Ejakpovi OEB (2013) Computerized tomographic patterns in patients with head injury at the University of Benin Teaching Hospital. Niger J Clin Pract 16: 19-22.
- Ashaleye CM, Famurewa OC, Komolate EO, Komolate MA, Amusa YB (2005) The pattern of computerized tomographic findings in moderate and severe head injuries in the Ile Ife, Nigeria. West Afri J Radiol 12: 813.
- World Health Organization (2006) Neurological Disorders: Public Health challenges: Geneva, WHO. pp: 16473-16475.
- Reilly P (2007) The impact of neurotrauma on Society. An international perspective. In: Weber JT editors. Neurotrauma: New insights Pathology and Treatment. Amsterdam, Netherlands: Academic Press, pp: 5-7.
- World Health Organization (2011) Motorcycle Related Road traffic Crashes in Kenya facts and figures.
- Chalya PL, Mabula JB, Ngayomela IH, Ranumba ES, Chandika AB, et al. (2010) Motorcycle injuries as an emergency public health problem in Mwanza city, North Western Tanzania. Tanza J Health 12: 214-221.
- Akanji AO, Akinola RA, Balogun BO, Akano AO, Atalabi OM, et al. (2015) Computerized Tomography scan and head injury. The experience in a tertiary hospital in Nigeria. A cross-sectional study. Med Pract Rev 6: 1-15.
- Agrawal A, Galwankar, S, Kapi IV, Coronado V, Bassavaraju SV, et al. (2012) Epidemiology and clinical characteristics of traumatic brain injuries in a rural setting in Maharishi, India, 2007–2009. Int JCrit IIin InjSci 2: 167-1671.
- Adogu OC, Ilika Al (2006) Knowledge of and attitude towards road traffic codes among commercial motorcycle riders in Anambra State. Niger Postgrad Med 13: 297-300.
- Oladehine MK, Adeoye AO, Adegbehingbe BO, Onakoya AO (2007) Visual functions of commercial drivers in relation to road accidents in Nigeria. Indian J Occup Environ Med 11: 71-75.
- Iribhogbe PE, Odai ED (2009) Driver-related risk factors in commercial motorcycle (Okada) crashes in Benin City, Nigeria. Prehosp Disaster Med 24: 356-359.
- Adekoya BJ, Owoeye JE, Adepoju FG, Ajaiyeoba AI (2009) Visual Function survey of commercial intercity vehicle drivers in Ilorin, Nigeia. Can J Ophthalmol 44: 261-264.
- Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness: a practical scale: Lancet 13: 81-84.
- Sun Z, Nigh KH, Vijayananthan A (2010) Is utilization of computed tomography justified in Clinical practice? Part 1: Application in the emergency department. Singapore Med J 51: 200-206.
- Emejulu JK (2018) Epidemiological patterns of head injury in a newly established neurological service: one-year prospective study. Afri Med Med Sci 37: 383-388.
- Coronado Va, Xu L, Basavaraju SV, McGuire LC, Wald MM, et al. (2011) Surveillance for traumatic brain injury related deaths United States, 1997–2007. MMWR Surveill Summ 60: 1-3.